Abstract
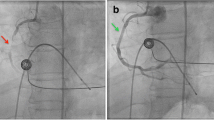
Percutaneous transluminal angioplasty (PTA) was performed on 25 patients with localized distal abdominal aortic stenoses. All patients were smokers and all complained of bilateral lower limb claudication. Eleven patients had small distal aortas and iliac vessels. Technically successful dilatation was achieved in all patients. Long-term follow-up was available on 17 of the patients. The mean follow-up period was 38 months. Cumulative patency at 5 years was 70%. Thirteen patients remain asymptomatic 15–83 months following PTA. Late failure occurred in 4 patients, 1–38 months following PTA. No complications related to PTA were experienced. PTA of localized aortic stenoses is a safe alternative to surgery and should be the treatment of choice in this condition.
Similar content being viewed by others
References
Heeney D, Bookstein J, Daniels E, Warmath M, Horn J, Rowley W (1983) Transluminal angioplasty of the abdominal aorta. Radiology 148:81–83
Charlebois N, Saint-Georges G, Hudon G (1986) Percutaneous transluminal angioplasty of the lower abdominal aorta. AJR 146:369–371
Velasquez G, Castaneda-Zuniga W, Formanek A (1980) Nonsurgical aortoplasty in Leriche syndrome. Radiology 134:359–360
Grollman JH, Del Vicario M, Mittal AK (1980) Percutaneous transluminal abdominal aortic angioplasty. AJR 134:1053–1054
Tegtmeyer CJ, Wellons HA, Thompson RN (1980) Balloon dilatation of the abdominal aorta. JAMA 244:2636–2637
Kumpe DA (1981) Percutaneous dilatation of an abdominal aortic stenosis. Three balloon catheter technique. Radiology 141:536–538
Hudon G, Bonan R, Hebert Y (1982) Abdominal aortic angioplasty: A case report with angiographic follow-up. J Can Assoc Radiol 33:262–264
Johnston KW, Colapinto RF, Baird RJ (1982) Transluminal dilatation: An alternative? Arch Surg 117:1604–1610
Coldman AJ, Elwood JM (1979) Examining survival data. Can Med Assoc J 121:1065–1071
Costantino MJ, Smith RB, Perdue GD (1979) Segmental aortic occlusion. An unusual lesion found in menopausal women. Arch Surg 114:317–318
De Laurentis DA, Friedmann P, Wolferth CC, Wilson A, Naide D (1978) Atherosclerosis and the hypoplastic aortoiliac system. Surgery 83:27–37
Szilagyi DE, Elliott JP, Smith RF, Reddy DJ, McPharlin M (1986) A thirty year survey of the reconstructive surgical treatment of aorto-iliac occlusive disease. J Vasc Surg 3:421–436
Cronenwett JL, Garrett HE (1983) Arteriographic measurement of the abdominal aorta, iliac and femoral arteries in women with atherosclerotic occlusive disease. Radiology 148:389–392
King RB, Myers KA, Scott DF, Devine TJ (1982) Aorto-iliac reconstructions for intermittent claudication. Br J Surg 69:169–172
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Odurny, A., Colapinto, R.F., Sniderman, K.W. et al. Percutaneous transluminal angioplasty of abdominal aortic stenoses. Cardiovasc Intervent Radiol 12, 1–6 (1989). https://doi.org/10.1007/BF02577116
Issue Date:
DOI: https://doi.org/10.1007/BF02577116