Abstract
Introduction
Despite attempts to limit their use, systemic antibiotics are extensively prescribed for respiratory infections in France. This survey analyzed data from the Thales database, which contains information from 1010 representative French general practitioners (GPs). The objective was to assess French GP prescribing patterns in upper respiratory tract infections (URTIs) including the rate of prescription of systemic antibiotics and anti-inflammatory drugs in the presence or absence of prescribing fusafungine (Locabiotal®), an antibiotic with anti-inflammatory activity indicated for local use in URTIs. Drug costs to the French National Sickness Fund were also assessed.
Methods
This was a retrospective, longitudinal, case-control analysis. Prescribing patterns and costs were compared between patients who did and patients who did not receive fusafungine for a URTI (rhinopharyngitis, tonsillitis, or an influenza-like condition). The fusafungine group consisted of all patients in the database who were prescribed fusafungine at least once between 1 December 1999 and 30 November 2000. The control group was made up of randomly selected patients, matched for age and sex with the study group, who received at least one drug prescription (but not fusafungine) for a URTI during the same period. Patients were selected at the time of their first prescription, and their records for 1 year were analyzed.
Results
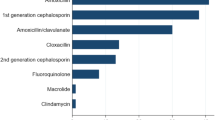
Each group contained 22 164 patients. For URTIs overall, systemic antibiotics were widely prescribed (at a rate of 54.6% and 67.8% in the fusafungine and control groups, respectively; p < 0.01). The rate of prescription of systemic antibiotics, NSAIDs and corticosteroids per prescription and per episode was significantly lower in the fusafungine group than in the control group.
The mean cost per prescription for the French National Sickness Fund was significantly lower for the three URTIs overall when fusafungine was prescribed (9.21 euros [€] vs €9.67; p < 0.01). The mean cost to the National Sickness Fund per prescription of systemic antibiotics, NSAIDs, and corticosteroids was also significantly lower in the fusafungine group compared with the control group. The cost of nasal preparations was higher in the fusafungine group because Locabiotal® is classified as a nasal preparation.
The cost per prescription to the National Sickness Fund was increased by the presence of systemic antibiotics, NSAIDs, or corticosteroids among the prescribed drugs and decreased with the prescription of fusafungine.
Conclusion
When fusafungine was prescribed for URTIs, fewer systemic antibiotics were prescribed, an important result in the current context of concern about emerging antibiotic resistance. The use of fusafungine was associated with a lower mean cost per prescription to the French National Sickness Fund.





Similar content being viewed by others
Notes
1The use of tradenames is for product identification purposes only and does not imply endorsement.
References
Gonzales R, Malone DC, Maselli JH, et al. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 2001; 15: 757–62
Witte W. Antibiotic resistance in Gram-positive bacteria: epidemiological aspects. J Antimicrob Chemother 1999; 44: 1–9
Cars O, Molstad S, Melander A. Variation in antibiotic use in the European Union. Lancet 2001; 357: 1851–3
Guillemot D. Les antibiotiques sont-ils surconsommés? Rev Prat 1998; 48: 585–6
Centre de Coordination de la Lutte contre les Infections Nosocomiales de l’ Interrégion Paris-Nord (CCLIN Paris-Nord). Surveillance des bactéries multirésistantes à partir du laboratoire dans les hôpitaux de l’ interrégion Paris- Nord (hors assistance Publique-Hôpitaux de Paris): rapport des résultats 2001. Paris: CCLIN Paris-Nord, 2002
Klugman KP, Goldstein F, Kohno S, et al. The role of fourth-generation cephalosporins in the treatment of infections caused by penicillin-resistant streptococci. Clin Microbiol Infect 1997; 3Suppl. 1: S48–60
Laurans G, Murbach V, Cattier B, et al. Observatoires régionaux du pneumocoque: surveillance de la sensibilité aux antibiotiques des pneumocoques isolés en situation pathogène en France en 1999 [online]. B.E.H. 2001 no. 33. Available from URL: http://www.invs.sante.fr/beh/2001/33/index.htm [Accessed 2003 Oct 13]
Chaix C, Durand-Zaleski I, Alberti C, et al. Control of endemic methicillinresistant Staphylococcus aureus: a cost-benefit analysis in an intensive care unit. JAMA 1999; 282: 1745–51
Ball P, Baquero F, Cars O, et al. Antibiotic therapy of community respiratory tract infections: strategies for optimal outcomes and minimized resistance emergence. The Consensus Group on Resistance and Prescribing In Respiratory Tract Infection. J Antimicrob Chemother 2002; 49: 31–40
Agence du Médicament. Antibiothérapie par voie générale en pratique courante: infections ORL et respiratoires basses. Presse Med 1999; 28: 406–14
Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med 2001; 134: 479–86
Agence Francaise de Sécurité Sanitaire des Produits de Santé (AFSSaPS). Antibiothérapie par voie generale en pratique courante: infections ORL et respiratoires basses. Ann Otolaryngol Chir Cervicofac 1999; 116: 302–14
Bradley CP. Decision making and prescribing patterns: a literature review. Fam Pract 1991; 8: 276–87
Greenhalgh T, Gill P. Pressure to prescribe. BMJ 1997; 315: 1482–3
Cockburn J, Pit S. Prescribing behaviour in clinical practice: patients’ expectations and doctors’ perceptions of patients’ expectations: a questionnaire study. BMJ 1997; 315: 520–3
Portier H. Résultat de l’évaluation du test de diagnostic rapide dans les angines. Abstract ORL-Pneumo-Allergo 2002; 2: 4–5
Guéniot C. Actualités des angines. Panorama Médecin 2001; 4824: 20
Caisse nationale d’assurance maladie. Mieux utiliser les antibiotiques, c’est préserver leur efficacité. Concours Med 2002; 124–23: 1614
Agence du Médicament. Prescription et consommation des antibiotiques en ambulatoire. Presse Med 1999; 28: 343–50
German-Fattal M. Fusafungine: an antimicrobial agent for the local treatment of respiratory tract infections. Clin Drug Invest 1996; 12: 308–17
German-Fattal M. Fusafungine, an antimicrobial with anti-inflammatory properties in respiratory tract infections. Clin Drug Invest 2001; 21: 653–70
Cuénant G. Value of Locabiotal® aerosol in rhinosinusitis. Rhinology Suppl 1988; 5: 69–74
Reinert P. Intérêt des test rapides pour la detection des infections streptococciques: illustration par une étude sur Locabiotal Pressuriseé dans les amygdalites. Maladies Médicaments 1989; 5: 113–23
Samolinski B, Zawisza E, Arcimowicz M, et al. Influence of fusafungine upon viral and bacterial infections. Med Sci Monit 1997; 3: 736–43
Bisno AL, Gerber MA, Gwaltney Jr JM, et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America. Clin Infect Dis 2002; 35: 113–25
Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med 2001; 134: 490–4
Hickner JM, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute rhinosinusitis in adults: background. Ann Intern Med 2001; 34: 498–505
Cooper RJ, Hoffmann JR, Bartlett JG, et al. Principles of appropriate antibiotic use for acute pharyngitis in adults: background. Ann Intern Med 2001; 134: 509–17
Guillemot D, Carbon C, Vauzelle-Kervroedan F, et al. Inappropriateness and variability of antibiotic prescription among French office-based physicians. J Clin Epidemiol 1998; 51: 61–8
Guillemot D, Maison P, Carbon C, et al. Trends in antimicrobial drug use in the community: France, 1981–1992. J Infect Dis 1998; 177: 492–7
Bouvenot G. French National Institute for prescriptions and consumption of medicines: prescriptions and consumption of antibiotics for respiratory infections. Bull Acad Natl Med 1999; 183: 601–13
Gerber MA, Randolph MF, Chanatry J, et al. Antigen detection test for streptococcal pharyngitis: evaluation of sensitivity with respect to true infections. J Pediatr 1986; 108: 654–8
Acknowledgments
The analysis of the data and preparation of this paper were supported by Les Laboratoires Servier, Neuilly-sur-Seine, France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fagnani, F., German-Fattal, M. Antibiotic Prescribing Patterns of French GPs for Upper Respiratory Tract Infections. Treat Respir Med 2, 491–498 (2003). https://doi.org/10.1007/BF03256676
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256676