Abstract
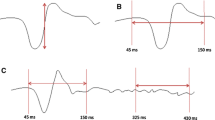
Chronic glaucoma has been shown preferentially to damage larger retinal cells and optic nerve fibres that provide the input to the magnocellular visual pathway. We compared the motion-onset visual evoked potentials (primarily the magnocellular system) with those to standard pattern reversal in 20 patients with bilateral chronic glaucoma. For motion-onset visual evoked potentials, the pattern (isolated 40′ checks of 10% contrast) moved in four cardinal directions (varied randomly from trial to trial) at a velocity of 10 deg/s for 20 ms, with an interstimulus interval of 1 s. In pattern-reversal stimulation, the checkerboard reversed at a rate of 2 reversals per second. In 60% of the eyes investigated, the results of both types of visual evoked potentials correlated, showing either normal (27.5%) or increased (32.5%) latencies. In the remaining 40% of the eyes, the normal pattern-reversal visual evoked potential latencies were accompanied by prolonged motion-onset visual evoked potentials. The high occurrence of delayed motion-onset visual evoked potentials in our patients confirms the primary magnocellular loss in chronic glaucoma and suggests that the motion-onset VEPs are suitable for detection of glaucomatous changes.
Similar content being viewed by others
References
Quigley HA, Dunkelberger GR, Green WR. Chronic human glaucoma causing selectively greater loss of large optic nerve fibres. Ophthalmology 1988; 95: 357–63.
Quigley HA, Sanchez RM, Dunkelberger GR, L'Hermaut NL, Baginski TA. Chronic glaucoma selectively damages large optic nerve fibres. Invest Ophthalmol Vis Sci 1981; 28: 913–20.
Livingstone M, Hubel D. Segregation of form, color, movement and depth: anatomy, physiology and perception. Science 1988; 240: 740–9.
Fitzke FW, Poinoosawmy D, Nagassubramanian S., Hitchings RA. Peripheral displacement thresholds in glaucoma and ocular hypertension. In: Heil A, ed. Perimetric update. Amsterdam: Kugler & Ghedini Publications, 1989: 399–452.
Silverman SE, Trick GL, Hart WM. Motion perception is abnormal in primary open-angle glaucoma and ocular hypertension. Invest Ophthalmol Vis Sci 1990; 31: 722–9.
Joffe KM, Raymond JE, Crichton A. Motion perimetry in glaucoma. Invest Ophthalmol Vis Sci 1991; 32: 1103.
Bullimore MA, Wood JM, Swenson K. Motion perception in glaucoma. Invest Ophthalmol Vis Sci 1993; 34: 3526–33.
Kubová Z, Kuba M, Spekreijse H, Blakemore C. Contrast dependence of motion-onset and pattern-reversal evoked potentials. Vision Res 1995; 35: 197–205.
Kuba M, Kubová Z. Visual evoked potentials specific for motion-onset. Doc Ophthalmol 1992; 80: 83–9.
Kuba M, Toyonaga N, Kubová Z. Motion-reversal visual evoked responses. Physiol Res 1992; 41: 369–73.
National Academy of Sciences-National Research Council Committee on Vision. Report of Working Group 39: recommended standard procedures for the clinical measurement and specification of visual acuity. Adv Ophthalmol 1980; 41: 103–48.
Towle VL, Moskowitz A, Sokol S, Schwartz B. The visual evoked potential in glaucoma and ocular hypertension: effects of check size, field size, and stimulation rate. Invest Ophthalmol Vis Sci 1983; 24: 175–83.
Göpfert E, Schlykowa L, Müller R. Zur topographie des Bewegungs-VEP am Menschen. Z EBG-BMG 1988; 19: 14–8.
Sokol S, Domar A, Moskowitz A, Schwartz H. Pattern evoked potential latency and contrast sensitivity in glaucoma and ocular hypertension. Doc Ophthalmol Proc Ser 1981; 27: 79–86.
Howe JW, Mitchell KW. Simultaneous recording of pattern electroretinogram and visual evoked cortical potential in group of patients with glaucoma. Doc Ophthalmol Proc Ser 1984; 40: 101–7.
Howe JW, Mitchell KW. Visual evoked cortical potential to paracentral retinal stimulation in chronic glaucoma, ocular hypertension, and an age-matched group of normals. Doc Ophthalmol 1986; 63: 37–44.
Fernández-Tirado FJ, Ucles P, Pablo L, Honrubia FM. Electrophysiological methods in early glaucoma detection. Acta Ophthalmol 1994; 72: 168–74.
Regan D. Steady-state evoked potentials. J Opt Soc Am 1977; 67: 1475–89.
Tobimatsu S, Tashima-Kurita S, Nakayama-Hiromatsu M, Kato M. Clinical relevance of phase of steady-state VEPs to P100 latency of transient VEPs. Electroencephalogr Clin Neurophysiol 1991; 80: 89–93.
Strasburger H. The analysis of steady-state evoked potentials revisited. Clin Vision Sci 1987; 1: 245–56.
Bray LCH, Mitchell KW, Howe JH, Gashau A. Visual function in glaucoma: a comparative evaluation of computerised static perimetry and the pattern visual evoked potential. Clin Vision Sci 1992; 7: 21–9.
Baez KA, McNaught AI, Dowler JGF, Poinoosawy D, Fitzke FW, Hitchins RA. Motion detection threshold and field progression in normal tension glaucoma. Br J Ophthalmol 1995; 79: 125–8.
Kubová Z, Kuba M, Juran J, Blakemore C. Is the motion system relatively spared in amblyopia? Evidence from cortical evoked responses. Vision Res 1996; 36: 181–90.
Kubová Z, Kuba M. Clinical application of motion-onset visual evoked potentials. Doc Ophthalmol 1992; 81: 209–18.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kubová, Z., Kuba, M., Hrochová, J. et al. Motion-onset visual evoked potentials improve the diagnosis of glaucoma. Doc Ophthalmol 92, 211–221 (1996). https://doi.org/10.1007/BF02583292
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02583292