Abstract
Background
Adjuvant radiotherapy after breast-conserving surgery (BCS) for breast cancer (BC) is a well-established indication. The risk of ischaemic heart disease after radiotherapy for BC increases linearly with the heart mean dose with no apparent threshold. Radiotherapy to the left breast in deep inspiration breath-hold (DIBH) reduces the dose to the heart. A new linac system with an integrated surface scanner (SS) for DIBH treatments was recently installed in our department. We tested it for potential benefits, safety, patients’ acceptance/compliance and associated additional workload.
Materials and methods
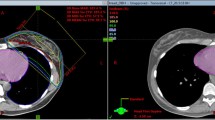
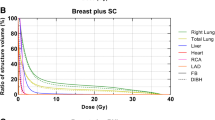
Twenty consecutive patients following BCS for breast carcinoma of the left side were enrolled in our institutional DIBH protocol. We compared dose to the heart and ipsilateral lung (IL) between plans in DIBH and free breathing (FB) using standard defined parameters: mean dose, maximal dose to a volume of 2 cm3 (D2 cm 3), volume receiving ≥ 5 Gy (V5), 10 Gy (V10), 15 Gy (V15) and 20 Gy (V20). Comparison of median calculated dose values was performed using a two-tailed Wilcoxon signed rank test.
Results
DIBH was associated with a statistically significant reduction (p < 0.001) in all studied parameters for the heart and the IL. In 16 of 20 patients the heart D2 cm 3 was less than 42 Gy in DIBH. In FB the heart D2 cm 3 was ≥ 42 Gy in 17 of 20 patients. The median daily treatment time was 9 min.
Conclusion
Radiotherapy of the left breast in DIBH using a SS could easily be incorporated into daily routine and is associated with significant dose reduction to the heart and IL.
Zusammenfassung
Hintergrund
Die adjuvante Strahlentherapie nach brusterhaltener Operation (BCS) bei Brustkrebs (BC) ist eine seit langem anerkannte Behandlungsform. Das postradiogene Risiko einer kardialen Ischämie steigt linear ohne erkennbaren Schwellenwert mit der mittleren Herzdosis. Die Bestrahlung der linken Brust in tiefer Inspiration unter Anhalten der Atmung (DIBH) reduziert die Herzdosis. Nach kürzlich erfolgter Installation eines neuen Linearbeschleunigers einschließlich eines laserbasierten Oberflächenscanners wurde das System bei der Bestrahlung der Brust in DIBH auf seinen möglichen Nutzen, die Sicherheit, die Patientenakzeptanz und Mitarbeit sowie die zusätzliche Arbeitsbelastung getestet.
Material und Methoden
Zwanzig Patientinnen mit linksseitigem BC wurden nach BCS entsprechend unserem klinikinternen Protokoll in TI bestrahlt. Es wurden zwischen den Plänen in DIBH und Atemmittellage die Herzdosis und die ipsilaterale Lungendosis mit Hilfe der folgenden Standardparameter verglichen: mittlere Dosis, maximale Dosis in 2 cm3 (D2 cm 3), Teilvolumina mit einer Dosis von ≥ 5 Gy (V5), 10 Gy (V10), 15 Gy (V15) und 20 Gy (V20). Zum Vergleich der medianen Dosiswerte für jeden Parameter wurde ein Wilcoxon-Vorzeichen-Rang-Test eingesetzt.
Ergebnisse
In Bezug auf das Herz und die ipsilaterale Lunge konnte bei der DIBH eine statistisch signifikante Reduktion (p < 0,001) aller untersuchten Parameter gezeigt werden. In 16 von 20 Patientinnen war die D2 cm 3 des Herzens bei der DIBH unter 42 Gy. In Atemmittellage war die D2 cm 3 des Herzens bei 17 von 20 Patientinnen ≥ 42 Gy. Die durchschnittliche Behandlungszeit betrug 9 min.
Schlussfolgerung
Die Strahlentherapie der linken Brust in DIBH mittels Oberflächenscanner ist eine leicht zu implementierende Methode, welche mit einer signifikanten Dosisreduktion des Herzens und der ipsilateralen Lunge assoziiert ist.





Similar content being viewed by others
References
Early Breast Cancer Trialists’ Collaborative Group (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378:1707–1716
Sedlmayer F, Sautter-Bihl ML, Budach W et al (2013) DEGRO practical guidelines: radiotherapy of breast cancer I: radiotherapy following breast conserving therapy for invasive breast cancer. Strahlenther Onkol 189:825–833
American Cancer Society (2013) Breast cancer facts & figures 2013–2014. American Cancer Society, Atlanta
Cuzick J, Stewart H, Rutqvist L et al (1994) Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol 12:447–453
Sardaro A, Petruzzelli MF, D’Errico MP et al (2012) Radiation-induced cardiac damage in early left breast cancer patients: risk factors, biological mechanisms, radiobiology, and dosimetric constraints. Radiother Oncol 103:133–142
Darby SC, Ewertz M, McGale P et al (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368:987–998
McGale P, Darby SC, Hall P et al (2011) Incidence of heart disease in 35,000 women treated with radiotherapy for breast cancer in Denmark and Sweden. Radiother Oncol 100:167–175
Darby SC, McGale P, Taylor CW, Peto R (2005) Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol 6:557–565
Hayden AJ, Rains M, Tiver K (2012) Deep inspiration breath hold technique reduces heart dose from radiotherapy for left-sided breast cancer. J Med Imaging Radiat Oncol 56:464–472
Swanson T, Grills IS, Ye H et al (2013) Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am J Clin Oncol 36:24–30
Korreman SS, Pedersen AN, Aarup LR et al (2006) Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys 65:1375–1380
Zurl B, Stranzl H, Winkler P, Kapp KS (2010) Quantitative assessment of irradiated lung volume and lung mass in breast cancer patients treated with tangential fields in combination with deep inspiration breath hold (DIBH). Strahlenther Onkol 186:157–162
Stranzl H, Zurl B (2008) Postoperative irradiation of left-sided breast cancer patients and cardiac toxicity. Does deep inspiration breath-hold (DIBH) technique protect the heart? Strahlenther Onkol 184:354–358
Bartlett FR, Colgan RM, Carr K (2013) The UK HeartSpare Study: randomised evaluation of voluntary deep-inspiratory breath-hold in women undergoing breast radiotherapy. Radiother Oncol 108:242–247
Nielsen MH, Berg M, Pedersen AN et al, Danish Breast Cancer Cooperative Group Radiotherapy Committee (2013) Delineation of target volumes and organs at risk in adjuvant radiotherapy of early breast cancer: national guidelines and contouring atlas by the Danish Breast Cancer Cooperative Group. Acta Oncol 52:703–710
The international commission on radiation units and measurements (2010) Prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT). J ICRU 10
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Gagliardi G, Lax I, Ottolenghi A, Rutqvist LE (1996) Long-term cardiac mortality after radiotherapy of breast cancer—application of the relative seriality model. Br J Radiol 69:839–846
Gagliardi G, Constine LS, Moiseenko V et al (2010) Radiation dose-volume effects in the heart. Int J Radiat Oncol Biol Phys 76:S77–S85
Nakamura N, Takahashi O, Kamo M et al (2014) Effects of geometrical uncertainties on whole breast radiotherapy: a comparison of four different techniques. J Breast Cancer 17:157–160
Farace P, Zucca S, Solla I et al (2012) Planning hybrid intensity modulated radiation therapy for whole-breast irradiation. Int J Radiat Oncol Biol Phys 84:e115–e122
van Mourik A, van Kranen S, den Hollander S et al (2011) Effects of setup errors and shape changes on breast radiotherapy. Int J Radiat Oncol Biol Phys 79:1557–1564
Joosten A, Bochud F, Moeckli R (2014) A critical evaluation of secondary cancer risk models applied to Monte Carlo dose distributions of 2-dimensional, 3-dimensional conformal and hybrid intensity-modulated radiation therapy for breast cancer. Phys Med Biol 59:4697–4722
Joosten A, Matzinger O, Jeanneret-Sozzi W et al (2013) Evaluation of organ-specific peripheral doses after 2-dimensional, 3-dimensional and hybrid intensity modulated radiation therapy for breast cancer based on Monte Carlo and convolution/superposition algorithms: implications for secondary cancer risk assessment. Radiother Oncol 106:33–41
Mast ME, van Kempen-Harteveld L, Heijenbrok MW et al (2013) Left-sided breast cancer radiotherapy with and without breath-hold: does IMRT reduce the cardiac dose even further? Radiother Oncol 108:248–253
Gaisberger C, Steininger P, Mitterlechner B et al (2013) Three-dimensional surface scanning for accurate patient positioning and monitoring during breast cancer radiotherapy. Strahlenther Onkol 189:887–893
Pili G, Grimaldi L, Fidanza C et al (2011) Geometric and dosimetric approach to determine probability of late cardiac mortality in left tangential breast irradiation: comparison between wedged beams and field-in-field technique. Int J Radiat Oncol Biol Phys 81:894–900
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Hepp, M. Ammerpohl, C. Morgenstern, L. Nielinger, P. Erichsen, A. Abdallah, and R. Galalae state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in study.
Rights and permissions
About this article
Cite this article
Hepp, R., Ammerpohl, M., Morgenstern, C. et al. Deep inspiration breath-hold (DIBH) radiotherapy in left-sided breast cancer. Strahlenther Onkol 191, 710–716 (2015). https://doi.org/10.1007/s00066-015-0838-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0838-y