Abstract
Background
Contrast-enhanced magnetic resonance imaging (MRI) is recommended for the diagnosis of acute osteoarticular infections in children. Diffusion-weighted imaging (DWI) may be an alternative to the injection of gadolinium.
Objective
To evaluate unenhanced MRI with DWI in comparison to contrast-enhanced MRI for the diagnostic work-up of acute osteoarticular infections in children.
Materials and methods
This retrospective study included 36 children (age range: 7 months-12 years) with extra-spinal osteoarticular infections and MRI performed within 24 h of admission. MRI protocol included short tau inversion recovery (STIR), water-only T2 Dixon, T1, DWI, and gadolinium-enhanced T1 sequences. Two readers reviewed three sets of images: 1) unenhanced sequences, 2) unenhanced sequences with DWI and 3) unenhanced followed by contrast-enhanced sequences (reference standard). Sensitivity and specificity of sets 1 and 2 were compared to set 3 and assessed to identify osteoarticular infections: osteomyelitis (long bones, metaphyseal equivalents), septic arthritis and abscess (soft tissues, bone).
Results
All 14 cases of osteomyelitis in the metaphyses and diaphyses of long bones and all 27 cases of septic arthritis were identified by unenhanced sequences, but 4/16 abscesses were missed. For the diagnosis of abscess, DWI increased sensitivity to 100%. Among the 18 osteomyelitis in metaphyseal equivalents, 4 femoral head chondroepiphyses were identified by contrast-enhanced sequences only.
Conclusion
MRI for suspected pediatric acute osteoarticular infections is the best diagnostic modality to guide patient management. An unenhanced protocol with DWI may be an alternative to a contrast-based protocol, even in the presence of an abscess. However, gadolinium remains necessary to assess for chondroepiphyseal involvement of the femoral head.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute pediatric osteoarticular infections bear significant morbidity if diagnosis and treatment are delayed, with potentially irreversible damage to the growing skeleton [1,2,3]. The need for prompt imaging and surgery is well documented and magnetic resonance imaging (MRI) holds a central role in current clinical algorithms [4, 5]. When acute osteoarticular infection is suspected in a child, emergency MRI aims to identify bone marrow signal abnormality, joint effusion and collections that can be targeted by puncture and aspiration to achieve a definite diagnosis [6, 7]. Alternatively, imaging findings will suggest a differential diagnosis and redirect management [8].
Contrast-enhanced MRI is the standard of imaging in children with suspected acute osteoarticular infection [9, 10]. However, safety concerns regarding the adverse effects of gadolinium retention in children raise the question of gadolinium-based contrast injection in pediatric MRI [11,12,13,14] . An unenhanced protocol that could confirm musculoskeletal infection and assist in the decision for surgical management is desirable.
Diffusion-weighted imaging (DWI) relates to tissue and fluid composition, such as high cellularity and viscosity of pus [15]. It has proven helpful in musculoskeletal imaging of adults for the diagnosis of soft-tissue abscess [16], osteomyelitis of the diabetic foot [17] and spine infections [18]. As for pediatric musculoskeletal imaging, previous studies have investigated the role of DWI in juvenile idiopathic arthritis [19, 20], chronic recurrent multifocal osteomyelitis [21] and bone tumors [22,23,24] but not for acute ostearticular infections.
The objective of our study was to assess whether DWI can replace contrast injection for the diagnosis of osteomyelitis, septic arthritis and abscess in children.
Materials and methods
This retrospective study was conducted in a single pediatric radiology center from January 2015 to March 2020 and was approved by our hospital’s local ethics committee (CE 14-102R).
We reviewed all consecutive MRIs performed before treatment of children admitted for suspected acute peripheral osteoarticular infection. Children with known hematological or oncological disease were excluded. Electronic medical records were searched for clinical and biological data.
MRI were performed on a 1.5-T unit (Avanto; Siemens, Erlangen, Germany) using the following protocol: T1-weighted (T1-W) turbo spin-echo (one longitudinal plane); two orthogonal planes with T2-weighting plus fat suppression (T2-W FS), short tau inversion recovery (STIR) (longitudinal plane) and water-only data set of fast spin-echo T2-weighted Dixon sequences (axial plane); DWI (axial plane) using single shot echo planar imaging (EPI), acquired using two b values, 0 and 800 s/mm2, with automatic monoexponential calculation of apparent diffusion coefficient (ADC) maps; and post-contrast injection T1-weighted spin echo with frequency-selective fat saturation (two orthogonal planes). Post-contrast sequences were obtained after injection of 0.2 ml/kg of gadoteric acid (Dotarem, Guerbet, France).
In young children, it may be difficult to localize the origin of infection because of ill-defined and nonspecific clinical symptoms. Therefore, MRI consistently started with a 3-D extended field of view (FOV) STIR to identify the anatomical site of signal abnormality. Subsequent sequences were acquired with a smaller FOV and with a dedicated peripheral coil targeted at the region of interest.
The approximate duration of MRI was 30 min, of which 15 to 20 min were dedicated to T1-W and T2-W FS sequences, 2 to 4 min were dedicated to DWI acquisition and 15 min to contrast injection, i.e. monitoring of venous catheter, manual injection and acquisition in two planes (acquisition time range: 7–11 min). General anesthesia was performed for children younger than 6 years old. Online Supplementary Material 1 includes a table with acquisition parameters depending upon the FOV dimension chosen to fit the anatomical location.
MRI analysis
All MRIs were anonymised, coded, transferred to and stored in random order on a dedicated computer station with OsiriX MD v 12.0.1 software (Geneva, Switzerland).
Image analysis was performed independently by two pediatric senior radiologists (C.H. and S.T., with 3 and 7 years of paediatric MRI experience, respectively), blinded to the clinical features, radiologic reports and final diagnoses, after a consensus-based training period on 10 patients. Disagreements were resolved by consensus.
Three sets of MRI sequences were compared:
-
1)
Unenhanced sequences (STIR, T2-W FS, T1-W): either STIR or water-only images of T2-W Dixon could be selected for analysis.
-
2)
Unenhanced sequences + DWI sequences.
-
3)
Unenhanced sequences + post-contrast sequences (T1-W FS).
The third combination was defined as the reference standard in keeping with relevant literature [9]. Each set of images was read successively without interval and was given a score immediately reported in a table.
Osteoarticular infections were divided into four patterns:
-
1)
Osteomyelitis in long bones (metaphyses and diaphyses).
-
2)
Osteomyelitis in metaphyseal equivalents (i.e. carpal and tarsal bones, margins of epiphyseal and apophyseal centers, and nonepiphyseal end of short tubular bones of the hands and feet). Although small round bones are epiphyseal equivalents, their ossifying centers behave like metaphyseal equivalents in the vicinity of the acrophysis along which enchondral growth occurs, hence for reasons of simplication, we defined them as metaphyseal equivalents [9, 25, 26]
-
3)
Septic arthritis.
-
4)
Abscess in bone or soft tissue (subperiosteal compartment, muscle and subcutaneous compartment).
The definition of infection on MRI was established on the basis of the existing literature [9, 14,15,16]. Accordingly, abnormal signal of bone, joint and cartilage (growth cartilage and epiphyses) was regarded as hypointense on T1-W sequences and hyperintense on fluid-sensitive sequences. Enhancement could be either increased (bone marrow in osteomyelitis, synovium in arthritis) or decreased (non-enhancing center with rim enhancement in abscess, enhancement defects in growth and epiphyseal cartilage). On DWI, osteomyelitis was characterized by high signal at b=800 and high signal on the apparent diffusion coefficient (ADC) map; joint effusion was characterized by low signal at b=800 and high signal on the ADC map, with opposite signal in case of purulent content; abscess was defined as a well-defined area of restricted diffusion, with high signal at b=800 and low signal on the ADC map. DWI was only assessed on a visual basis with correlation between the images acquired at high b value and the corresponding ADC map, without ADC quantification. When possible, comparison with the opposite side or limb was used to decide normal or abnormal signal.
A binary score was used for each MRI sequence to assess the absence (score 0) or the presence (score 1) of abnormal signal.
Statistical analysis
Descriptive analysis was used for patient characteristics and diagnosed pathologies. Sensitivity and specificity with 95% confidence interval (CI) were calculated to detect each of four patterns of osteoarticular infection on images in sets 1 and 2. All statistical analyses were performed using MedCalc for Windows (MedCalc Software, Ostend, Belgium). Inter-rater agreement was calculated using Kappa statistics, with level of agreement defined as almost perfect for values >0.90, strong 0.80–0.90 and moderate 0.60–0.79 [27].
Results
Patient characteristics
Our cohort included 38 children with proven osteoarticular infections for whom MRI was performed on admission. After excluding 2 cases because of image distortion on DWI, 36 patients were included (16 F/20 M), with a median age of 26 months (range: 7 months-12 years). Twenty-six children were younger than 5 years old. Symptoms lasted from 1 to 15 days (median: 3 days) before admission. Patient characteristics and clinical data are summarised in Table 1.
All MRIs were performed within 24 h of admission (range: 30 min–22 h 20 min, median: 3 h 5 min). Twenty-six patients (72%) underwent a surgical procedure following imaging, either for microbial identification or drainage/debridement. Pathogenic bacteria were identified in 32 patients, either by culture from bone, joint or blood samples, or by polymerase chain reaction assay on oropharyngeal swab: Kingella Kingae (56%), Methicillin-susceptible Staphylococcus aureus (22%), Streptococcus sp.(8%), Staphylococcus epidermidis (3%). In the remaining four children, the diagnosis of osteoarticular infection was made on the basis of clinical and biological findings and favorable evolution under empiric antibiotic therapy.
Of the 32 cases of osteomyelitis in long bones and metaphyseal equivalents, 27 cases of septic arthritis and 16 bone/periosteal abscesses were identified. The anatomical regions involved were, in decreasing order, the hip (9), the ankle (7), the foot (7), the knee (6), the elbow (3), the pelvis (2), the hand (1) and the shoulder (1). Each patient was scanned once but may have displayed more than one pattern of infection. Table 2 shows sensitivity and specificity of unenhanced and DWI sequences depending on the pattern of infection.
Diagnostic MRI
Osteomyelitis in long bones
Fourteen patients (39%) had osteomyelitis in long bone metaphyses or diaphyses, distributed as follows: 6 femurs, 3 fibulas, 2 tibias, 2 ulnas and 1 metatarsal bone. All cases were identified on standard unenhanced sequences with no added value of DWI.
Osteomyelitis in metaphyseal equivalents
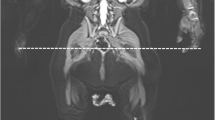
Eighteen patients (50%) had osteomyelitis in a metaphyseal equivalent, distributed as follows: 11 epiphyses, 3 tarsal bones, 2 carpal bones, 1 pubic bone close to the triradiate cartilage and 1 iliac bone close to the sacroiliac joint. The 11 affected epiphyses (median age: 20 months) involved the ossification centers of 5 femoral heads, 3 distal tibias, 2 distal femurs and 1 proximal humerus. Of the 18 metaphyseal equivalent osteomyelites, 14 were identified on standard unenhanced sequences with no additive value of DWI. All 4 missed locations were the femoral head chondro-epiphysis, in patients ages 9, 10, 13 and 30 months old. Abnormal signal indicative of injury was only depicted as absent enhancement on contrast-enhanced sequences (Fig. 1).
A 10-month-old boy with left femoral chondroepiphyseal injury from left hip arthritis. a Coronal STIR demonstrates joint effusion alone (arrow). b On the coronal T1-weighted image, the ossification center of the femoral head is unremarkable (arrow). c Axial DWI (b value of 800 s/mm2) confirms joint effusion (arrow), but the femoral head has normal signal in comparison to the right side (asterisk). d Coronal T1-weighted fat-suppressed image after contrast injection demonstrates absent enhancement of left femoral chondroepiphysis (white arrow); there is enhancement around the joint capsule consistent with arthritis (black arrow). DWI diffusion-weighted imaging, STIR short tau inversion recovery
Septic arthritis
Among the 27 patients with arthritis, 7 (26%) were isolated and 20 (74%) were concurrent with osteomyelitis. All cases were identified on standard unenhanced sequences with no added value of DWI.
Abscesses
Soft-tissue abscesses
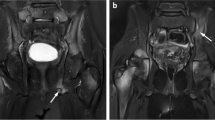
Ten patients (28%) had an abscess in a soft-tissue location (i.e. in subcutaneous soft tissue, subperiosteal space and tendon sheath). Of these, eight were identified on standard unenhanced sequences. DWI identified all cases (Fig. 2).
A 12-year-old girl with a soft-tissue abscess associated with arthritis and cellulitis of the ankle. a Axial STIR shows ill-defined and circumferential oedema of the soft tissues around the ankle (arrows). b Axial DWI (b value of 800 s/mm2) allows delineation of a circumscribed subcutaneous collection (arrow). c An axial T1-weighted fat-suppressed image after contrast injection confirms a subcutaneous abscess (curved arrows). DWI diffusion-weighted imaging, STIR short tau inversion recovery
Bone abscesses
Six patients (17%) had an abscess in the bone medullary cavity. Of these, four were identified on standard unenhanced sequences. In all six cases, DWI was positive for the diagnosis of an abscess (Fig. 3).
A 20-month-old boy with bone abscess in osteomyelitis of the distal tibia. a Coronal STIR shows a focus of high signal of the metaphysis and physis of the distal tibia (arrow), within a background of medullary hyperintensity, consistent with osteomyelitis (star). b A coronal T1-weighted image shows corresponding focal hypointense signal (arrow) and diffuse hypointense metaphysis (star). c Axial DWI (b value of 800 s/mm2) depicts a focus of hyperintensity (arrow). d An axial T1-weighted fat-suppressed image after contrast injection confirms a small bone abscess with peripheral enhancement around a low signal core (arrow). DWI diffusion-weighted imaging, STIR short tau inversion recovery
Inter-reader agreement
Global inter-reader agreement was strong with a Kappa coefficient of 0.826 (95% CI, 0.78–0.88). Kappa coefficients ranged from 0.68 to 0.92 for the conventional unenhanced sequences, from 0.72 to 0.87 for DWI and from 0.71 to 0.87 for post-contrast sequences, depending on the pattern of infection.
Discussion
Magnetic resonance imaging is the modality of choice for investigating acute osteoarticular infections in children, decision-making about antibiotic therapy and surgical management [4,5,6].
Previous pediatric studies showed that T1-W and fluid-sensitive (STIR and T2-W with fat suppression) sequences are sufficient to confirm or exclude osteomyelitis and arthritis, but gadolinium injection remains the reference standard to identify complications of osteomyelitis such as abcess, and growth cartilage and chondroepiphyseal injury [9, 10, 13, 14, 28]. Averill et al. [13] retrospectively studied the MRIs of 78 children with suspected osteoarticular infection and demonstrated equal sensitivity and specificity between pre-contrast and post-contrast images for the diagnosis of osteomyelitis. However, reader confidence for abscess was increased with contrast injection. Similarly, a more recent analysis of 90 pediatric MRIs by Markhardt et al. [14] showed that fluid-sensitive sequences were as sensitive as contrast-enhanced sequences with a 100% negative predictive value for osteoarticular infection, although the diagnosis of concomitant abscess was missed in three cases without contrast injection. Other authors reviewed MRI studies of 14 epiphyseal osteomyelitis cases in children in correlation with surgery [28]. Among the 10/14 abnormally enhanced epiphyses, 4 corresponded to either chondroepiphyseal abscess or injury without abscess, highlighting that an enhancement defect may indicate chondroepiphyseal involvement. In line with these studies, current MRI guidelines recommend witholding gadolinium injection when pre-contrast sequences are normal, and reserving contrast medium for suspected abscess and/or epiphyseal involvement [9, 10].
To avoid gadolinium injection, we evaluated the diagnostic performance of an unenhanced protocol with DWI in comparison with a standard contrast-enhanced MRI. To our knowledge, DWI is not currently part of routine pediatric MRI protocols for osteoarticular infection in most centers, although recently, Chaturvedi [29] reported the usefulness of DWI to assess for subperiosteal abscess in children based on unpublished data. So far, only adult studies have emphasized that ADC values can differentiate osteomyelitis from noninfectious bone marrow edema [17, 30, 31].
In our study, all cases of osteomyelitis and arthritis were correctly identified by unenhanced sequences. The addition of DWI increased the sensitivity of unenhanced sequences for the detection of abscess, by demonstrating bright signal on high b value images with corresponding low intensity on ADC map. Interestingly, we report one 11-year old boy with ankle osteomyelitis complicated by bone necrosis for which DWI showed restricted diffusion, but contrast-enhanced sequences did not confirm bone abscess. We considered this case a false-positive bone abscess on DWI. Importantly, in the absence of contrast medium, this misdiagnosis would not have altered the patient’s management. In either case, bone abscess and bone necrosis, surgical debridement is necessary to improve antibiotic therapy efficiency [13].
Another important issue shown by our study is that DWI is less sensitive in detecting femoral head chondroepiphysial involvement in children younger than the age of 30 months. This age group has an increased propensity for chondroepiphyseal infection [9, 26, 30]. The femoral head frequently does not enhance after contrast injection in hip infection. The reason for this peculiar behavior on MRI remains controversial and may be related to direct infection or to ischemic phenomena concomitant with joint infection [32,33,34]. In our cohort, four diseased femoral heads were missed on non-enhanced and DWI images. There is an age-related increase in fat marrow content and parallel decrease of enhancement of the epiphyses [35]. This may partly explain why non-contrast images are less sensitive to abnormal epiphyseal signal in the younger patient, whose epiphyses contain less fat. Moreover, the small size of growing epiphyseal ossification centers may negatively affect spatial resolution and render difficult the detection of any abnormal signal. Similarly, we presumed that DWI could not identify altered signal of the femoral head chondroepiphyses because of their fatty, marrow-rich and low proton density content, which makes them appear normally hypointense on DWI and ADC map [15, 36]. In our series, the other seven epiphyses showed abnormal signal on pre-contrast sequences and therefore contrast-enhanced sequences had no added value for the diagnosis of chondritis and osteomyelitis.
Our study is limited by its retrospective nature and its small sample size. However, it is notable for the very young age of our cohort (72% were younger than 5 years old) for whom MRI, without contrast injection, could be of increased interest. One reason for the limited number of patients is that we already regularly dispense with contrast medium in MRI studies when pre-contrast and DWI sequences are informative enough to enable the decision for surgical management and to guide the procedure. The retrospective nature of our work, along with the absence of a control group, could have been the source of bias by positively influencing the interpretation in cases of uncertainty. Regarding DWI, we only analysed images on a qualitative basis, as either increased or decreased signal with visual correlation to the ADC map, without measuring ADC values. Although our inter-reader agreement was high, the visual analysis of DWI may lead to subjective interpretation in ill-trained radiologists. It may be even more difficult when small bones of the extremities are examined, where cumulative dephasing from increased K space filling to increase resolution can be responsible for image distorsion. In our study, we chose the axial plane for DWI to minimize geometric distortion.
Another limitation of our study relates to its reproducibility in other institutions. In our pediatric hospital, we are able to perform an emergent MRI any time septic arthritis or osteomyelitis is suspected, but we are aware that MRI and general anesthesia are not always available during night shifts and out-of-hours in every hospital. Finally, we emphasize that our study was designed to test DWI as part of an MRI protocol for invstigating osteoarticular infection, and not to differentiate infection from alternative diagnoses, such as Langerhans cell histiocytosis.
Our study acts as a reminder that all MRI protocols should be tailored to each individual patient. The decision to inject contrast medium should be undertaken while the unenhanced images are acquired. To that end, we encourage the routine addition of DWI to standard unenhanced sequences for the work-up of osteoarticular infections in children and suggest the following recommendations:
-
As currently and widely accepted, when T1- and T2-W FS are negative, there is no need for DWI and contrast medium.
-
When T1- and T2-W FS are positive, DWI should be performed; if DWI does not show restricted diffusion, then contrast medium is not required.
-
However, if DWI shows restricted diffusion in soft tissue or bone, then the likelihood of an abscess is high. Depending on the radiologist’s level of confidence, contrast medium should be considered to increase the accuracy of findings. Alternatively, the radiologist may chose to abstain from injecting contrast medium when images are informative enough to guide the orthopedist’s surgical procedure.
In addition, contrast-enhanced sequences should be maintained for suspected proximal femoral head involvement especially in young children, irrespective of the suspected underlying mechanism (direct infection, transient ischemia) since it impacts decision-making regarding joint aspiration, duration of antibiotic therapy and clinical follow-up. It would be useful to perform multicenter studies in a larger cohort to obtain data that would support our recommandations and our belief that contrast can be avoided in many children with this common acute pathology.
Conclusion
Emergency unenhanced MRI with DWI can establish the diagnosis of acute osteoarticular infections in children and negates the need for gadolinium. Such a protocol is sufficient for prompt medical and surgical management. However, gadolinium-based contrast injection remains necessary to evaluate the femoral head chondroepiphysis in younger children, in whom diffusion imaging is not reliable.
References
Yeo A, Ramachandran M (2014) Acute haematogenous osteomyelitis in children. BMJ 348:g66
Ceroni D, Kampouroglou G, Valaikaite R et al (2014) Osteoarticular infections in young children: what has changed over the last years? Swiss Med Wkly 144:w13971
Peters W, Irving J, Letts M (1992) Long-term effects of neonatal bone and joint infection on adjacent growth plates. J Pediatr Orthop 12:806–810
Griswold BG, Sheppard E, Pitts C et al (2020) The introduction of a preoperative MRI protocol significantly reduces unplanned return to the operating room in the treatment of pediatric osteoarticular infections. J Pediatr Orthop 40:97–102
Quick RD, Williams J, Fernandez M et al (2018) Improved diagnosis and treatment of bone and joint infections using an evidence-based treatment guideline. J Pediatr Orthop 38:e354–e359
Jaramillo D, Treves ST, Kasser JR et al (1995) Osteomyelitis and septic arthritis in children: appropriate use of imaging to guide treatment. AJR Am J Roentgenol 165:399–403
Kan JH, Hilmes MA, Martus JE et al (2008) Value of MRI after recent diagnostic or surgical intervention in children with suspected osteomyelitis. AJR Am J Roentgenol 191:1595–1600
Lindsay AJ, Delgado J, Jaramillo D, Chauvin NA (2019) Extended field of view magnetic resonance imaging for suspected osteomyelitis in very young children: is it useful? Pediatr Radiol 49:379–386
Jaramillo D, Dormans JP, Delgado J et al (2017) Hematogenous osteomyelitis in infants and children: imaging of a changing disease. Radiology 283:629–643
Safdar NM, Rigsby CK, Iyer RS et al (2018) ACR appropriateness criteria acutely limping child up to age 5. J Am Coll Radiol 15:S252–S262
Blumfield E, Swenson DW, Iyer RS, Stanescu AL (2019) Gadolinium-based contrast agents - review of recent literature on magnetic resonance imaging signal intensity changes and tissue deposits, with emphasis on pediatric patients. Pediatr Radiol 49:448–457
Stanescu AL, Shaw DW, Murata N et al (2020) Brain tissue gadolinium retention in pediatric patients after contrast-enhanced magnetic resonance exams: pathological confirmation. Pediatr Radiol 50:388–396
Averill LW, Hernandez A, Gonzalez L et al (2009) Diagnosis of osteomyelitis in children: utility of fat-suppressed contrast-enhanced MRI. AJR Am J Roentgenol 192:1232–1238
Markhardt BK, Woo K, Nguyen JC (2019) Evaluation of suspected musculoskeletal infection in children over 2 years of age using only fluid-sensitive sequences at MRI. Eur Radiol 29:5682–5690
Chavhan GB, Alsabban Z, Babyn PS (2014) Diffusion-weighted imaging in pediatric body MR imaging: principles, technique, and emerging applications. Radiographics 34:E73–E88
Chun CW, Jung J-Y, Baik JS et al (2018) Detection of soft-tissue abscess: comparison of diffusion-weighted imaging to contrast-enhanced MRI. J Magn Reson Imaging 47:60–68
Martin Noguerol T, Luna Alcala A, Beltran LS et al (2017) Advanced MR imaging techniques for differentiation of neuropathic arthropathy and osteomyelitis in the diabetic foot. Radiographics 37:1161–1180
Dumont RA, Keen NN, Bloomer CW et al (2019) Clinical utility of diffusion-weighted imaging in spinal infections. Clin Neuroradiol 29:515–522
Neubauer H, Evangelista L, Morbach H et al (2012) Diffusion-weighted MRI of bone marrow oedema, soft tissue oedema and synovitis in paediatric patients: feasibility and initial experience. Pediatr Rheumatol Online J 10:20
Barendregt AM, Mazzoli V, van Gulik EC et al (2020) Juvenile idiopathic arthritis: diffusion-weighted MRI in the assessment of arthritis in the knee. Radiology 295:373–380
Leclair N, Thormer G, Sorge I et al (2016) Whole-body diffusion-weighted imaging in chronic recurrent multifocal osteomyelitis in children. PLoS One 11:e0147523
Baunin C, Schmidt G, Baumstarck K et al (2012) Value of diffusion-weighted images in differentiating mid-course responders to chemotherapy for osteosarcoma compared to the histological response: preliminary results. Skeletal Radiol 41:1141–1149
Lee SK, Jee W-H, Jung CK et al (2020) Prediction of poor responders to neoadjuvant chemotherapy in patients with osteosarcoma: additive value of diffusion-weighted MRI including volumetric analysis to standard MRI at 3T. PLoS One 15:e0229983
Jaramillo D (2010) Whole-body MR imaging, bone diffusion imaging: how and why? Pediatr Radiol 40:978–984
Oestreich AE (2004) The acrophysis: a unifying concept for understanding enchondral bone growth and its disorders. II. Abnormal growth. Skeletal Radiol 33:119–128
Nixon GW (1978) Hematogenous osteomyelitis of metaphyseal-equivalent locations. AJR Am J Roentgenol 130:123–129
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Johnson DP, Hernanz-Schulman M, Martus JE et al (2011) Significance of epiphyseal cartilage enhancement defects in pediatric osteomyelitis identified by MRI with surgical correlation. Pediatr Radiol 41:355–361
Chaturvedi A (2021) Pediatric skeletal diffusion-weighted magnetic resonance imaging, part 2: current and emerging applications. Pediatr Radiol 51:1575–1588
Eguchi Y, Ohtori S, Yamashita M et al (2011) Diffusion magnetic resonance imaging to differentiate degenerative from infectious endplate abnormalities in the lumbar spine. Spine (Phila Pa 1976) 36:E198–E202
Dietrich O, Geith T, Reiser MF, Baur-Melnyk A (2017) Diffusion imaging of the vertebral bone marrow. NMR Biomed 30(3):e3333
Kwack K-S, Cho JH, Lee JH et al (2007) Septic arthritis versus transient synovitis of the hip: gadolinium-enhanced MRI finding of decreased perfusion at the femoral epiphysis. AJR Am J Roentgenol 189:437–445
Kim EY, Kwack K-S, Cho JH et al (2012) Usefulness of dynamic contrast-enhanced MRI in differentiating between septic arthritis and transient synovitis in the hip joint. AJR Am J Roentgenol 198:428–433
Ogden JA (1979) Pediatric osteomyelitis and septic arthritis: the pathology of neonatal disease. Yale J Biol Med 52:423–448
Dwek JR, Shapiro F, Laor T et al (1997) Normal gadolinium-enhanced MR images of the developing appendicular skeleton: part 2. Epiphyseal and metaphyseal marrow. AJR Am J Roentgenol 169:191–196
MacKenzie JD, Gonzalez L, Hernandez A et al (2007) Diffusion-weighted and diffusion tensor imaging for pediatric musculoskeletal disorders. Pediatr Radiol 37:781–788
Funding
Open access funding provided by University of Geneva.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
Summary of acquisition parameters depending on the size of field-of-view and coil, chosen to fit the patient and the location of disease. In children younger the 6 years old, the initial sequence is an extended field-of-view three-dimensional short tau inversion recovery sequence. (DOCX 21.5 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Habre, C., Botti, P., Laurent, M. et al. Benefits of diffusion-weighted imaging in pediatric acute osteoarticular infections. Pediatr Radiol 52, 1086–1094 (2022). https://doi.org/10.1007/s00247-022-05329-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05329-3