Abstract
The first majorly destructive pandemic of the twenty-first century broke out due to the spread of Severe Acute Respiratory Syndrome Coronavirus 2 worldwide. Remote management was put in place to efficiently assess the patients to prevent unnecessary hospitalization and educate the infected on the red flags. This study is a retrospective case control study that will contain a retrospective include analysis of medical records of 13,174 pediatric and adult patients with a laboratory-confirmed diagnosis of Coronavirus Disease and were undergoing remote management at REDMED online clinic in the period of July, 2021 and March, 2022. The retrieved data will be analyzed in specific detail and the hospitalization rate will be compared with country-wide results. The analysis helped us conclude, that there is a statistically significant difference between the country-wide hospitalization rate (16.8% by December 31, 2021 and 15.1% by July, 2022) and hospitalization rate (total mean value—1.8%) recorded at REDMED (×2 = 2123.488, df = 1, p < 0.0001 and ×2 = 1824.761, df = 1, p < 0.0001). This type of discrepancy requires further investigation. However, we have a reason to believe that direct communication with your doctor through an application might be the reason for being compliant and trusting the service provider. Well-managed and organized telemedicine is an efficient tool to manage Coronavirus or other Infectious Diseases remotely, especially when direct patient-to-doctor audiovisual communication is enabled..
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The first majorly destructive pandemic of the twenty-first century that broke out due to the spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-COV-2) worldwide and cast all countries into chaos, and despair, prompted fast adjustment to overcome this huge challenge [1,2,3]. Most of the countries responded with strict lockdowns, however, South Korea, which had a milder approach and civic involvement, is considered to be the most efficient. They utilized modern technologies, implemented milder restrictions, perfected identification, tacking and isolation of the infected [4,5,6]. The pandemic caused chaos in educational system as well and a lot of universities introduced remote studying, whilst some scientists and countries proposed hybrid teaching models to be implemented to find a middle ground between spread of the disease and maintaining the quality [7]. Whilst some countries totally restricted or prohibited various types of mass gatherings (political, recreational, religious etc.) some countries implemented specialized guidelines for such events, including using digital applications, COVID-19 vaccination status, social distancing, COVID-19 test results and so on [8,9,10]. Advent of new technologies and digital tools prompted researchers to study and analyze COVID-19 patterns, including patterns of spreading, which might be useful in management of the pandemic [11]. Telehealth and remote management had become interesting before the recent pandemic begun. For example, in the United States (US) patients can be monitored for high blood pressure, apnea, asthma and etc. [12,13,14] It is also widely used for management of various neurological conditions and might even be life-saving in certain conditions [15]. Therefore, in addition to a prompt response from scientists by starting to create either a drug to cure Coronavirus Disease (COVID-19) or an effective vaccine against SARS-COV-2, some countries implemented a hotline to communicate to their patients, whilst other countries together with existing hotline also gave permission for using existing telehealth platforms to manage the infected [12, 13, 16,17,18]. Remote management was put in place to make an efficient assessment of the patients to prevent unnecessary hospitalization and to educate the infected on what the red flags were [19, 20]. The country of Georgia initially responded heavy-handedly with a strict lock-down and did not start setting up state-governed call centers until a second wave hit the country [21]. These call centers could have been contacted though an emergency number 112 or 911. Later on, in July 2021 REDMED, which had been an up and running telemedical clinic by this time, started to provide service to SARS-COV-2 positive patients who had private insurance. Overall, 14,235 pediatric and adult patients were managed remotely in the period of July 2021 up to March, 2022. This retrospective study will provide the analysis of data collected from all those patients. Comparative analysis of variant-specific outcomes and presenting symptoms, variant-specific outcomes in vaccinated and unvaccinated adults, variant-specific characteristics in adult and pediatric populations will be presented and discussed. We understand that this grade of digitalization comes with the risks of its own, such as leakage of patients’ personal information, which is a huge concern. Jain et. al, for example, published a paper proposing ways to solve this problem and how to keep personal information protected [22].
2 Methods
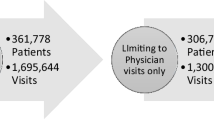
This study will include a retrospective review of medical records for 13,174 pediatric and adult patients with a laboratory-confirmed diagnosis of COVID-19 who were undergoing remote management at REDMED online clinic in the period of July, 2021 and March, 2022. REDMED in comparison to state-governed call centers comprised of personnel who had previous experience with telemedicine. The platform allows patients to use personal computers, laptops, pads or smartphones to get a remote consultation with a preffered specialist. The platform is based on Twilio engagement algorithm to help patient and doctor set-up a fast, encrypted and reliable communication with each other—via messaging, audio-only calls or video-calls, the communication between patient and doctor is available unless patient is already healthy and is “discharged” from the online clinic. Although, doctors had a specific work schedule, the communication through the system is available 24/7. Unlike other systems and algorithms, which include multiple steps such as schedulers, that might slow down the process [12, 13], in the case of REDMED, a patient can communicate to a specific service provider 24/7 via text message or requesting a call until the electronic medical record is active and the patients is not deemed healthy. REDMED is easy to set up and is available on all digital devices (Smart TV, smart phones, PC, laptops) with an access to the internet via application (REDMED for patients) or a web-page (www.redmed.ge). Remote management protocol includes communication with patients upon appearance in the system, gather anamnesis, inspect visually and give individual recommendations, educate them about respiratory and non-respiratory red flags of COVID-19 and follow-up calls every 2 days until the patient was considered healthy. Georgian national guidelines of COVID-19 management in this period were changing in accordance with the Center for Disease Control and Prevention of the United States (CDC). The hospitalization rate will be compared to the nationwide results presented by the NCDC. As per the data of 31st of December, 2021 Georgia had 934 741 laboratory-confirmed cases and 157 047 (16.8%) had been hospitalized and as per the data of July 1st, 2022 – 1 660 249 laboratory-confirmed cases and 250 113 (15.1%) had been hospitalized (Fig. 3). The report also states that over 30% of these hospitalizations were requested by the patients and did not have concrete medical grounds [23]. The study design is a retrospective case control study and aims to analyze the experience of REDMED online clinic and to compare the data with country-wide results in regards to hospitalization rate. The study was conducted at the facilities of REDMED online clinic. It was conducted in accordance with Helsinki Declaration, 1975 and REDMED institutional review board (IRB) approval (approval#RM-01-0422).
2.1 Statistical analysis
Statistical analysis will be executed utilizing Microsoft Excel and SPSS, we will be actively utilizing chi-squared test and comparison of proportions test.
3 Results
3.1 Dataset
This study will include information from 13,174 pediatric and adult patients who were undergoing remote management during SARS-COV-2 infection, the patients from January, 2022 will be excluded to better compare Delta and Omicron variant-specific details. Figure 1 shows the age distribution of the patients. Figure 2 shows distribution of vaccinated and unvaccinated patients.
For this study we also utilized data from 9th report of the National Center for Disease Control and Public Health (NCDC), to determine dates when one of the variants became dominant and to compare hospitalization rate of our study to the countrywide data (Fig. 3) [23].
3.2 Variant-specific separation
To compare Omicron and Delta variants we will follow the latest report of the NCDC [23], which includes periods when certain strains of SARS-COV-2 were dominant. Therefore, the study will include patients from July, 2021 up to January 1, 2022—when Delta variant was dominant (95% +)—and patients from February 1st, 2022 up to 1st of March, 2022—when Omicron was dominant (95% +).
3.3 Separation by age in adult Delta and adult Omicron groups
The adult patient group comprises all the patients who are 18 + years old. Additionally, to make a more meticulous comparison in regards to hospitalization following age sub-groups will be set: 18–34, 35–54, 55–65, 65 + .
The pediatric patient group will consist of all the patients who are 0–18 years old.
3.4 Study groups
Having established above-mentioned separation we will get the following groups: Adult Delta (adult patients who were infected when Delta variant was dominant), Adult Omicron (adult patients who were infected when Omicron variant was dominant), Pediatric Delta (pediatric patients who were infected when Delta variant was dominant), Pediatric Omicron (pediatric patients who were infected when Omicron variant was dominant).
Adult Delta will consist of 6306 patients; Adult Omicron will consist of 5833 patients; Pediatric Delta will consist of 235 patients; Pediatric Omicron will consist of 800 patients.
3.5 Adult delta group
Presenting symptoms at the onset in this group were as follows: fever (63.63%, 4013/6306), cough (32.72%, 2063/6306), catarrhal events, such as nasal discharge, throat ache etc. (21.81% 1376/6306), myalgia/arthralgia (16.36%, 1032/6306), headache (7.27%, 459/6306), nausea/vomiting (5.45%, 344/6306), diarrhea (3.63%, 229/6306), abdominal pain (1.81%, 114/6306). The number of asymptomatic patients with a laboratory-confirmed diagnosis of COVID-19 was as high as 23.63% (1490/6306) (Table 1).
Number of patients who were hospitalized was 157 (overall hospitalization rate 2.48%). As we mentioned, the adult groups were further subdivided into subsequent age sub-groups: 18–34 sub-group—1544 patients, 35–54 sub-group—2931 patients, 55–65 sub-group—1350 patients, 65 + sub-group—481 patients. Out of the patients who were admitted to a hospital 15 were from 18 to 34 sub-group (hospitalization rate 0.97%), 70 were from sub-group 35–54 (hospitalization rate 2.38%), 42 were from sub-group 55–65 (hospitalization rate 3.1%), 30 were from sub-group 65 + (hospitalization rate of 6.23%) (Table 2).
The leading reason for admission to the hospital was respiratory deterioration (130/157, 82.8%). The second most common reason was resistant fever (15/157, 9.5%), third reason was severe dehydration (12/157, 7.6%).
Mean fever resolution (axial temperature lower than 37.5 degrees Celsius without medication) day after disease onset in this group was 8 (Min.—1, Max.—19) (Fig. 4).
The number of vaccinated patients in this group was 306 (4.85%) and none of them were hospitalized.
No death was recorded in patients, while they were under remote care. No follow-up has been done after they were hospitalized.
3.6 Adult Omicron group
Presenting symptoms at the onset shifted in terms of prevalence and were as follows: fever (50.01%, 2917/5833), cough (41.23%, 2405/5833), catarrhal events (31.49% 1837/5833), headache (27.27%, 1590/5833), myalgia/arthralgia (12.98%, 757/5833), nausea/vomiting (11.68%, 681/5833), abdominal pain (11.36%, 662/5833), diarrhea (0.64%, 38/5833), conjunctivitis (0.61%, 35/5833). The number of asymptomatic patients with a laboratory-confirmed diagnosis of COVID-19 was as high as 23.05% (1344/5833) (Table 1).
Number of patients who were hospitalized was 52 (overall hospitalization rate 0.89%). As per sub-groups: 18–34 sub-group consisted of 1231 patients, 35–54 sub-group consisted of 2828 patients, 55–65 sub-group consisted of 1214 patients, 65 + sub-group consisted of 560 patients. Out of the patients who were admitted to a hospital 1 was from 18 to 34 sub-group (hospitalization rate 0.08%), 22 were from sub-group 35–54 (hospitalization rate 0.77%), 15 were from sub-group 55–65 (hospitalization rate 1.23%), 14 were from sub-group 65 + (hospitalization rate of 2.5%) (Table 2).
48 patients were admitted to the hospital due to respiratory deterioration, while 2 patients were admitted to the hospital due to severe dehydration and 2 patients due to acute severe chest pain.
Mean fever resolution day after disease onset in this group was 5 (Min.—2, Max.—17) (Fig. 4).
The number of vaccinated patients in this group was 571 (9.78%) and none of them were hospitalized.
No death was recorded in patients, while they were under remote care. No follow-up has been done after they were hospitalized.
3.7 Pediatric Delta group
Presenting symptoms at the onset in pediatric patients during delta domination was as follows: fever (53.3%, 125/235), catarrhal events (16.6% 39/235), headache (13.4%, 16/235), nausea/vomiting (10.2%, 24/235), myalgia/arthralgia (7.2%, 17/235), cough (6.5%, 15/235), abdominal pain (6.5%, 15/235), diarrhea (3.4%, 8/235), conjunctivitis (3.4%, 8/235). The number of asymptomatic patients with a laboratory-confirmed diagnosis of COVID-19 was as high as 30.2% (71/235) (Table 1).
The number of patients who were hospitalized was 12 (overall hospitalization rate 5.1%). The main reason for hospitalization was not made on clinical grounds, but on social grounds, and 7 out of 12 (58.3%) patients were hospitalized due to the inability of adequate management at home. The rest of the five children were hospitalized for the following reasons: resistant fever (1 patient), severe dehydration (1 patient), respiratory distress (1 patient), somnolence (1 patient), and possible multisystem inflammatory syndrome in children (MIS-C) (resistant fever plus Kawasaki disease (KD) signs) (1 patient). The majority of hospitalized children were below 8 years old. (Table 2).
Mean fever resolution day after disease onset in this group was 6 (Min.—1, Max.—25) (Fig. 5).
No vaccinated patient was in this group.
No death was recorded in patients, while they were under remote care. No follow-up has been done after they were hospitalized.
3.8 Pediatric Omicron group
Presenting symptoms at the onset in pediatric patients during delta domination was as follows: catarrhal events (55% 440/800), fever (37.62%, 301/800), cough (15%, 120/800), headache (13.87%, 111/800), abdominal pain (9.25%, 74/800), nausea/vomiting (8.25%, 66/800), myalgia/arthralgia (5%, 40/800), diarrhea (3%, 24/800), stridor (1.12%, 9/800). The number of asymptomatic patients with a laboratory-confirmed diagnosis of COVID-19 was as high as 19% (152/800) (Table 1).
The number of patients who were hospitalized was 11 (overall hospitalization rate 1.37%). The main reason for hospitalization similar to the Pediatric Delta Group was not made on clinical grounds, but on social grounds, and 6 out of 11 (54.5%) patients were hospitalized due to the inability of adequate management at home. 3 patients were hospitalized due to dehydration and 2 patients were hospitalized due to resistant fever. The majority of patients—8 children—were below the age of 6 (Table 2).
Mean fever resolution day after disease onset in this group was 3 (Min.—1, Max.—11) (Fig. 5).
4 vaccinated patients were in this group. None of them were hospitalized.
No death was recorded in patients, while they were under remote care. No follow-up has been done after they were hospitalized.
4.1 Comparative statistical analysis
The analysis helped us conclude that there is a statistically significant difference when comparing hospitalization rate against the age sub-groups, including the pediatric age group (×2 = 66.737, df = 4, p < 0.0001) (Table 2). There was also significant statistical difference in regards to study groups and hospitalization rate (× 2 = 59.997, df = 3, p < 0.0001). We found that there also is a statistically significant difference between countrywide hospitalization rate, recorded before December 31, 2021 and July 1, 2022, and hospitalization rate that was recorded at REDMED (× 2 = 2123.488, df = 1, p < 0.0001 and × 2 = 1824.761, df = 1, p < 0.0001) (Table 2). Another discovery we came over is that there is a statistically significant difference in hospitalization rate among vaccinated and unvaccinated patients (respectively, 0% vs 1.88%) (x2 = 15.634, df = 1, p = 0.0001). It has to be mentioned, though, that preventive potential of the vaccines slightly decreased, which is evident by significant statistical difference between number of vaccinated patients in Adult Omicron and Adult Delta Groups (respectively, 4.85% and 9.88%) (x2 = 113.756, df = 1, p < 0.0001).
5 Discussion
COVID-19 pandemic has challenged the modern world, however, it responded swiftly and the reality has changed. The success and trust that was gained by m-RNA and vector vaccines is extraordinary, which might change modern medicine [23,24,25,26]. The same has to be said about telemedicine, although it has some limitations, this method can be very useful against infectious diseases, especially reducing the risk of spreading and chances of healthcare system overload, as well as remote patient education [27,28,29]. We are sure that telemedicine will gain more ground in stroke management and other fields even faster than before 2020 [30].
Multiple matters can be observed when we analyze data that was collected during this study.
First of all, it is evident that Omicron spreads quicker, almost 4 times quicker among the adult population in the case of Georgia, which might also be attributed to a lower percentage of vaccination rate [23]. Just by looking at the group sizes Adult Delta size is almost the same size as Adult omicron size, however, the time frame is 6 months for the Adult Delta group, while for Adult Omicron it is 1 month.
In the case of the pediatric population, the Pediatric Omicron group size more than tripled the Pediatric Delta size, while the time frame is 6 times shorter for the Pediatric Omicron size. This kind of difference is very unusual according to the reported data [31,32,33,34,35,36,37,38]. That is why we tried to look into this matter very closely and we believe there are multiple reasons acting in tandem that helped the Omicron variant spread faster than usual. The first is that in November, 2021 all schools had to resume offline classes. Secondly, it is that vaccine coverage among the pediatric population is extremely low. The third is lower adherence to personal protective measures by children [25]. We believe that an amalgam of those factors played their role in infecting almost 3 times the amount in a timeframe that was 6 times smaller.
Second of all, it is clear that the Omicron variant has a milder course in both adult and pediatric populations. When we compare Adult Delta and Adult Omicron hospitalization rates, it is vivid that the overall hospitalization rate decreased almost 3 times (2.48% to 0.89%). Even if we look into individual age sub-groups: 18–34 sub-group—approximately 11 times less (0.97% vs 0.081%), 35–54 sub-group—approximately 3 times less (2.38% vs 0.77%), sub-group 55–65—approximately 3 times less (3.11% vs 1.23%), sub-group 65 +—approximately 2.5 times less (6.23% vs 2.5%).
COVID-19 in pediatric patients is well known to be significantly milder [39] and as we mentioned in the results section most of the hospitalizations were not decided on clinical grounds, but on social grounds. Regardless of this notion, we can clearly see a significant decrease in the admission rate in this population as well—5.1% vs 1.37%. So, basically, there was a massive decrease in hospitalization rate even though the Pediatric Delta group had 59% more asymptomatic patients than Pediatric Omicron (30.2% vs 19%).
In the Pediatric Omicron population, we had 9 patients who were older than 8 years and had presenting symptoms consistent with laryngotracheitis (stridor, barking cough, hoarseness), which responded well to oral dexamethasone and budesonide inhalation. It is an extremely rare event in this age group, however, there are case reports that such events were documented in adults as well [39, 40].
When we compare our hospitalization rate to the nationwide data reported by NCDC (Table 1, Fig. 3), the difference is so dramatic that this subject clearly needs more studying to detect what the reason for the hospitalization rate of up to 16.8% was. Our colleagues from Georgia report that the management of the pandemic was largely political and the country could have done better with a managerial body that did not have political bias [41]. We can deliberate that direct patient-to-doctor communication, rather than through a hotline, and the ability of audiovisual consultation, rather than a telephone call, facilitated by REDMED has affected those numbers. If we take into account that over 30% of the patients subjected themselves to hospitalization, the reliability and trust towards the service provider has to play a certain role [23]. However, the discrepancy is so huge that Georgian medical community will need to seriously study this subject to detect what the reason was: foul play, incompetence, or other objective reason(s).
Fever resolution in regard to symptom onset was faster in Adult Omicron and Pediatric Omicron groups—respectively, 5 and 3 days vs 8 and 6 days.
Regarding the vaccination status, the first thing we notice is that none of the vaccinated patients have been hospitalized, which is a good demonstration of the protection that it offers. The next thing that should be noticed is that though the preventive potential of vaccines has been diminished in regards to the Omicron variant, in both Adult Delta and Adult Omicron groups the absolute majority of patients were unvaccinated (95.15% vs 90.22%). It is hard to attribute this effect to a specific vaccine since the data we possess does not specify which shot has been given to which patient and Georgia has been distributing Sinopharm BBIBP, CoronaVac, VaxZevria and Cominarty vaccines.
6 Conclusion
In the end, we would like to conclude that despite the limitations Telemedicine might have, in the case of COVID-19 it indeed is an efficient tool to manage patients at home and prevent unnecessary overload of ambulatory and in-patient service, which by itself increases the risk for transmission. We think it would be wiser for governments to contact and utilize already established remote platforms, that already has certain experience in telemedicine. We would recommend that service providers offer direct patient-to-doctor audiovisual communication without any intermediary link, which might lead to better patient compliance and trust building. It should be also noted, that there was an increase in vaccinated patients in the Adult Omicron group, the absolute majority of the patients were unvaccinated and none of the patients required hospitalization which means that vaccines still offer solid protection.
Data availability
Data is not publicly available, however, upon reasonable request, any party will be granted access according to the Georgian legislature. The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tsang HF, Chan LWC, Cho WCS, Yu ACS, Yim AKY, Chan AKC, Ng LPW, Wong YKE, Pei XM, Li MJW, Wong SC. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther. 2021;19(7):877–88.
Kaul V, Gallo de Moraes A, Khateeb D, Greenstein Y, Winter G, Chae J, Stewart NH, Qadir N, Dangayach NS. Medical education during the COVID-19 pandemic. Chest. 2021;159(5):1949–60.
Khan M, Adil SF, Alkhathlan HZ, Tahir MN, Saif S, Khan M, Khan ST. COVID-19: a global challenge with old history, epidemiology and progress so far. Molecules. 2020;26(1):39.
Haider N, Osman AY, Gadzekpo A, Akipede GO, Asogun D, Ansumana R, Lessells RJ, Khan P, Hamid MMA, Yeboah-Manu D, Mboera L, Shayo EH, Mmbaga BT, Urassa M, Musoke D, Kapata N, Ferrand RA, Kapata PC, Stigler F, Czypionka T, McCoy D. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob Health. 2020;5(10):e003319.
Du J, Mayer G, Hummel S, Oetjen N, Gronewold N, Zafar A, Schultz JH. Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: cross-sectional survey study. J Med Internet Res. 2020;22(12): e24240.
Lee D, Heo K, Seo Y. COVID-19 in South Korea: lessons for developing countries. World Dev. 2020;135: 105057.
Bardesi H, Al-Mashaikhi A, Basahel A, Yamin M. COVID-19 compliant and cost effective teaching model for King Abdulaziz University. Int J Inf Technol. 2021;13(4):1343–56.
Basahel S, Alsabban A, Yamin M. Hajj and Umrah management during COVID-19. Int J Inf Technol. 2021;13(6):2491–5.
https://www.getreading.co.uk/news/reading-berkshire-news/easter-2021-lockdown-rules-how-20295398
Alafif T, Etaiwi A, Hawsawi Y, Alrefaei A, Albassam A, Althobaiti H. DISCOVID: discovering patterns of COVID-19 infection from recovered patients: a case study in Saudi Arabia. Int J Inf Technol. 2022;14(6):2825–38. https://doi.org/10.1007/s41870-022-00973-2.
https://www.aafp.org/pubs/fpm/blogs/inpractice/entry/telehealth_algorithm.html
Jessica Spiegelman, Nicole Krenitsky and Sbaa Syeda et al. Rapid Development and Implementation of a Covid-19 Telehealth Clinic for Obstetric Patients. Nejm Catalyst Innovations in Care Delivery. 2020.
Chirra M, Marsili L, Wattley L, Sokol LL, Keeling E, Maule S, Sobrero G, Artusi CA, Romagnolo A, Zibetti M, Lopiano L, Espay AJ, Obeidat AZ, Merola A. Telemedicine in Neurological Disorders: Opportunities and Challenges. Telemed J e-Health. 2019;25(7):541–50.
Mahajan V, Singh T, Azad C. Using telemedicine during the COVID-19 pandemic. Indian Pediatr. 2020;57(7):652–7.
Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health. 2020;11:2150132720980612.
Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2): e18810.
García-Azorín D, Trigo J, Talavera B, Martínez-Pías E, Sierra Á, Porta-Etessam J, Arenillas JF, Guerrero ÁL. Frequency and type of red flags in patients with Covid-19 and headache: a series of 104 hospitalized patients. Headache. 2020;60(8):1664–72.
Madani S, Shahin S, Yoosefi M, Ahmadi N, Ghasemi E, Koolaji S, Mohammadi E, Mohammadi Fateh S, Hajebi A, Kazemi A, Pakatchian E, Rezaei N, Jamshidi H, Larijani B, Farzadfar F. Red flags of poor prognosis in pediatric cases of COVID-19: the first 6610 hospitalized children in Iran. BMC Pediatr. 2021;21(1):563. https://doi.org/10.1186/s12887-021-03030-2.
Covid-19 legislative acts: https://www.ncdc.ge/#/pages/content/22788fbb-ea55-4de5-b2e7-d73ec6323af6
Jain S, Doriya R. Security framework to healthcare robots for secure sharing of healthcare data from cloud. Int J Inf Technol. 2022;14(5):2429–39.
COVID-19 Report of the National Center for Disease Control and Public Health 2020–2022 REPORT The 9th Revision: http://test.ncdc.ge/Handlers/GetFile.ashx?ID=d10ffd42-c682-4dba-bffd-21ec38c7db5d
Liu S, Jiang Q, Zhao X, Zhao R, Wang Y, Wang Y, Liu J, Shang Y, Zhao S, Wu T, Zhang Y, Nie G, Ding B. A DNA nanodevice-based vaccine for cancer immunotherapy. Nat Mater. 2021;20(3):421–30.
Li S, Jiang Q, Liu S, Zhang Y, Tian Y, Song C, Wang J, Zou Y, Anderson GJ, Han JY, Chang Y, Liu Y, Zhang C, Chen L, Zhou G, Nie G, Yan H, Ding B, Zhao Y. A DNA nanorobot functions as a cancer therapeutic in response to a molecular trigger in vivo. Nat Biotechnol. 2018;36(3):258–64.
Morse MA, Gwin WR 3rd, Mitchell DA. Vaccine therapies for cancer: then and now. Target Oncol. 2021;16(2):121–52.
Morante V, Borghi M, Farina I, Michelini Z, Grasso F, Gallinaro A, Cecchetti S, Di Virgilio A, Canitano A, Pirillo MF, Bona R, Cara A, Negri D. Integrase-defective lentiviral vector is an efficient vaccine platform for cancer immunotherapy. Viruses. 2021;13(2):355.
Lukas H, Xu C, Yu Y, Gao W. Emerging telemedicine tools for remote COVID-19 diagnosis, monitoring, and management. ACS Nano. 2020;14(12):16180–93.
Colbert GB, Venegas-Vera AV, Lerma EV. Utility of telemedicine in the COVID-19 era. Rev Cardiovasc Med. 2020;21(4):583–7.
Garattini L, Badinella Martini M, Zanetti M. More room for telemedicine after COVID-19: lessons for primary care? Eur J Health Econ. 2021;22(2):183–6.
Araf Y, Akter F, Tang YD, Fatemi R, Parvez MSA, Zheng C, Hossain MG. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J Med Virol. 2022;94(5):1825–32.
Chenchula S, Karunakaran P, Sharma S, Chavan M. Current evidence on efficacy of COVID-19 booster dose vaccination against the Omicron variant: a systematic review. J Med Virol. 2022;94(7):2969–76.
Scott L, Hsiao NY, Moyo S, Singh L, Tegally H, Dor G, Maes P, Pybus OG, Kraemer MUG, Semenova E, Bhatt S, Flaxman S, Faria NR, de Oliveira T. Track Omicron’s spread with molecular data. Science. 2021;374(6574):1454–5.
Thakur V, Ratho RK. OMICRON (B.1.1.529): a new SARS-CoV-2 variant of concern mounting worldwide fear. J Med Virol. 2022;94(5):1821–4.
CDC COVID-19 Response Team (2021). SARS-CoV-2 B.1.1.529 (Omicron) Variant - United States, December 1–8. MMWR Morb Mortal Wkly Rep. 2021;70(50):1731–4.
Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In StatPearls: StatPearls Publishing; 2023.
Meo SA, Meo AS, Al-Jassir FF, Klonoff DC. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci. 2021;25(24):8012–8.
Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021;50(1):44–57.
Kamidani S, Rostad CA, Anderson EJ. COVID-19 vaccine development: a pediatric perspective. Curr Opin Pediatr. 2021;33(1):144–51.
Alhedaithy AA, Murad IS, Aldabal N. Acute laryngotracheitis caused by COVID-19: a case report and literature review. Int J Surg Case Rep. 2022;94: 107074.
Kamali Aghdam M, Shabani Mirzaee H, Eftekhari K. Croup is one of the clinical manifestations of novel coronavirus in children. Case Rep Pulmonol. 2021;2021:8877182.
Nadareishvili I, Zhulina A, Tskitishvili A. The approach to the COVID-19 pandemic in Georgia—A health policy analysis. Int J Public Health. 2022;67:10.
Acknowledgements
We would love to thank every doctor who took part in battling COVID-19, especially our colleagues at REDMED who were actively communicating with patients: Irina Fichkhadze, MD, Thea Shengelia, MD, Shorena Meunargia, MD, Keti Tsertsvadze, MD and etc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
No financial assistance was received to support the study.
Author information
Authors and Affiliations
Contributions
All authors are responsible for the work described in this paper. All authors were involved in at least one of the following: [conception, design of work or acquisition, analysis, interpretation of data] and [drafting the manuscript and/or revising/reviewing the manuscript for important intellectual content]. All authors provided final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Patient consent
Patients’ consent was not required to perform the retrospective study, since upon admission all the patients had already given informed consent which already includes an article about the retrospective review of the medical records without disclosing patients’ identities and personal information, which is a criminal offense in the Republic of Georgia.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chakhunashvili, K., Chakhunashvili, D.G., Kvirkvelia, E. et al. Comparative analysis of a private telehealth clinic and country-wide COVID-19 patient management results. Discov Health Systems 2, 22 (2023). https://doi.org/10.1007/s44250-023-00036-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44250-023-00036-8