Abstract
Purpose
To decrease intensive care unit (ICU)-acquired catheter-related infections (CRI), it is essential that healthcare workers receive training and that quality improvement programmes are in place. The aim of our study was to evaluate risk factors for catheter colonisation and infection, focussing specifically on local care bundles.
Methods
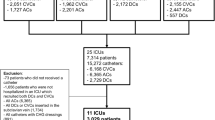
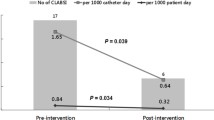
Data were collected prospectively in 51 ICUs [7,188 patients, 8,626 central venous catheters (CVCs)] during two 6-month periods in 2007 and 2008, using a standardized questionnaire on catheter insertion, care and removal. Colonisation and CRI incidence were 6.1 and 2.2/1,000 CVC-days, respectively. A hierarchical mixed logistic model was used to identify risk factors for CRI and colonisation.
Results
Written CVC protocols were available in 46 (90 %) ICUs and were strictly followed in 38 ICUs. Factors significantly associated with CRI fell into three overall categories: (1) patient-related factors—immunosuppression [odds ratio (OR) 1.42, p = 0.02], medical diagnosis at admission (OR 1.64, p = 0.03) and trauma patient (OR 2.54, p < 0.001); (2) catheter-related factors—catheter rank (OR 1.7, p < 0.0001, non-subclavian catheter (OR 2.1, p < 0.001) and longer time with the catheter (p < 10−4); (3) centre-related factors—quantitative tip culture method (OR 2.55, p = 0.005) and alcohol-based povidone-iodine [OR 0.68, 95 % confidence interval (CI) 0.49–0.96] or alcohol-based chlorhexidine preparations (OR 0.69, 95 % CI 0.34–1.39) as compared to an aqueous povidone-iodine preparation (p < 0.001).
Conclusions
We identified several risk factors for CRI that are amenable to improvement (preference for the subclavian route and use of an antiseptic solution containing alcohol). However, several patient-related factors were also found, and the use of quantitative catheter culture methods increased culture sensitivity, thereby increasing the CRI rate. Case-mix issues and the culture method should be taken into account when assessing the risk of CRI across centres.

Similar content being viewed by others
References
Warren DK, Zack JE, Elward AM, Cox MJ, Fraser VJ (2001) Nosocomial primary bloodstream infections in intensive care unit patients in a nonteaching community medical center: a 21-month prospective study. Clin Infect Dis 33:1329–1335
Timsit JF (2005) Updating of the 12th consensus conference of the Societe de Reanimation de langue francaise (SRLF): catheter related infections in the intensive care unit. Ann Fr Anesth Reanim 24:315–322
Timsit JF (2007) Diagnosis and prevention of catheter-related infections. Curr Opin Crit Care 13:563–571
Gastmeier P, Geffers C (2006) Prevention of catheter-related bloodstream infections: analysis of studies published between 2002 and 2005. J Hosp Infect 64:326–335
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355:2725–2732
Timsit JF, Dubois Y, Minet C, Bonadona A, Lugosi M, Ara-Somohano C, Hamidfar-Roy R, Schwebel C (2011) New materials and devices for preventing catheter-related infections. Ann Intensive Care 1:34
Desenclos JC (2009) RAISIN—a national programme for early warning, investigation and surveillance of healthcare-associated infection in France. Euro Surveill 14(46)
Hansen S, Schwab F, Behnke M, Carsauw H, Heczko P, Klavs I, Lyytikainen O, Palomar M, Riesenfeld Orn I, Savey A, Szilagyi E, Valinteliene R, Fabry J, Gastmeier P (2009) National influences on catheter-associated bloodstream infection rates: practices among national surveillance networks participating in the European HELICS project. J Hosp Infect 71:66–73
ECDC (2010) European surveillance of healthcare-associated infections in intensive care units—HAIICU Protocol v1.01. Available at: http://www.ecdc.europa.eu/en/aboutus/calls/Procurement%20Related%20Documents/5_ECDC_HAIICU_protocol_v1_1.pdf
Blakely TA, Woodward AJ (2000) Ecological effects in multi-level studies. J Epidemiol Community Health 54:367–374
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, Dudeck MA, Pollock DA, Horan TC (2009) National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 37:783–805
Lucet JC, Boudama L, Zahar JR, Schwebel C, Geffory A, Pease S, Herault MC, Haouache H, Adrie C, Thuong M, Francais A, Garrouste-Orgeas M, Timsit JF (2010) Infectious risk associated with arterial catheters compared to central venous catheters. Crit Care Med 38:552–559
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S (2011) Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis 52:e162–e193
Badley AD, Steckelberg JM, Wollan PC, Thompson RL (1996) Infectious rates of central venous pressure catheters: comparison between newly placed catheters and those that have been changed. Mayo Clin Proc 71:838–846
L’Heriteau F, Olivier M, Maugat S, Joly C, Merrer J, Thaler F, Grandbastien B, Beaucaire G, Astagneau P (2007) Impact of a five-year surveillance of central venous catheter infections in the REACAT intensive care unit network in France. J Hosp Infect 66:123–129
Timsit JF, Sebille V, Farkas JC, Misset B, Martin JB, Chevret S, Carlet J (1996) Effect of subcutaneous tunneling on internal jugular catheter-related sepsis in critically ill patients: a prospective randomized multicenter study. JAMA 276:1416–1420
Vandecasteele SJ, Van Eldere J, Merckx R, Peetermans WE (2004) The effect of systemic antibiotics on the microbiological diagnosis of experimental foreign body infections caused by Staphylococcus epidermidis. Diagn Microbiol Infect Dis 48:89–95
Souweine B, Heng AE, Aumeran C, Thiolliere F, Gazuy N, Deteix P, Traore O (2008) Do antibiotics administered at the time of central venous catheter removal interfere with the evaluation of colonization? Intensive Care Med 34:286–291
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 49:1–45
Zahar JR, Timsit JF, Garrouste-Orgeas M, Francais A, Vesin A, Descorps-Declere A, Dubois Y, Souweine B, Haouache H, Goldgran-Toledano D, Allaouchiche B, Azoulay E, Adrie C (2011) Outcomes in severe sepsis and patients with septic shock: pathogen species and infection sites are not associated with mortality. Crit Care Med 39:1886–1895
Timsit JF, Schwebel C, Bouadma L, Geffroy A, Garrouste-Orgeas M, Pease S, Herault MC, Haouache H, Calvino-Gunther S, Gestin B, Armand-Lefevre L, Leflon V, Chaplain C, Benali A, Francais A, Adrie C, Zahar JR, Thuong M, Arrault X, Croize J, Lucet JC (2009) Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: a randomized controlled trial. JAMA 301:1231–1241
Rijnders BJ, Van Wijngaerden E, Peetermans WE (2002) Catheter-tip colonization as a surrogate end point in clinical studies on catheter-related bloodstream infection: how strong is the evidence? Clin Infect Dis 35:1053–1058
Timsit JF, Lugosi M, Minet C, Schwebel C (2011) Should we still need to systematically perform catheter culture in the intensive care unit? Crit Care Med 39:1556–1558
Siegman-Igra Y, Anglim AM, Shapiro DE, Adal KA, Strain BA, Farr BM (1997) Diagnosis of vascular catheter-related bloodstream infection: a meta-analysis. J Clin Microbiol 35:928–936
Bouza E, Alvarado N, Alcala L, Sanchez-Conde M, Perez MJ, Munoz P, Martin-Rabadan P, Rodriguez-Creixems M (2005) A prospective, randomized, and comparative study of 3 different methods for the diagnosis of intravascular catheter colonization. Clin Infect Dis 40:1096–1100
Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S (2002) Chlorhexidine compared with povidone-iodine solution for vascular catheter-site care: a meta-analysis. Ann Intern Med 136:792–801
Parienti JJ, du Cheyron D, Ramakers M, Malbruny B, Leclercq R, Le Coutour X, Charbonneau P (2004) Alcoholic povidone-iodine to prevent central venous catheter colonization: a randomized unit-crossover study. Crit Care Med 32:708–713
Mimoz O, Villeminey S, Ragot S, Dahyot-Fizelier C, Laksiri L, Petitpas F, Debaene B (2007) Chlorhexidine-based antiseptic solution vs alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med 167:2066–2072
Edmiston CE Jr, Seabrook GR, Johnson CP, Paulson DS, Beausoleil CM (2007) Comparative of a new and innovative 2 % chlorhexidine gluconate-impregnated cloth with 4 % chlorhexidine gluconate as topical antiseptic for preparation of the skin prior to surgery. Am J Infect Control 35:89–96
Timsit JF (2000) Scheduled replacement of central venous catheters is not necessary. Infect Control Hosp Epidemiol 21:371–374
Safdar N, Kluger DM, Maki DG (2002) A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters: implications for preventive strategies. Medicine (Baltimore) 81:466–479
Deshpande KS, Hatem C, Ulrich HL, Currie BP, Aldrich TK, Bryan-Brown CW, Kvetan V (2005) The incidence of infectious complications of central venous catheters at the subclavian, internal jugular, and femoral sites in an intensive care unit population. Crit Care Med 33:13–20 (Discussion 234–235)
Goetz AM, Wagener MM, Miller JM, Muder RR (1998) Risk of infection due to central venous catheters: effect of site of placement and catheter type. Infect Control Hosp Epidemiol 19:842–845
Parienti JJ, Thirion M, Megarbane B, Souweine B, Ouchikhe A, Polito A, Forel JM, Marque S, Misset B, Airapetian N, Daurel C, Mira JP, Ramakers M, du Cheyron D, Le Coutour X, Daubin C, Charbonneau P (2008) Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA 299:2413–2422
Lorente L, Henry C, Martin MM, Jimenez A, Mora ML (2005) Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care 9:R631–R635
Lorente L, Jimenez A, Garcia C, Galvan R, Castedo J, Martin MM, Mora ML (2008) Catheter-related bacteremia from femoral and central internal jugular venous access. Eur J Clin Microbiol Infect Dis 27:867–871
Acknowledgments
The HAI National Early Warning, Investigation and Surveillance (RAISIN) Working Group is a partnership between the five regional infection control coordinating centres (CLIN), funded by the French Ministry of Health and the National Public Health Surveillance Institute (InVS). REA-RAISIN is a national ICU-acquired infection surveillance network, granted by the InVS. This study was supported by an unrestricted research Grant from Ethicon.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Members of the REA-RAISIN network committee are: P.E. Bollaert (Nancy), R. Gauzit (Paris), D. Gruson, G. Janvier (Bordeaux), T. Lavigne (Strasbourg), A. Lepape (Lyon), P.F. Perrigault (Montpellier), J.F. Timsit (Grenoble), D. Villers (Nantes), S. Boussat, S. Mariani (CClin Est, Nancy), P. Jarno, Nadine Garreau (CClin Ouest, Rennes), F. l’Heriteau, F. Daniel (CClin Paris-Nord, Paris), A. Savey, A. Machut, I. Russell (CClin Sud-Est, Lyon), A.G. Venier, E. Reyrreaud (CClin Sud-Ouest), B. Coignard (InVS, Paris).
Participating local (city) hospitals (in alphabetic order) and investigators of the sub-study were: GARRIGUES Bernard, MARDRUS Philippe (CHG du pays d’Aix, AIX EN PROVENCE); HAUSERMANN Marie Hélène (CH Henri Mondor, AURILLAC); ROYER Daniel, EDE Cyrille (Centre Hospitalier, AUXERRE); COURANT Pierre, MARTIN Régine (CHG Henri Duffaut, AVIGNON); GUERIN Anne-Marie, GUERIN Anne-Marie (CH, BEAUVAIS); SAMAIN Emmanuel, TALON Daniel (CHU, BESANCON); BELLE Evelyne, TALON Daniel (CHU, BESANCON); DHONNEUR Gilles, DURAND Isabelle (Hôpital Jean Verdier, BONDY); LANCON Jean-Pierre, HUMEAU Catherine (Infirmerie Protestante de Lyon, CALUIRE ET CUIRE); ZERR Bernard, DEMANGE Marie (CHG, CHAMBERY); JUST Bernard, (Centre Hospitalier, CHARLEVILLE MEZIERES); BULTEL Jean, PAIRE Marie-Claude (CH, DIGNE LES BAINS); FREYSZ Marc, MILESI-DEFRANCE Nadine (CHU, DIJON); LETELLIER Nicolas, NEVEU Christiane (CH Victor Josselin, DREUX); PAYEN Jean-Francois, DURAND Michel (CHU, GRENOBLE); KEMPF Jean, FRITSCH Hubert (Centre Hospitalier, HAGUENAU); CLAUD Bernard, GAILLARD Michel (CHG Emile Roux, LE PUY EN VELAY); PELERIN Remy, STRUILLOU Laurence (CH Bretagne Sud, LORIENT); GUERIN Claude, BAYLE Frédérique (HCL-Hôpital Croix Rousse, LYON); BAILLON Jean-Jacques, BER Charles Eric (HCL-Hôpital Edouard Herriot, LYON); VIALE Jean-Paul, DUPERRET Serge (HCL-Hôpital Croix Rousse, LYON); ALLAOUCHICHE Bernard, FLOCCARD Bernard (HCL-Hôpital Edouard Herriot, LYON); GUERIN Claude, LERAY Véronique (HCL-Hôpital Croix Rousse, LYON); PUIDUPIN Marc, LIONS Christophe (Hôpital d’Instruction des Armées Desgenettes, LYON); MANCHON Jacques, POMMIER Christian (CH Saint Joseph-Saint Luc, LYON); SEGHBOYAN Jean-Marie, BENICHOUGRANE Nadine (Fondation Hôpital Ambroise Paré, MARSEILLE; MOKART Djamel, BERGER Pierre (Institut J. Paoli-Calmettes, MARSEILLE); OUNIS Nadia ,TURCON Monique (Clinique Vert Coteau, MARSEILLE); MARTIN Claude Denis, WIRAMUS Sandrine (APHM-Hôpital Nord, MARSEILLE; COURTIN Patrick (CHG, MARTIGUES); NICOLA Walid, FOURNIER-HOOCK Régine (CH, MONTARGIS); MILLET Olivier, PONCET Annie (CHG, MONTELIMAR); CHAUSSET Robert (CHG, MONTLUCON); CAPDEVILA Xavier, CHARDON Patrick (CHU-Hôpital Lapeyronie, MONTPELLIER); JONQUET Olivier, CORNE Philippe (CHU-Gui De Chauliac, MONTPELLIER); PERRIGAULT Pierre-François, GENIEZ Chantal (CHU-Gui De Chauliac, MONTPELLIER); CAPRON Matthieu, CAPRON Matthieu (CH de Moulins-Yzeure, MOULINS); CHABOT François, KHEIR Ayman (CHU, NANCY); MEISTELMAN Claude, PERRIER Jean-François (CHU, NANCY); GERARD Alain, THIVILIER Carine (CHU, NANCY); MASSON Bruno, PIQUE Martine (CHG, NARBONNE); GAUZIT Rémy, CASETTA Anne (Hôtel Dieu, PARIS 04EME); RABBAT Antoine, CASETTA Anne (Hôtel Dieu, PARIS 04EME); LEON Alain, LEPOUSE Claire (CHU, REIMS); LEON Alain, SUINAT Jean-Louis (CHU, REIMS); BEURET Pascal, CARTON Marie-Josée (CHG, ROANNE); THIBAUT Freddy, HOFF Jerôme (CH, SAINT-NAZAIRE); CAGNIN Sylvie, CAGNIN Sylvie (Hôpitaux du Mont Blanc, SALLANCHES); MOFREDJ Ali (CHG, SALON DE PROVENCE); JUNGFER-BOUVIER Françoise, GUIGNABERT Catherine (Centre Hospitalier, SENS); JACQUES Luc (CH Intercommunal du Bassin de Thau, SETE); POTTECHER Thierry, LAUNOY Anne (Hôpitaux Universitaire, STRASBOURG); COMBE Christian (CHG, VILLEFRANCHE SUR SAONE).
Rights and permissions
About this article
Cite this article
Timsit, J.F., L‘Hériteau, F., Lepape, A. et al. A multicentre analysis of catheter-related infection based on a hierarchical model. Intensive Care Med 38, 1662–1672 (2012). https://doi.org/10.1007/s00134-012-2645-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2645-6