Abstract
A dual control system for assisting respiration was developed. The following features were included: (i) ventilation is controlled by the metabolic rate from continuously measured CO2 output, (ii) physiologic dead space approximated as a linear function of tidal volume is used to estimate alveolar ventilation, and (iii) oxygen concentration in the inspired gas is regulated by the arterial oxygen saturation continuously measured with an ear oximeter.
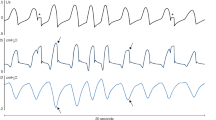
The ventilator was used on dogs with an inspired gas mixture of 85% N2 and 15% O2. Arterial Pco2 was maintained between 36 and 39 mmHg for a duration exceeding 60 minutes. Although an oscillatory variation was seen in the arterial Po2 due to the adoption of an on-off control mode to regulate the O2 fraction in the inspired gas, it remained between 80 and 136 mmHg.
The dual control system of assisting respiration is capable of maintaining both the arterial Pco2 and Po2 within normal levels at any level of metabolic rate and any respiratory frequency.
Sommaire
On a développé un système à contrôle double pour aider la respiration. Il comprend les traits suivants: (i) La ventilation est contrôlée par le taux métabolique à partir de la mesure en continu du rendement en CO2, (ii) L'espace physiologique mort, calculé en tant que fonction linéaire du volume d'air de respiration, sert à estimer la ventilation alvéolaire et (iii) la concentration d'oxygène dans le gaz inspiré est réglée par la saturation artérielle d'oxygène mesurée en continu à l'aide d'un oxymètre placé dans l'oreille.
Le ventilateur fut utilisé sur des chiens avec un mélange de gaz inspiré contenant 85% de N2 et 15% de CO2. La pression artérielle de CO2 fut maintenue entre 36 et 39 mm de Hg pendant une durée supérieure à 60 minutes. Bien qu'une variation oscillatoire de la pression artérielle en O2, causée par l'adoption d'un mode de contrôle marche-arrêt servant à régler la fraction de O2 dans le gaz inspiré fut observée, celle-ci demeura entre 80 et 135 mm de Hg.
Le système à contrôle double d'aide respiratoire est capable de maintenir à la fois la pression artérielle de CO2 et de O2 dans des limites normales pour tout taux métabolique et toute fréquence respiratoire.
Zusammenfassung
Es wurde ein doppeltes Regelsystem als Atmungshilfe entwickelt das folgende Merkmale aufweist: 1) die Atemluft wird durch die Stoffwechselgeschwindigkeit aus der ständig gemessenen CO2-Leistung geregelt, 2) der physiologisch tote Raum, der als lineare Funktion des Atemvolumens im Näherungsverfahren bestimmt wurde, wird zur Beurteilung der Alveolen-Ventilation verwendet und 3) die Sauerstoffkonzentration im eingeatmeten Gas wird durch die arterielle Sauerstoffsättigung reguliert, die ständig mit einem Sauerstoffmesser im Ohr gemessen wird.
Das unterstützende Atemgerät wurde an Hunden mit einem Mischgas aus 85% N2 und 15% O2 eingesetzt. Der arterielle PCO2-Druck wurde für eine Dauer von höchstens 60 Minuten bei 36 und 39 mm HG gehalten. Obgleich im arteriellen PO2 eine Schwingungsänderung entstand, da man zur Regulierung der O2-Fraktion im eingeatmeten Gas eine Ein-/Ausschaltung verwendete, blieb er zwischen 80 und 135 mm Hg.
Aus den vorstehenden Ergebnissen läßt sich ersehen, daß das Doppelregelsystem bei der Atmungshilfe einen arteriellen PCO2 und PO2 in normaler Höhe bei jeder Stoffwechselgeschwindigkeit und Atmungsfrequenz beibehalten kann.
Similar content being viewed by others
References
Askrog, V. (1966) Changes in (a-A) CO2 difference and pulmonary pressure in anesthetized man.J. Appl. Physiol.21, 1299–1305.
Bean, J. W. (1945) Effects of oxygen at increased pressure.Physiol. Rev.25, 1–147.
Brewis, P. A. L. (1969) Oxygen toxicity during artificial ventilation.Thorax24, 656–666.
Burton, G. W. (1966) The value of carbon dioxide monitoring during anesthesia.Anesthesia21, 173–183.
Coles, J. R., Brown, W. A. andLampard, D. G. (1973) Computer control of respiration and anaesthesia.Med. & Biol. Eng.11, 262–267.
Comroe, J. H. Jun., Dripps, R. D., Dumke, P. R. andDeming, M. (1945) Oxygen toxicity.J.A.M.A.128, 710–717.
Comroe, J. H. Jun., Forster, R. E., Dubois, A. B., Briscoe, W. A. andCarlsen, E. (1965)The lung. Chicago, Year Book Medical Publishers, 313–316.
Cooper, E. A. (1967) Physiological dead space in passive respiration.Anesthesia22, 199–219.
Crossman, P. F., Bushnell, L. S. andWhyte, J. W. (1970) Dead space during artificial respiration: gas compression and mechanical dead space.J. Appl. Physiol.28, 94–97.
Danman, J. T., Guy, L. P. andDancis, J. (1954) Retrolental fibroplasia and oxygen therapy.J.A.M.A.155, 223–226.
Frumin, M. J., Bergman, M. A. andHoladay, D. A. (1959) Carbon dioxide and oxygen blood levels with a carbon dioxide controlled artificial respirator.Anesthesiology20, 313–320.
Gilbert, D. L. (1972) Oxygen and life.Anesthesiology37, 100–111.
Holloman, G. H. Jun., Milhorn, H. T. Jun. andColeman, T. G. (1968) A sampled-data regulator for maintaining a constant alveolar CO2.J. Appl. Physiol.25, 463–468.
Kamiyama, M., Tachibana, N. andYamamura, H. (1968) Automatic controller for artificial ventilation.Jap. J. Anesthesiology17, 1047–1048.
Kawakami, Y., Irie, T., Kishi, F., Osaki, Y., Murao, M., Mitamura, Y., Mikami, T. andSugawara, H. (1971) Application of a computerized respirator to patients with chronic obstractive pulmonary diseases.Jap. J. Chest Diseases30, 798–803.
Lewinsohn, G. E., Grassino, A. E., Channin, E. A. andTyler, J. M. (1970) Control of inspired oxygen concentration in pressure cycled ventilators,J.A.M.A.,211, 961–963.
Lambertsen, C. J. andWendel, H. (1960) An alveolar pco2 control system: its use to magnify respiratory depression by meperidine.J. Appl. Physiol.45, 43–48,
Markello, R., Cutter, J. A. andKing, B. D. (1963) Hyperventilation studies during nitrous oxide narcoticrelaxant anesthesia.Anesthesiology24, 225–230.
Mikami, T., Mitamura, Y., Yamamoto, K. andSugawara, H. (1972)A controlled assisting respirator. Monograph Series of the Research Institute of Applied Electricity, No. 20, 54–68.
Mitamura, Y., Mikami, T., Sugawara, H. andYoshimoto, C. (1971) An optimally controlled respirator.IEEE Trans.BME-18, 330–338.
Mitamura, Y., Mikami, T., Sugawara, H. andYoshimoto, C. (1971) Automatic control of respiration by an optimally controlled respirator.Jap. J. Med. Electron. & Biol. Eng.9, 397–405.
Nash, G., Blennerhassett, T. B. andPontoppidan, H. (1967) Pulmonary lesions associated with oxygen therapy and artificial ventilation.New Eng. J. Med.276, 368–374.
Nunn, J. F. andHill, D. W. (1960) Respiratory dead space and arterial to end-tidal CO2 tension difference in anesthetized man.J. Appl. Physiol.15, 383–389.
Pontoppidan, H., Whyte, J. H., Bendixen, H. H., Laver, M. B. andRadford, E. P. (1965) Ventilation and oxygen requirements during prolonged artificial ventilation in patients with respiratory failure.New Eng. J. Med.273, 401–409.
Pontoppidan, H. andBerry, P. R. (1967) Regulation of the inspired oxygen concentration during artificial ventilation.J.A.M.A.201, 89–92.
Radford, E. P., Ferris, B. J. andKriet, B. C. (1954) Clinical use of nomogram to estimate proper ventilation during artificial respiration.New Eng. J. Med.251, 877–884.
Radford, E. P. (1955) Ventilation standards for use in artificial respiration.J. Appl. Physiol.7, 451–460.
Severinghaus, J. W. andStupfel, M. (1957) Alveolar dead space as an index of distribution of blood flow in pulmonary capillaries.J. Appl. Physiol.10, 335–348.
Slater, E. M., Nilsson, S. E., Leake, D. L., Laver, M. B., Whyte, J. H. andBendixen, H. H. (1965) Arterial oxygen tension measurements during nitrous oxide-oxygen anesthesia.Anesthesiology26, 642–647.
Stadie, W. C., Ringgs, B. C. andHagaard, H. (1944) Oxygen poisoning.Am. J. Med. Sci.207, 84–114.
Suwa, K., Whyte, J. H. andBendixen, H. H. (1966) Circulation and dead space changes on controlling the ventilation of dogs.J. Appl. Physiol.21, 1855–1859.
Thornton, J. A. (1960) Physiological dead space.Anaesthesia15, 381–393.
Toll, M. D. (1972) An isolated transient-free soild-state a.c. power switch.Med, & Biol Eng.10, 532–535.
Waters, R. M. (1942) Newer viewpoints on clinical anesthesia.Fed. Proc.1, 213–219.
Watson, W. E. (1962) Observations on physiological dead space during intermittent positive pressure respiration.Brit. J. Anaesth.34, 502–508.
West, J. B. (1967)Ventilation/blood flow and gas exchange. Oxford, Blackwell Scientific Publications, 88–90.
Williams, J. V., Tirney, D. F. andParker, H. R. (1966) Surface factors in the lung, atelectasis, and transpulmonary pressure.J. Appl. Physiol.21, 819–827.
Winter, P. M. andSmith, G. (1972) The toxicity of oxygen.Anesthesiology37, 210–241.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mitamura, Y., Mikami, T. & Yamamoto, K. A dual control system for assisting respiration. Med. & biol. Engng. 13, 846–854 (1975). https://doi.org/10.1007/BF02478088
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02478088