Abstract
Aim
This study had two aims: Firstly, to describe how prescriptions for proton pump inhibitor (PPI) in primary care were influenced by a change of the hospital drug policy, and secondly, to describe if a large discount on an expensive PPI (esomeprazole) to a hospital would influence prescribing patterns after discharge.
Methods
This register study was conducted at Odense University Hospital, Denmark, and by use of pharmacy dispensing data and a hospital-based pharmacoepidemiological database, the medication regimens of patients were followed across hospitalisation. The influence of hospital drug policy on prescribings in primary care was measured by the likelihood of having a high-cost PPI prescribed before and after change of drug policy.
Results
In total, 9,341 hospital stays in 2009 and 2010 were included. The probability of a patient to be prescribed an expensive PPI after discharge decreased from 33.5 to 9.4 %, corresponding to a risk ratio of 0.28. In primary care after discharge, 13.4 % of esomeprazole use was initiated in the hospital, and this was 8.4 % for PPIs in general. After the change of hospital drug policy, this decreased to 6.5 % for esomeprazole and increased for the recommended PPIs pantoprazole and lansoprazole to 14.6 and 26.1 %, respectively. The effect of a large discount on expensive PPI to hospital was 14.7 %, and this decreased to 2.6 % when coordinating drug policy in hospital and primary care.
Conclusion
The likelihood of having an expensive PPI prescribed after hospital stay decreased when coordinating drug policy and the influence of a large discount to hospital could be minimised.


Similar content being viewed by others
References
Godman B, Sakshaug S, Berg C, Wettermark B, Haycox A (2011) Combination of prescribing restrictions and policies to engineer low prices to reduce reimbursement costs. Exp Rev Pharmacoecon Outcome Res 11(1):121–129
Cahir C, Fahey T, Tilson L, Teljeur C, Bennett K (2012) Proton pump inhibitors: potential cost reductions by applying prescribing guidelines. BMC Health Serv Res 12:408
Gray T, Bertch K, Galt K, Gonyeau M, Karpiuk E, Oyen L (2005) Guidelines for therapeutic interchange-2004. Pharmacotherapy 25(11):1666–1680
Godman B, Shrank W, Andersen M, Berg C, Bishop I, Burkhardt T, Garuoliene K, Herholz H, Joppi R, Kalaba M, Laius O, McGinn D, Samaluk V, Sermet C, Schwabe U, Teixeira I, Tilson L, Tulunay FC, Vlahović-Palčevski V, Wendykowska K, Wettermark B, Zara C, Gustafsson LL (2010) Comparing policies to enhance prescribing efficiency in Europe through increasing generic utilization: changes seen and global implications. Exp Rev Pharmacoecon Outcome Res 10(6):707–722
Godman B, Shrank W, Andersen M, Berg C, Bishop I, Burkhardt T, Garuoliene K, Herholz H, Joppi R, Kalaba M, Laius O, Lonsdale J, Malmström RE, Martikainen JE, Samaluk V, Sermet C, Schwabe U, Teixeira I, Tilson L, Tulunay FC, Vlahović-Palčevski V, Wendykowska K, Wettermark B, Zara C, Gustafsson LL (2010) Policies to enhance prescribing efficiency in Europe: findings and future implications. Front Pharmacol 1:141
Wettermark B, Godman B, Jacobsson B, Haaijer-Ruskamp FM (2009) Soft regulations in pharmaceutical policy making: an overview of current approaches and their consequences. Appl Health Econ Health Policy 7(3):137–147
Plet HT, Hallas J, Nielsen GS, Kjeldsen LJ (2013) Drug and therapeutics committees in Danish hospitals: a survey of organization, activities and drug selection procedures. Basic Clin Pharmacol Toxicol 112(4):264–269
Mittmann N, Knowles S (2009) A survey of pharmacy and therapeutic committees across Canada: scope and responsibilities. Can J Clin Pharmacol 16(1):e171–e177
Reynolds DJ, Fajemisin O, Wilds S (2012) Local formularies. Br J Clin Pharmacol 74(4):640–643
Florentinus SR, Heerdink ER, van Dijk L, Griens AM, Groenewegen PP, Leufkens HG (2009) Is new drug prescribing in primary care specialist induced? BMC Health Serv Res 9:6
Jones MI, Greenfield SM, Jowett S, Bradley CP, Seal R (2001) Proton pump inhibitors: a study of GPs’ prescribing. Fam Pract 18(3):333–338
Robertson J, Fryer JL, O’Connell DL, Sprogis A, Henry DA (2001) The impact of specialists on prescribing by general practitioners. Med J Aust 175(8):407–411
Prosser H, Almond S, Walley T (2003) Influences on GPs’ decision to prescribe new drugs-the importance of who says what. Fam Pract 20(1):61–68
Jones MI, Greenfield SM, Bradley CP (2001) Prescribing new drugs: qualitative study of influences on consultants and general practitioners. BMJ 323(7309):378–381
Grimmsmann T, Schwabe U, Himmel W (2007) The influence of hospitalisation on drug prescription in primary care—a large-scale follow-up study. Eur J Clin Pharmacol 63(8):783–790
Cochrane RA, Mandal AR, Ledger-Scott M, Walker R (1992) Changes in drug treatment after discharge from hospital in geriatric patients. BMJ 305(6855):694–696
Viktil KK, Blix HS, Eek AK, Davies MN, Moger TA, Reikvam A (2012) How are drug regimen changes during hospitalisation handled after discharge: a cohort study. BMJ Open 2(6)
Krag A, Teglbjerg LS, Malchow-Moller A, Hallas J, Bytzer P (2006) Prescribing of acid suppressive therapy: interactions between hospital and primary care. Aliment Pharmacol Ther 23(12):1713–1718
Ahrens D, Behrens G, Himmel W, Kochen MM, Chenot JF (2012) Appropriateness of proton pump inhibitor recommendations at hospital discharge and continuation in primary care. Int J Clin Pract 66(8):767–773
Buck TC, Hallas J, Broesen K (2010) [Status og visioner for HEKLA 2010]. Status and vision. Hospital Section for Quality of Drug Use, 2010. Odense University Hospital
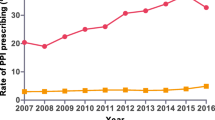
Danish State Serum Institute. Statistics on the total sales of medicines in Denmark 1996–2012, http://www.medstat.dk/en, April 2013
Institute for Rational Pharmacotherapy. PPI prevent NSAID-induced gastroduodenal ulcers [Protonpumpehæmmer forebygger NSAID-udløst maveblødning], April 2013
Odense University Hospital http://www.ouh.dk/wm197174/ Marts 2013
Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44(4):445–448
WHO Collaborating Centre for Drug Statistics Methodology (2010) Guidelines for ATC classification and DDD assignment 2011. Norwegian Institute of Public Health, Oslo
Epidemiology FL (2000) When an entire country is a cohort. Science 287(5462):2398–2399
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39(7 Suppl):22–25
Johannesdottir SA, Maegbaek ML, Hansen JG, Lash TL, Pedersen L, Ehrenstein V (2012) Correspondence between general practitioner reported medication use and timing of prescription dispensation. Clin Epidemiol 4:13–18
Lau HS, de Boer A, Beuning KS, Porsius A (1997) Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol 50(5):619–625
Andrade SE, Kahler KH, Frech F, Chan KA (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15(8):565–574, discussion 75–7
Steiner JF, Prochazka AV (1997) The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol 50(1):105–116
Conflict of interest
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that Jesper Hallas has participated in research projects funded by Nycomed, the manufacturer of pantoprazole, and AstraZeneca, the manufacturer of Nexium (esomeprazole) and, with grants paid to institutions where they have been employed. Jesper Hallas has personally received fees for teaching from Nycomed and consulting from the Danish Association of Pharmaceutical Manufacturers.
Michael Due Larsen, Mette Schou and Anja Sparre Kristiansen declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Larsen, M.D., Schou, M., Kristiansen, A.S. et al. The influence of hospital drug formulary policies on the prescribing patterns of proton pump inhibitors in primary care. Eur J Clin Pharmacol 70, 859–865 (2014). https://doi.org/10.1007/s00228-014-1681-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-014-1681-2