Abstract
Introduction
COVID-19 vaccines have been developed to compact the current SARS-CoV-2 pandemic and have been administered to people all over the world. These vaccines have been quite effective in reducing the possibility of severe illness, hospitalization and death. However, the recent emergence of Variants of Concern specifically the delta variant, B.1.617.2, had resulted in additional waves of the pandemic.
Methods
We aim to review the literature to understand the transmission and disease severity, and determine the efficacy of the current COVID-19 vaccines. We searched Pubmed, Scopus, and Embase till August 4th 2021, and used the search terms “delta variant”, “vaccinations”,” breakthrough infections”, and “neutralizing antibody”. For the meta-analysis, 21 studies were screened in particular and five articles (148,071 cases) were included in the study, and only four were analyzed in the meta-analysis.
Results
In this review, both in vitro and in vivo studies showed significant reductions in neutralization rates against delta variants for vaccinated individuals and convalescent patients with prior history of COVID-19. However, There was a lower incidence of infection with SARS-CoV-2 due to Delta variant was found after the second dose of Pfizer-BioNTech, Oxford-AstraZeneca and Moderna vaccines.
Conclusion
In fully vaccinated individuals, symptomatic infection with the delta variant was significantly reduced, and therefore, vaccinations play an important role to assist the fight against delta variant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The emergence of the COVID-19 had shocked the world and affected every nation. Coronaviruses belong to a large family of viruses that have been recognized as large positive-stranded RNA viruses [1]. These viruses are known to have a high predisposition for errors in replication which gives a unique advantage for the virus to increasingly mutate with every replication cycle [2]. These mutations make the virus even more virulent and thereby increase its transmissibility and also evade the host’s natural or acquired immunity [3].
With the continued pandemic, there is a real concern about the effects of emerging variants of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The emergence of these variants had caused concern among the public as well as the healthcare workers (HCWs) [4]. These variants are classified as variants of interest (VOI) and variants of concern (VOC) [5]. VOC refers to variants that have increased transmissibility or virulence, and VOI refers to those with the potential to cause the disease. The first known case of delta variant was first identified in India in late 2020 and ever since has spread worldwide to over 60 countries [6, 7]. Multiple vaccines against SARS-CoV-2 have been authorized and rolled out worldwide, all have been designed based on the original Wuhan SARS-CoV-2 S protein that was first sequenced in January 2020 [8]. Vaccines efficacy depends on stimulating an appropriate antibody and T-cell response to S protein [9]. Efforts to fight the COVID-19 virus have focused on the spike protein which is crucial for the virus to enter the cells [10]. The spike protein is divided into an N-terminal S1 domain which allows the virus to attach to the host cells through the angiotensin-converting enzyme (ACE) 2 receptor and a C-terminal S2 domain which allows the virus to adhere to the cell membrane [11, 12]. The S1 domain has two specific domains known as the N-terminal domain (NTD) and a receptor-binding domain (RBD) [13]. Most of the vaccines that have been developed and some monoclonal antibodies that have been used in combatting this virus have specifically focused on the S domain [9, 14].
Despite the vaccinations, the virus evolved due to several mutations that have been appearing on the RBD and the NTD [15] and consequently in VOC and VOI. Out of all the variants that are present at the time of this review, the delta variant B.1.617.2 has become the most concerning of all, due to its high rates of transmission not only in India but also worldwide [16]. The pace at which the delta variant is out-competing other variants can be elucidated from the publicly available data from the COG-UK/ME explorer for the variants of concern in the UK, Scotland, and Northern Ireland. The initial data showed that 47.91% of all the new cases were delta variants and the alpha variant (B.1.1.7.1) comes in a distant second at 0.15% [17]. We intend to discuss the effect of convalescent sera, monoclonal antibodies (mAb), and sera of vaccinated individuals on delta variants based on in vitro tests first and then discuss the effect of vaccination on Delta variants. In addition, we conducted a meta-analysis to evaluate COVID-19 vaccine effectiveness against variants to provide a numeric estimate of the efficacy.
Methods
We reviewed the literature to understand the transmission and disease severity, and determine the efficacy of the current vaccines. We searched Pubmed, Scopus, and Embase till August 4th 2021, and used the search terms “delta variant”, “vaccinations”,” breakthrough infections”, and “neutralizing antibody”.
In addition, to examine the effectiveness/efficacy of SARS-CoV-2 vaccines against the Delta [B.1.617.2] variant, we conducted a meta-analysis to evaluate COVID-19 vaccine to provide a numeric estimate. We used a protocol from the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) statement. Vaccine effectiveness measures of how well a vaccine protects people from infection (e.g., vaccine effectiveness of 88% means that 88% of people will be protected from becoming infected with SARS-CoV-2 and 12% of people will still be at risk of becoming infected with SARS-CoV-2). We also used the risk of bias in non-randomized studies-of interventions (ROBINS-I) tool to evaluate studies with low risk of bias and high quality [18]. Taking a conservative approach, a random effect with the DerSimoniane–Laird model was used [19]. This approach results in wider confidence intervals [CIs] than a fixed-effect model. Statistical heterogeneity was assessed utilizing χ2 test and I2 statistics [20]. An I2 value of < 40% indicates low heterogeneity, 30–60% moderate heterogeneity, 50–90% substantial heterogeneity, and 75–100% considerable heterogeneity. To detect the source of heterogeneity, subgroup analysis was performed based on vaccine brand administered [Pfizer-BioNTech, Oxford-AstraZeneca, and Moderna]. Publication bias was evaluated using funnel plots and the Egger’s correlation test, with p < 0.05 indicating statistical significance [21]. R version 4.1.0 with the packages metafor and meta was used for all statistical analyses.
Results
In vitro tests against the delta variant
Convalescent sera
A study evaluated the neutralization ability of the sera against delta variants, and was based on the reduction in titers with a comparison reference to the D614G (B.1 lineage)[22]. There were four-to-sixfold reduction in the neutralization rate against the delta variants [22]. This means that the delta variant is less sensitive to the antibodies produced by natural infection, and thus, there is a possibility of reinfection with the delta variant. This emphasizes the need for vaccinations in people who have already built immunity due to previous exposure to COVID-19.
Monoclonal antibodies
A set of monoclonal antibodies (casirivimab, bamlanivimab, imdevimab, and etesevimab) had been approved and all of them target the RBD region. It was shown that all these monoclonal antibodies have reduced sensitivity against the delta variant and that bamlanivimab in specific did not show any antiviral activity [23, 24].
Sera of vaccinated individuals
Several studies have been done to evaluate the efficacy of vaccinations on the delta variant. In some studies, the efficacy of the sera against D614G was measured, whereas in other studies, wild type virus was used to test the sensitivity of Delta variant to the sera of vaccinated individuals [22, 25, 26]. In one study, the sera of vaccinated individuals after a single dose of Pfizer vaccine (BNT162b2) and AstraZeneca vaccine (ChAdOx1 nCoV-19) showed very low levels of neutralizing antibody activity [22]. However, when the sera of vaccinated individuals were used after the completion of two doses of the COVID-19 vaccine, there were higher levels of neutralizing antibodies. The efficacy of two doses of either AstraZeneca vaccine or Pfizer-Biontech was 60% and 88%, respectively [22]. In another study from India, sera collected from patients vaccinated with the BBV152 (COVAXIN) vaccine had neutralizing antibodies against the delta variant, but this was reduced by 1.95 times [16]. In the Legacy study, neutralizing antibodies (NAbs) were determined from 149 participants who received one dose (median time of 30 days) and 159 who had two doses (median time = 28 days) of BNT162b2 against multiple SARS-CoV-2 strains including wild-type and B.1.617.2 [25]. Of the group who had two doses, 3% did not have neutralizing antibodies (Nab) against B.1.617.2 and these antibodies were generally 5·8 (95% CI 5·0–6·9) fold less against B.1.617.2 compared to the wild-type [25]. Reduced NAb activity against B.1.617.2 relative to B.1.1.7 strain after one vaccine dose was also related to age and time since the second dose of the BNT162b2 vaccine [25]. In vitro neutralization studies, not yet peer-reviewed at the time of this review, conducted by Moderna (mRNA-1273) also showed that there is a 2.1-fold reduction in neutralizing titers of delta variant [27]. In another study which is yet to be peer-reviewed, it was shown that the single dose of the Johnson & Johnson vaccine (Ad26.COV2.S) had shown low neutralizing antibody titers against the delta variants and thus make the vaccinated individuals vulnerable to breakthrough infections [28]. It, therefore, can be seen that although there has been lower efficacy against delta variant, vaccinations may still play an important role for developing resistance toward the delta variant. In a company-sponsored study, researchers tested 20 volunteers immunized with BNT162b2 from the original clinical trial [29] for neutralization. Serum was taken 2–4 weeks after the second dose showed the following geometric mean neutralization titers (GMT) against spike protein: 502 for USAWA1/2020, 302 for B.1.525, 157 for B.1.617.1, 157 for B.1.617.2, 355 B.1.617.2, 343 for B.1.617.2.v2, and 331 for B.1.618, and these were statistically lower than the wild-type USAWA1/2020 [30]. Thus, neutralization of most of the variants was considerably reduced relative to the wild-type virus. Sera from eight participants of the Ad26.COV2.S COVID‐19 vaccine ENSEMBLE trial [31] was collected 71 days post single dose; in comparison to wild type, there was a 1.6-fold reduction in GMT [31]. Another study involving 20 participants who received either one or two doses of Ad26.COV2.S reported a median neutralizing antibody titer of 184 against wild type versus 171 against the B.1.617.1 variant, and 107 against the B.1.617.2 variant [32].
Effect of vaccinations on delta variant in vivo
The emergence of significant mutations on the spike protein like D614G, L452R, T19R, dell157-158, T478K, D614G, P681R, and D950N had been well documented [33]. The mutations called 452R and 478 K have allowed the virus to replicate at a faster pace, which in turn contributes to higher transmissibility [34].
A test-negative case–control study compared vaccination status in persons with symptomatic COVID-19 with BNT162b2 or ChAdOx1 nCoV-19 vaccines. The study included 14,837 with alpha variant and 4272 with delta variants. In the pooled analysis of all vaccinated individuals, one dose of the vaccine was less effective against the delta variant (30.7%; 95% CI 25.2–35.7) than the alpha variant (48.7%; 95% CI 45.5–51.7) [35]. Two doses of any of the vaccines showed the effectiveness of 87.5% (95% CI 85.1–89.5) against the alpha variant and 79.6% (95% CI 76.7–82.1) against the delta variant [35]. For BNT162b2, there was a small difference in the effectiveness against the different variants with 93.7% (95% CI 91.6–95.3) for the alpha variant and 88.0% (95% CI 85.3–90.1) for the delta variant [35]. However, ChAdOx1 nCoV-19 was 74.5% [95% CI 68.4–79.4] effective against alpha and only 67.0% [95% CI 61.3–71.8] against delta [35]. The study did not have enough number of cases nor did it account for sufficient time for follow-up, to evaluate the effectiveness in terms of hospitalizations or deaths [35]. The effectiveness with heterologous vaccinations (meaning one dose being BNT162b2 and the other being ChAdOx1 nCoV-19) was found to be 79.6%. This study is specifically important for the countries to change their policies with regards to the vaccination strategies. There was a consensus earlier that increasing the dosing intervals between the two shots would increase the efficacy of the vaccine and also increase the possibility of a larger population being vaccinated [36]. This policy with the ever-increasing spread of delta variant would not be productive as a single dose of the vaccination could put these populations at risk. However, in another study, a single shot of ChAdOx1 nCoV-19 for residents in a care home that was exposed to delta variant did not need any hospitalizations [37]. This might be because the second dose of the vaccine was given on the same day of exposure to the delta variant.
Protection from B.1.617.1 (Kappa) (with L452R and E484Q mutations in RBD) and B.1.617.2 (Delta) (with RBD L452R and T478K mutations in RBD) by vaccines has been of concern. Liu et al. tested neutralization activity against the latter variants from 25 individuals who received two doses of BNT162b2 vaccine, administered 3 weeks apart, with serum taken 4–14 days after the second dose. The neutralization titers against B.1.617.1 and B.1.617.2 were reduced 2.7-fold (p < 0.0001) and 2.5-fold (p < 0.0001) respectively, relative to a Wuhan-related strain (isolated early in the pandemic from Australia). Additionally, neutralization was tested from another 25 individuals who received two doses of ChAdOx1nCoV-19 administered 8–14 weeks apart, with serum taken 14–28 days after the second dose. The neutralization titers against B.1.617.1 and B.1.617.2 were reduced 2.6-fold (p < 0.0001) and 4.3-fold (p < 0.0001), respectively, relative to the Wuhan-related strain. Finally, they tested 20 volunteers 10 weeks after a single dose of BNT162b2 and found a complete absence of neutralization [38].
The effectiveness of available SARS-CoV-2 vaccines against the variant of concern Delta [B.1.617.2]
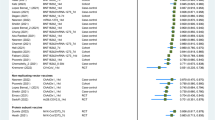
Our literature search revealed 21 articles and after full-text screening we identified five articles (148,071 cases), and only four were included in the meta-analysis (Fig. 1). The key findings of vaccine effectiveness against variants of concern (Delta) are presented in Table 1. Overall, there was low certainty of evidence that one dose of Pfizer-BioNTech prevented symptomatic infection from the Delta variant (range of mean estimates: 79–88%) [35, 39]. There was a moderate certainty of evidence that two doses of Pfizer-BioNTech prevented symptomatic infection from the Delta variant (range of mean estimates: 87–96%) [40,41,42]. There was also low certainty of evidence that one dose of Oxford-AstraZeneca prevented symptomatic infection from the Delta variant (range of mean estimates: 60–67%); and a moderate certainty of evidence that two doses of ChAdOx1 vaccine prevented symptomatic infection from the Delta variant (range of mean estimates: 59.8–92%) [40, 42]. There was moderate certainty of evidence that Moderna prevented symptomatic infection and hospitalization from the Delta variant (72% and 96%, respectively) [41]. Of the 152,752 COVID-19 vaccine recipients who received the first dose and included in the meta-analysis, the overall pooled proportion who had a laboratory-confirmed SARS-CoV-2 infection with Delta variant after Pfizer-BioNTech vaccination was 42.4% (95% CI 0.0–54.5, n = 30,882, 4 studies, I2 = 99%, p < 0.01), while 19.4% (95% CI 0.0–30.7, n = 120,879, 4 studies, I2 = 99%, p < 0.0001) suffered infection with SARS-CoV-2 due to Delta variant after Oxford-AstraZeneca and 56.5% (95% CI 30–83, n = 991, 1 study) after Moderna vaccination (Fig. 2). As expected, lower incidence of infection with SARS-CoV-2 due to the Delta variant was found after the second dose of Pfizer-BioNTech (4.8, 95% CI 0.0–9.3, I2 = 93%), Oxford-AstraZeneca (9.7, 95% CI 0.0–14.1, I2 = 99%), and Moderna (5.0, 95% CI − 4.6 to 14.7) vaccination (Fig. 3). Funnel plots for possible publication bias for the pooled effect size to determine the prevalence of infections in SARS-CoV-2 patients with Delta variant appeared asymmetrical on visual inspection, and Egger’s tests showed asymmetry (p values < 0.05).
Delta variant effect in high-risk activities
High-risk activities or performance sports put people in close quarters and there are low chances of people to socially distance themselves or adhere to wearing masks while performing such activities. A recent report showed two cases of trekkers who were fully vaccinated with both Moderna and AstraZeneca test positive for delta variants [43]. The trekker with the AstraZeneca vaccine developed severe pneumonia and the other trekker had mild sore throat and congestion. Both the trekkers eventually got better. In a similar context, a recent outbreak that happened in a gymnastics facility highlights how easily a single infected case of the delta variant can spread quickly in the facility and the community, as well [44]. Among the 47 cases that had the delta variant, only two needed hospitalization and they both happened among unvaccinated individuals.
Delta variant effect on fully vaccinated individuals at large social events
Social events are places that bring people in close proximity and can produce high chances of transmission for the delta variants. A recent wedding event had a small outbreak of delta variant infection among the attendees [45]. The significant difference here was the fact that all six individuals were fully vaccinated. Among them, one of the individuals who was vaccinated with BBV152(COVAXIN) died, whereas the other individual vaccinated with Pfizer (BNT162b2) needed monoclonal antibody infusion. This shows a distinct case of vaccine breakthrough where the person’s immune system might have not generated the necessary immunological response to the vaccinations or maybe that immunity started to wane over time.
Delta variant effect on health care workers
In a recent outbreak in a hospital in Finland, it can be seen how the delta variant could spread so quickly among patients and health care workers (HCWs) [46]. Among the 58 patients (mean age 80 years) who were infected, there were 18 deaths. Among these 18 patients, only one patient who died was fully vaccinated, 11 were vaccinated with one dose and 6 were unvaccinated individuals. The age of the patients and any underlying comorbidities might have some effect, but a majority of the deaths were due to the delta variant. Among HCWs, there were about 45 cases of infections, but no deaths, and the mean age among the HCWs was 38 years. These HCWs also contributed further to secondary infections in the community with whom they were in close contact. This highlights the presence of breakthrough infections with the delta variant, even in individuals who are fully vaccinated.
Despite the availability of vaccines worldwide, there has been an overwhelming vaccine hesitancy [38]. In the Kingdom of Saudi Arabia, the initial willingness of the HCWs to receive the ChAdOx1 nCoV-19 and RNA BNT162b2 vaccines were 24.4%, and 20.9%, respectively [47]. In USA, for example, the vaccination rates can range from 44.8% in Mississippi and 75.4% in Vermont [48]. This is a worrying trend, since in a matter of a month (July 13th–August 13th, 2021), the 7 day moving average in the USA had increased by 350% [48]. This just shows how fast the delta variant can transmit and cause disruptions not only in the USA but also worldwide. It is highly imperative that it is time for the unvaccinated HCWs to understand the situation and make informed decisions to get vaccinated. There is also a need for additional doses for immunocompromised individuals and booster doses for other individuals overtime. It is also important that administration of booster doses follow the order of priority and be given to older age groups followed by younger age groups. This is because historically it had been shown that vaccine efficacy decreases with age, and that innate immunity shows a decline with the age [49, 50]. Few studies had shown that the heterologous vaccinations (BNT162b2 and ChAdOx1 nCoV-19), may results in a strong immune response [51, 52]. In the meantime, there is a continued need to focus on wearing masks, practice hand hygiene and cough etiquette, and to observe social distancing to end this pandemic.
In conclusion, SARS-CoV-2 seems to be constantly outsmarting us and trying to survive by mutating in ways that gives it a significant advantage to bypass the immune system. The delta variant, at this time, is the most concerning among the variants given its higher rate of transmission and the reduced neutralizing activities. The only way to slow down its spread is through complete vaccinations and following health protocols that are in place. Also, it is important to have policies for preparing health systems (both supplies and personnel), identifying populations at risk, following vaccination shortfalls and expanding vaccination coverage, and early detection and quarantine of COVID-19 cases, must be set forth at local levels. It is important to have further research on variants and to develop vaccines that can tackle the variants that exist currently and those that might emerge in the future.
References
Robson F, Khan KS, Le TK, Paris C, Demirbag S, Barfuss P, et al. Coronavirus RNA proofreading: molecular basis and therapeutic targeting. Mol Cell. 2020;79:710–27. https://doi.org/10.1016/j.molcel.2020.07.027.
Tegally H, Wilkinson E, Lessells RJ, Giandhari J, Pillay S, Msomi N, et al. Sixteen novel lineages of SARS-CoV-2 in South Africa. Nat Med. 2021;27:440–6. https://doi.org/10.1038/s41591-021-01255-3.
Volz E, Hill V, McCrone JT, Price A, Jorgensen D, O’Toole Á, et al. Evaluating the effects of SARS-CoV-2 spike mutation D614G on transmissibility and pathogenicity. Cell. 2021;184:64-75.e11. https://doi.org/10.1016/J.CELL.2020.11.020.
Temsah MH, Barry M, Aljamaan F, Alhuzaimi AN, Al-Eyadhy A, Saddik B, et al. SARS-CoV-2 B.1.1.7 UK variant of concern lineage-related perceptions, COVID-19 vaccine acceptance and travel worry among healthcare workers. Front Public Heal. 2021. https://doi.org/10.3389/fpubh.2021.686958.
Centers for Disease Control and Prevention. SARS-CoV-2 variant classifications and definitions n.d. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html (accessed 21 Aug 2021)
ECDC. Threat assessment brief: emergence of SARS-CoV-2 B.1.617 variants in India and situation in the EU/EEA 2021. https://www.ecdc.europa.eu/en/publications-data/threat-assessment-emergence-sars-cov-2-b1617-variants (accessed 16 Aug 2021).
Centers for Disease Control and Prevention (CDC). SARS-CoV-2 variant classifications and definitions 2021. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcases-updates%2Fvariant-surveillance%2Fvariant-info.html (accessed 16 Aug 2021).
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–74. https://doi.org/10.1016/S0140-6736(20)30251-8.
Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586:516–27. https://doi.org/10.1038/s41586-020-2798-3.
Du L, He Y, Zhou Y, Liu S, Zheng B-J, Jiang S. The spike protein of SARS-CoV–a target for vaccine and therapeutic development. Nat Rev Microbiol. 2009;7:226–36. https://doi.org/10.1038/nrmicro2090.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271-280.e8. https://doi.org/10.1016/j.cell.2020.02.052.
Huang Y, Yang C, Xu XF, Xu W, Liu SW. Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharmacol Sin. 2020;41:1141–9. https://doi.org/10.1038/s41401-020-0485-4.
Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–20. https://doi.org/10.1038/s41586-020-2180-5.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–16. https://doi.org/10.1056/nejmoa2035389.
Greaney AJ, Starr TN, Gilchuk P, Zost SJ, Binshtein E, Loes AN, et al. Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell Host Microbe. 2021;29:44-57.e9. https://doi.org/10.1016/j.chom.2020.11.007.
Yadav PD, Sapkal GN, Abraham P, Ella R, Deshpande G, Patil DY, et al. Neutralization of variant under investigation B.1.617.1 With sera of BBV152 vaccinees. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab411.
COG-UK/Mutation Explorer n.d. http://sars2.cvr.gla.ac.uk/cog-uk/ (accessed 16 Aug 2021)
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016. https://doi.org/10.1136/bmj.i4919.
DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–14. https://doi.org/10.1016/j.cct.2006.04.004.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al (Eds) Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Training. Cochrane; 2021.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34. https://doi.org/10.1136/bmj.315.7109.629.
Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, et al. Reduced sensitivity of SARS-CoV-2 variant delta to antibody neutralization. Nature. 2021;596:276–80. https://doi.org/10.1038/s41586-021-03777-9.
Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, et al. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science. 2021;371:850–4. https://doi.org/10.1126/science.abf9302.
Taylor PC, Adams AC, Hufford MM, de la Torre I, Winthrop K, Gottlieb RL. Neutralizing monoclonal antibodies for treatment of COVID-19. Nat Rev Immunol. 2021;21:382–93. https://doi.org/10.1038/s41577-021-00542-x.
Wall EC, Wu M, Harvey R, Kelly G, Warchal S, Sawyer C, et al. Neutralising antibody activity against SARS-CoV-2 VOCs B.1.617.2 and B.1.351 by BNT162b2 vaccination. Lancet. 2021;397:2331–3. https://doi.org/10.1016/S0140-6736(21)01290-3.
Mlcochova P, Kemp S, Shanker Dhar M, Papa G, Meng B, Mishra S, et al. SARS-CoV-2 B.1.617.2 delta variant emergence and vaccine breakthrough 1 2 n.d. Mlcochova. https://doi.org/10.1101/2021.05.08.443253
Maeda K, Amano M, Uemura Y, Tsuchiya K, Matsushima T, Noda K, et al. Correlates of neutralizing/SARS-CoV-2-S1-binding antibody response with adverse effects and immune kinetics in BNT162b2-vaccinated individuals. MedRxiv. 2021. https://doi.org/10.1101/2021.07.27.21261237.
Tada T, Zhou H, Samanovic MI, Dcosta BM, Cornelius A, Mulligan MJ, et al. Comparison of neutralizing antibody titers elicited by mRNA and adenoviral vector vaccine against SARS-CoV-2 variants. BioRxiv Prepr Serv Biol. 2021. https://doi.org/10.1101/2021.07.19.452771.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–15. https://doi.org/10.1056/nejmoa2034577.
Liu J, Liu Y, Xia H, Zou J, Weaver SC, Swanson KA, et al. BNT162b2-elicited neutralization of B.1.617 and other SARS-CoV-2 variants. Nature. 2021;596:273–5. https://doi.org/10.1038/s41586-021-03693-y.
Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384:2187–201. https://doi.org/10.1056/nejmoa2101544.
Barouch DH, Stephenson KE, Sadoff J, Yu J, Chang A, Gebre M, et al. Durable humoral and cellular immune responses 8 months after Ad26.COV2.S vaccination. N Engl J Med. 2021. https://doi.org/10.1056/nejmc2108829.
Centre for Disease Prevention E. Emergence of SARS-CoV-2 B.1.617 variants in India and situation in the EU/EEA 2021.
Adam D. What scientists know about new, fast-spreading coronavirus variants. Nature. 2021;594:19–20. https://doi.org/10.1038/D41586-021-01390-4.
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med. 2021;385:585–94. https://doi.org/10.1056/nejmoa2108891.
Flaxman A, Marchevsky N, Jenkin D, Aboagye J, Aley PK, Angus BJ, et al. Tolerability and immunogenicity after a late second dose or a third dose of ChAdOx1 nCoV-19 (AZD1222). SSRN Electron J. 2021. https://doi.org/10.2139/SSRN.3873839.
Williams SV, Vusirikala A, Ladhani SN, De Olano EFR, Iyanger N, Aiano F, et al. An outbreak caused by the SARS-CoV-2 Delta (B.1.617.2) variant in a care home after partial vaccination with a single dose of the COVID-19 vaccine Vaxzevria, London, England, April 2021. Eurosurveillance. 2021. https://doi.org/10.2807/1560-7917.es.2021.26.27.2100626.
Liu C, Ginn HM, Dejnirattisai W, Supasa P, Wang B, Tuekprakhon A, et al. Reduced neutralization of SARS-CoV-2 B.1.617 by vaccine and convalescent serum. Cell. 2021;184:4220-4236.e13. https://doi.org/10.1016/j.cell.2021.06.020.
Sheikh A, McMenamin J, Taylor B, Robertson C. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet. 2021;397:2461–2. https://doi.org/10.1016/S0140-6736(21)01358-1.
Bernal JL, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of COVID-19 vaccines against the B.1.617.2 variant. MedRxiv. 2021. https://doi.org/10.1101/2021.05.22.21257658.
Nasreen S, Chung H, He S, Brown KA, Gubbay JB, Buchan SA, et al. Effectiveness of COVID-19 vaccines against variants of concern in Ontario, Canada. MedRxiv. 2021. https://doi.org/10.1101/2021.06.28.21259420.
Stowe J, Andrews N, Gower C, Gallagher E, Utsi L, Simmons R, et al. Effectiveness of COVID-19 vaccines against hospital admission with the Delta (B.1.617.2) variant. Preprint 2021.
Amatya B, Pandey P, Dawadi S, Manandhar S. COVID-19 in fully vaccinated Everest trekkers in Nepal. J Travel Med. 2021. https://doi.org/10.1093/jtm/taab098.
Dougherty K. SARS-CoV-2 B.1.617.2 (delta) variant COVID-19 outbreak associated with a gymnastics facility—Oklahoma, April–May 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1004–7. https://doi.org/10.15585/MMWR.MM7028E2.
Farinholt T, Doddapaneni H, Qin X, Menon V, Meng Q, Metcalf G, et al. Transmission event of SARS-CoV-2 delta variant reveals multiple vaccine breakthrough infections. MedRxiv Prepr Serv Heal Sci. 2021. https://doi.org/10.1101/2021.06.28.21258780.
Hetemäki I, Kääriäinen S, Alho P, Mikkola J, Savolainen-Kopra C, Ikonen N, et al. An outbreak caused by the SARS-CoV-2 delta variant (B.1.617.2) in a secondary care hospital in Finland May 2021. Eurosurveillance. 2021. https://doi.org/10.2807/1560-7917.es.2021.26.30.2100636.
Temsah MH, Barry M, Aljamaan F, Alhuzaimi A, Al-Eyadhy A, Saddik B, et al. Adenovirus and RNA-based COVID-19 vaccines’ perceptions and acceptance among healthcare workers in Saudi Arabia: a national survey. BMJ Open. 2021. https://doi.org/10.1136/bmjopen-2020-048586.
CDC. CDC COVID data tracker 2021. https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases (accessed 18 Aug 2021)
Lord JM. The effect of aging of the immune system on vaccination responses. Hum Vaccines Immunother. 2013;9:1364–7. https://doi.org/10.4161/hv.24696.
Nikolich-Zugich J, Knox KS, Rios CT, Natt B, Bhattacharya D, Fain MJ. SARS-CoV-2 and COVID-19 in older adults: what we may expect regarding pathogenesis, immune responses, and outcomes. GeroScience. 2020;42:505–14. https://doi.org/10.1007/s11357-020-00186-0.
Lin A, Liu J, Ma X, Zhao F, Yu B, He J, et al. Heterologous vaccination strategy for containing COVID-19 pandemic. MedRxiv. 2021. https://doi.org/10.1101/2021.05.17.21257134.
Groß R, Zanoni M, Seidel A, Conzelmann C, Gilg A, Krnavek D, et al. Heterologous ChAdOx1 nCoV-19 and BNT162b2 prime-boost vaccination elicits potent neutralizing antibody responses and T cell reactivity. MedRxiv. 2021. https://doi.org/10.1101/2021.05.30.21257971.
Bernal JL, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021. https://doi.org/10.1136/bmj.n1088.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study design: JAT, TK, SA, and MB; literature review and data extraction: JAT, TK, SA, and MB; data analysis: JAT, TK, SA, and MB; data interpretation: all authors; writing of the manuscript draft: all authors; final manuscript approval: all authors.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Al-Tawfiq, J.A., Koritala, T., Alhumaid, S. et al. Implication of the emergence of the delta (B.1.617.2) variants on vaccine effectiveness. Infection 50, 583–596 (2022). https://doi.org/10.1007/s15010-022-01759-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01759-1