Abstract
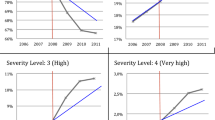
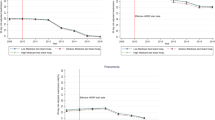
Policy makers have made several attempts to limit hospitals’ upcoding. We investigate the impact of a law introducing a minimum length of stay for discharges with complications. We analyze its effects on the probability of a discharge with complications, on its length of stay and on its reimbursement. We show that the policy has been effective in limiting upcoding, since, after the law, (1) the probability of a discharge with complications has decreased by 3%; (2) its length of stay has risen by 0.17 days more than the observed corresponding variation in the length of stay of a discharge in the control group; (3) the hospital’s revenue on a discharge with complications has decreased by 8.5% more than the observed revenue change on a discharge in the control group. Furthermore, we find evidence of an ownership effect on upcoding, since not-for-profit and for-profit hospitals have been more affected by the law than public hospitals.
Similar content being viewed by others
References
Agency for Healthcare Research and Quality (2008) Healthcare cost and utilization project. Comorbidity Software Version 3.3. http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp
Berta P, Callea G, Martini G, Vittadini G (2010) The effects of upcoding, cream skimming and readmissions on the Italian hospitals efficiency: a population–based investigation. Econ Model 27: 812–821
Besley T, Case A (2000) Unnatural experiments? Estimating the incidence of endogenous policies. Econ J 110: 672–694
Blundell R, McCurdy T (1999) Labor supply: a review of alternative approaches. In: Ashenfelter O, Card D (eds) Handbook of labor economics. Elsevier, Amsterdam
Charlson ME, Pompei P, Ales KA, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373–383
Dafny LS (2005) How do hospitals respond to price changes?. Am Econ Rev 95: 1525–1547
Dafny LS, Dranove D (2009) Regulatory exploitation and management changes: upcoding in the hospital industry. J Law Econ 52: 223–250
de Groot V, Beckerman H, Lankhorst G, Bouter L (2003) How to measure comorbidity: a critical review of available methods. J Clin Epidemiol 56: 221–229
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36: 8–27
Fossati A (2002) Economia Pubblica. Franco Angeli, Milan
GoldsteinH Spiegelhalter DJ (1996) League tables and their limitations: statistical issues in comparison of institutional performance. JRSS Ser A 159(3): 385–443
Heckman J (2005) The scientific model of causality. Sociol Methodol 35: 1–97
Holland PW (1986) Statistics and causal inference. J Am Stat Assoc 81: 945–970
Imbens G, Rubin DB (2009) Causal inference in statistics, and in the social and biomedical sciences. Cambridge University Press, New York
Jin H, Rubin DB (2009) Public schools versus private schools: causal inference with partial compliance. J Educ Behav Stat 34: 24–35
Jones AM (2009) Panel data methods and applications to health economics. In: Mills TC, Patterson K (eds) Palgrave handbook of econometrics. Volume II: applied econometrics. Palgrave MacMillan, Basingstoke
Liu Z, Dow WH, Norton EC (2004) Effect of drive-through delivery laws in postpartum length of stay and hospital charges. J Health Econ 23: 129–155
McClellan M (1997) Hospital reimbursement incentives: an empirical analysis. J Econ Manag Strat 6: 91–128
Mayes R (2007) The origins, development, and passage of Medicare’s revolutionary prospective payment system. J History Med Allied Sci 62: 21–55
Rubin DB (1974) Estimating causal effects of treatments in randomized and nonrandomized studies. J Educ Psychol 66: 688–701
Rubin DB (1975) Bayesian inference for causality: the importance of randomization. In: The Proceedings of the social statistics section of the American Statistical Association, pp 233–239
Rubin DB (1978) Bayesian–inference for causal effects—ole of randomization. Annals of Statistics 6: 34–58
Schneider B, Carnoy M, Kilpatrick J, Schmidt WH, Shavelson RJ (2007) Estimating causal effects using experimental and observational designs a think tank white paper. American Educational Research Association, Washington, DC
Silverman E, Skinner J (2004) Medicare upcoding and hospital ownership. J Health Econ 23: 369–389
Simborg DW (1981) DRG creep: a new hospital-acquired disease. New Engl J Med 304(26): 1602–1604
Southern DA, Quan H, Ghali WA (2004) Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care 42: 355–360
Stuart EA (2007) Estimating causal effects using school-level data sets. Educ Res 36: 187–198
Winship C, Morgan S (2007) Counterfactuals and causal inference. Cambridge University Press, Cambridge
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vittadini, G., Berta, P., Martini, G. et al. The effect of a law limiting upcoding on hospital admissions: evidence from Italy. Empir Econ 42, 563–582 (2012). https://doi.org/10.1007/s00181-012-0548-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00181-012-0548-6