Summary
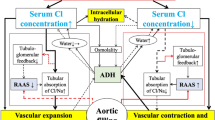
To investigate the influence of critical illness on plasma renin activity and aldosterone levels and to examine potential inhibitory effects of dopamine therapy on aldosterone responsiveness, we measured plasma renin activity, and potassium and creatinine in serum, as well as the responses of aldosterone, cortisol and prolactin levels to TRH 200 µg i.v. + Synacthen 0.25 mg i.v. in 63 unselected, critically ill patients (32 females, 31 males, aged 18–84 years). Of the patients 19 received dopamine treatment (3–13 µg/kg/min i.v.); 21 of the patients died in the further course of their disease. Plasma renin activity was increased in 66.7% of the patients and aldosterone levels were elevated in 90.5% of the patients. There were correlations (P<0.05) of lethality with plasma renin activity and cortisol levels and correlations (P<0.01) of aldosterone concentrations with plasma renin activity and cortisol levels. Whereas dopamine treatment had no inhibitory effect on aldosterone levels before and after stimulation, prolactin stimulation was decreased in dopamine-treated patients.
Thus, dopamine does not generally lose its potency of hormone inhibition in critically ill patients, but has no influence on the secondary aldosteronism developing regularly in the early phase of critical illness, which is apparently mainly due to the stimulatory effect of ACTH (or ACTH-related pituitary peptides) and is considered an epiphenomen of the stress mechanisms acting upon the patients in this condition.
Similar content being viewed by others
Abbreviations
- ACTH:
-
Adrenocorticotropes Hormon
- TRH:
-
Thyreotropin-Releasing Hormon
- ZNS:
-
Zentrales Nervensystem
Literatur
Abboud FM (1979) Shock. In: Beeson PB, McDermott W, Wyngaarden JB (Hrsg) Textbook of Medicine. WB Saunders, London Toronto Philadelphia
Aguilera G, Fujita K, Catt KJ (1981) Mechanisms of inhibition of aldosterone secretion by adrenocorticotropin. Endocrinology 108:522–528
Aguilera G, Mendelsohn FAO, Catt KJ (1984) Dopaminergic regulation of aldosterone secretion. Frontiers in Neuroendocrinology 8:265–293
Allolio B, Stuttmann R, Fischer H, Leonhard W, Winkelmann W (1983) Long-term etomidate and adrenocortical suppression. Lancet 2:626
Bailey RR, Abernethy MH, Beaven DW (1967) Adrenocortical response to the stress of an acute myocardial infarction. Lancet 1:970–973
Dresel M, Falke W (1984) Der Verlauf der Plasmakatecholamine Noradrenalin und Adrenalin beim akuten Myokardinfarkt. Beziehung zu Hämodynamik, Infarktgröße und ventrikulärer Extrasystolie. Inauguraldissertation, Frankfurt am Main
Finlay WEI, McKee JI (1982) Serum cortisol levels in severely stressed patients. Lancet 1:1414–1415
Gillis G, Grossmann A (1985) The CRFs and their control: Chemistry, Physiology and clinical implications. Clin Endocrinol Metab 14:821–844
Goldberg LI (1974) Dopamine — clinical use of an endogenous catecholamine. N Engl J Med 291:707–710
Gordon MB, Moore TJ, Dluhy RG, Williams GH (1983) Dopaminergic modulation of aldosterone responsiveness to angiotensin II with changes in sodium intake. J Clin Endocrinol Metab 56:340–345
Heimburg P (1984) Herzinsuffizienz. In: Hornbostel H, Kaufmann W, Siegenthaler W (Hrsg) Innere Medizin in Praxis und Klinik, Band I. G Thieme, Stuttgart New York
Husband DJ, Alberti KGMM, Julian DG (1983) “Stress” hyperglycaemia during acute myocardial infarction: An indicator of preexisting diabetes? Lancet 2:179–181
Jungmann E (1985) Untersuchungen zur endogenen dopaminergen Regulation der Aldosteronsekretion. Habilitationsschrift, Frankfurt am Main
Jungmann E, Wächtler M, Schwedes U, Usadel KH, Schöffling K (1985) The dopaminergic control of aldosterone secretion. In: Mantero F, Biglieri EG, Funder JW, Scoggins BA (Hrsg) The adrenal gland and hypertension. Raven Press, New York
Jungmann E, Schifferdecker E, Althoff PH (1986) Das Syndrom des hyperreninämischen Hypoaldosteronismus beim kritisch kranken Patienten. Med Klin (im Druck)
Kahana L, Keidar S, Sheinfeld M, Palant A (1983) Endogenous cortisol and thyroid hormone levels in patients with acute myocardial infarction. Clin Endocrinol 19:131–139
Kallner G, Ljunggren JG (1979) The role of endogenous cortisol in patients with non-thyroidal illness and decreased T3 levels. Acta Med Scand 206:459–461
Kojima K, Ogata A (1982) Reversal by a dopamine antagonist of saline-induced attenuation of aldosterone response to angiotensin II infusion in man. Endocrinol Japon 29:21–25
Ledingham IM, Watt I (1983) Influence of sedation on mortality in critically ill multiple trauma patients. Lancet 1:1270
Ledingham IM, Finlay WEI, Watt I, McKee JI (1983) Etomidate and adrenocortical function. Lancet 1:1434
Logan RW, Murdoch WR (1966) Blood-levels of hydrocortisone, transaminases, and cholesterol after myocardial infarction. Lancet 2:521–524
Long WM, Pons GM, Sprung CL (1985) Metabolic and hormonal responses to injury and sepsis in the critically ill. In: Geelhoed GW, Chernow B (Hrsg) Endocrine Aspects of acute illness. Churchill Livingstone, New York Edinburgh London Melbourne
Luger A, Graf H, Prager R, Sturmvoll HK (1984) Alterations in the renin-angiotensin-aldosterone system in the critically ill. Horm Metab Res 16:213–214
McKee JI, Finlay WEI (1983) Cortisol replacement in severely stressed patients. Lancet I:484
McLees BD (1979) Critical Care Medicine. In: Beeson PB, McDermott W, Wyngaarden JB (Hrsg) Textbook of Medicine. WB Saunders, Philadelphia London Toronto
Madias NE, Harrington JT (1983) Postischemic acute renal failure. In: Brenner BM, Lazarus JM (Hrsg) Acute renal failure. WB Saunders, Philadelphia London Toronto
Oelkers W (1985) Prolonged ACTH infusion suppresses aldosterone secretion in spite of high renin activity. Acta endocrinol 108:91–97
Sachs L (1978) Angewandte Statistik. Springer, Berlin Heidelberg New York
Sainsbury JRC, Stoddart JC, Watson MJ (1981) Plasma cortisol levels. Anaesthesia 36:16–21
Schifferdecker E, Schulz F, Althoff PH, Schöffling K (1984) Pathologische Schilddrüsenfunktionswerte bei schweren nichtthyreoidalen Erkrankungen. Intern Prax 24:481–491
Schröder R (1975) Dopamin. FK Schattauer, Stuttgart New York
Schwartau M, Bücking J (1984) Zur Bedeutung des sekundären Hyperaldosteronismus in der internistischen Intensivmedizin. Intensivmed 21:19–22
Stoeckel H, Korpassy A (1982) Das Verhalten der Aldosteronexkretion und Hydrocortisonexkretion bei prolongiertem Streß und Langzeitbeatmung. Z prakt Anästh 7:28–37
Witzgall H, Weber PC (1983) Der Angiotensin II-induzierte Anstieg von Aldosteron und 18-OH-Kortikosteron bei Patienten mit essentieller Hypertonie und beim idiopathischen Hyperaldosteronismus wird durch Dopamin reduziert. Verh Dtsch Ges Inn Med 89:1443–1446
Zipser RD, Davenport MW, Martin KL, Tuck ML, Warner NE, Swinney RR, Davis CL, Horton B (1981) Hyperreninaemic hypoaldosteronism in the critically ill: A new entity. J Clin Endocrinol Metab 53:867–873
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jungmann, E., Schifferdecker, E., Rümelin, A. et al. Plasma Renin Aktivität und Aldosteronverhalten bei kritisch kranken Patienten. Klin Wochenschr 65, 87–91 (1987). https://doi.org/10.1007/BF01745482
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01745482