Abstract
Background
Recently, laparoscopic distal pancreatectomy (LDP) has become the standard procedure for resection of left-sided pancreatic tumors. Fluid collection (FC) at the resection margin of the pancreatic stump after LDP is a frequent radiological finding. However, there have been few treatment guidelines and the optimal management for this clinical finding is unclear. The aim of present study is to define the incidence of FC and suggest the optimal management for FC after LDP.
Methods
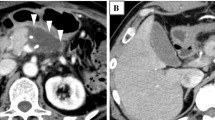
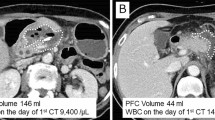
A total of 1227 patients who underwent LDP between March 2005 and December 2015 were collected. FC was considered present when the longest diameter of the lesion on CT scan was > 3 cm.
Results
A follow-up with at least two CT image was available for 1102 patients. Of these, 689 (62.5%) patients showed initial fluid collection (IFC) at the pancreas resection site in immediate postoperative CT. IFC (+) group had higher proportion of men, BMI, and higher rate of concomitant splenectomy than IFC (−) group. Among patients with FC after LDP, the treatment group had more frequent leukocytosis and accompanying symptoms than the observation group. Seventy-seven patients underwent therapeutic interventions for FC after LDP. Among them, 55 (71.4%) patients underwent endoscopic ultrasonography-guided gastrocystostomy (EUS-GC). EUS-GC group had a higher success rate (85.6 vs. 63.6%, p < 0.033) and shorter hospital stay after the intervention (5.2 vs. 13.3 days, p < 0.001) than those who underwent other procedures.
Conclusions
High BMI, male, and concomitant splenectomy contribute to the occurrence of FC after LDP. In most cases, FC after LDP resolved spontaneously over time with observation. The patients with symptomatic FC ultimately required treatment. EUS-GC is the optimal intervention therapy for FC after LDP.



Similar content being viewed by others
References
Song KB et al (2011) Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc 25(10):3364–3372
Xie K et al (2012) Laparoscopic distal pancreatectomy is as safe and feasible as open procedure: a meta-analysis. World J Gastroenterol 18(16):1959–1967
Xia T et al (2017) Risk factors for postoperative pancreatic fistula after laparoscopic distal pancreatectomy using stapler closure technique from one single surgeon. PLoS ONE 12(2):e0172857
Nakamura M et al (2011) Prolonged peri-firing compression with a linear stapler prevents pancreatic fistula in laparoscopic distal pancreatectomy. Surg Endosc 25(3):867–871
Miyasaka Y et al (2017) Attempts to prevent postoperative pancreatic fistula after distal pancreatectomy. Surg Today 47(4):416–424
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bassi C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591
Shin SH et al (2015) A comparative study of laparoscopic vs. open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg 220(2):177–185
Gagner M, Pomp A, Herrera MF (1996) Early experience with laparoscopic resections of islet cell tumors. Surgery 120(6):1051–1054
Kooby DA et al (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248(3):438–446
Mabrut JY et al (2005) Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery 137(6):597–605
Liang S, Hameed U, Jayaraman S (2014) Laparoscopic pancreatectomy: indications and outcomes. World J Gastroenterol 20(39):14246–14254
Bauman MD et al (2017) Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surg Endosc 32(1):53–61
Chang YR et al (2017) Prediction of pancreatic fistula after distal pancreatectomy based on cross-sectional images. World J Surg 41(6):1610–1617
Goh BK et al (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143(10):956–965
Moskovic DJ et al (2010) Drain data to predict clinically relevant pancreatic fistula. HPB (Oxford) 12(7):472–481
Sierzega M et al (2013) Natural history of intra-abdominal fluid collections following pancreatic surgery. J Gastrointest Surg 17(8):1406–1413
Tjaden C et al (2016) Fluid collection after distal pancreatectomy: a frequent finding. HPB (Oxford) 18(1):35–40
Seeliger H et al (2010) Risk factors for surgical complications in distal pancreatectomy. Am J Surg 200(3):311–317
Ferrone CR et al (2008) Pancreatic fistula rates after 462 distal pancreatectomies: staplers do not decrease fistula rates. J Gastrointest Surg 12(10):1691–1697; discussion 1697–8
Tang CW et al (2014) Spleen-preserving distal pancreatectomy or distal pancreatectomy with splenectomy?: Perioperative and patient-reported outcome analysis. J Clin Gastroenterol 48(7):e62–e66
Shoup M et al (2002) The value of splenic preservation with distal pancreatectomy. Arch Surg 137(2):164–168
Pendola F et al (2017) Distal pancreatectomy for benign and low grade malignant tumors: short-term postoperative outcomes of spleen preservation—a systematic review and update meta-analysis. J Surg Oncol 115(2):137–143
Varadarajulu S, Trevino JM, Christein JD (2009) EUS for the management of peripancreatic fluid collections after distal pancreatectomy. Gastrointest Endosc 70(6):1260–1265
Raijman I et al (2015) Endoscopic drainage of pancreatic fluid collections using a fully covered expandable metal stent with antimigratory fins. Endosc Ultrasound 4(3):213–218
Kwon YM et al (2013) Management of peripancreatic fluid collections following partial pancreatectomy: a comparison of percutaneous versus EUS-guided drainage. Surg Endosc 27(7):2422–2427
Acknowledgements
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (Grant Number: HI14C2640).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ki Byung Song, Jaewoo Kwon, Young-Joo Lee, Dae Wook Hwang, Jae Hoon Lee, Sang Hyun Shin, Myung-Hwan Kim, Sung Koo Lee, Dong-Wan Seo, Sang Soo Lee, Do Hyun Park, Tae Jun Song, Guisuk Park, Yejong Park, Seung Jae Lee, and Song Cheol Kim have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Song, K.B., Kwon, J., Lee, YJ. et al. The treatment indication and optimal management of fluid collection after laparoscopic distal pancreatectomy. Surg Endosc 33, 3314–3324 (2019). https://doi.org/10.1007/s00464-018-06621-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06621-w