Abstract
Purpose
Drug-drug interactions (DDIs) are often avoidable and, if undetected, can lead to patient harm. This review aimed to determine the prevalence of potential DDIs (pDDIs), clinically relevant DDIs (DDIs that could lead to measurable patient harm, taking into account the patient’s individual clinical profile) and DDIs that resulted in actual patient harm during hospitalisation.
Method
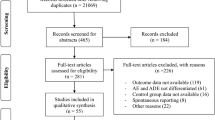
Four databases were scanned for English papers published from 2000 to 2016. Papers that reported prevalence of DDIs in the outpatient setting, at admission or discharge, involving only specific drugs, or in specific disease populations or age groups were excluded.
Results
Twenty-seven papers met the inclusion criteria and were graded for quality using the Critical Appraisal Skills Programme (CASP) cohort study checklist. Ten papers were rated as ‘poor’, 14 as ‘fair’ and only three papers as ‘good’. Overall, the meta-analysis revealed that 33% of general patients and 67% of intensive care patients experienced a pDDI during their hospital stay. It was not possible to determine the prevalence of clinically relevant DDIs or DDIs that resulted in actual patient harm as data on these categories were limited. Of the very few studies that reported on harm, only a small proportion of DDIs were found to have resulted in actual patient harm.
Conclusions
Standardisation of DDI definitions and research methods are required to allow meaningful prevalence rates to be obtained and compared. Studies that go further than measuring pDDIs are critically needed to determine the impact of DDIs on patient safety.


Similar content being viewed by others
References
Dechanont S et al (2014) Hospital admissions/visits associated with drug-drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf 23(5):489–497
Hines LE, Murphy JE (2011) Potentially harmful drug-drug interactions in the elderly: a review. Am J Geriatric Pharmacotherapy 9(6):364–377
Peyriere H et al (2003) Adverse drug events associated with hospital admission. Ann Pharmacother 37(1):5–11
Reis AMM, Cassiani SHB (2011) Prevalence of potential drug interactions in patients in an intensive care unit of a university hospital in Brazil. Clinics 66(1):9–15
Wright A et al (2012) Preventability of adverse drug events involving multiple drugs using publicly available clinical decision support tools. Am J Health Syst Pharm 69(3):221–227
Hines LE et al (2011) Critical issues associated with drug-drug interactions: highlights of a multistakeholder conference. Am J Health Syst Pharm 68(10):941–946. https://doi.org/10.2146/ajhp100440
Espinosa-Bosch M et al (2012) Prevalence of drug interactions in hospital healthcare. Int J Clin Pharm 34(6):807–817
Moura CS, Acurcio FA, Belo NO (2009) Drug-drug interactions associated with length of stay and cost of hospitalization. J Pharm Pharm Sci 12(3):266–272
Shad MU, Marsh C, Preskorn SH (2001) The economic consequences of a drug-drug interaction. J Clin Psychopharmacol 21(1):119–120
Bucsa C et al (2013) How many potential drug-drug interactions cause adverse drug reactions in hospitalized patients? Eur J Intern Med 24(1):27–33
Moura C, Prado N, Acurcio F (2011) Potential drug-drug interactions associated with prolonged stays in the intensive care unit: a retrospective cohort study. Clin Drug Investig 31(5):309–316
Becker ML et al (2007) Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf 16(6):641–651
Abideen S, Vivekanandan K, Mishra P (2015) Assessment of prevalence of potential drug-drug interactions in medical intensive care unit of a tertiary care hospital in India. Asian J Pharmaceutical Clinical Res 8(1):125–130
Kumara Swamy RC et al (2014) Prevalence of polypharmacy and drug to drug interactions in a tertiary care teaching hospital. Int Res J Pharmacy 5(10):778–782
Ogata K et al (2014) Polypharmacy in elderly cancer patients. Ann Oncol 25:v100
Sancar M et al (2011) Identification potential drug-drug interaction in elderly patients receiving polypharmacy prescription. Int J Clin Pharm 33(2):407
Sharifi H, Hasanloei MAV, Mahmoudi J (2014) Polypharmacy-induced drug-drug interactions; threats to patient safety. Drug Res 64(12):633–637
Sindhu MS, Kannan B (2013) Investigating the factors affecting drug-drug interactions. Int J Pharm Bio Sci 4(4):P467–P476
Lima RE, De Bortoli Cassiani SH (2009) Potential drug interactions in intensive care patients at a teaching hospital. Rev Lat Am Enfermagem 17(2):222–227
Lubinga SJ, Uwiduhaye E (2011) Potential drug-drug interactions on in-patient medication prescriptions at Mbarara Regional Referral Hospital (MRRH) in western Uganda: prevalence, clinical importance and associated factors. Afr Health Sci 11(3):499–507
Radozevic N, Gantumur M, Vlahovic-Palcevski V (2008) Potentially inappropriate prescribing to hospitalised patients. Pharmacoepidemiol Drug Saf 17(7):733–737
Reimche L, Forster AJ, van Walraven C (2011) Incidence and contributors to potential drug-drug interactions in hospitalized patients. J Clin Pharmacol 51(7):1043–1050
Bertsche T et al (2010) Prevention of adverse drug reactions in intensive care patients by personal intervention based on an electronic clinical decision support system. Intensive Care Med 36(4):665–672
Classen DC, Phansalkar S, Bates DW (2011) Critical drug-drug interactions for use in electronic health records systems with computerized physician order entry: review of leading approaches. J Patient Saf 7(2):61–65
Saxena K, Lung BR, Becker JR (2011) Improving patient safety by modifying provider ordering behavior using alerts (CDSS) in CPOE system. AMIA Annual Symposium Proceedings, 2011, p 1207–1216
van der Sijs H et al (2006) Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc 13(2):138–147
Bryant AD, Fletcher GS, Payne TH (2014) Drug interaction alert override rates in the Meaningful Use era: no evidence of progress. Appl Clin Inform 5(3):802–813
Ko Y et al (2007) Practitioners’ views on computerized drug-drug interaction alerts in the VA system. J Am Med Inform Assoc 14(1):56–64
Chiatti C et al (2012) The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people a systematic review. Drug Saf 35(Suppl. 1):73–87
Gnjidic D, Johnell K (2013) Clinical implications from drug-drug and drug-disease interactions in older people. Clinical Experimental Pharmacol Physiol 40(5):320–325
(CASP), C.A.S.P. CASP checklists. 2013 [cited 2017 10th January]; Available from: http://www.casp-uk.net/checklists
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Stat 21(4):607–611
Knapp G, Hartung J (2003) Improved tests for a random effects meta-regression with a single covariate. Stat Med 22(17):2639–2710
Higgins JPT, Thompson SG, Deeks JJ (2003) Measuring inconsistency in meta-analysis. BMJ 327(7414):557–560
Egger M, Davey Smith G, Schneider M (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
R Development Core Team, R (2013) a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Al-Hajje A et al (2012) Medication prescribing errors: data from seven Lebanese hospitals. Le Journal medical libanais. Lebanese Medical J 60(1):37–44
Amin A et al (2011) Review of prescriber approach towards rational drug practice in hospitalised patients. J Ayub Medical College, Abbottabad: JAMC 23(1):19–22
Blix HS et al (2004) The majority of hospitalised patients have drug-related problems: results from a prospective study in general hospitals. Eur J Clin Pharmacol 60(9):651–658
Ismail M et al (2013) Potential drug-drug interactions in internal medicine wards in hospital setting in Pakistan. Int J Clin Pharm 35(3):455–462
Kaliamurthy K et al (2015) Study of drug-drug interactions in general medicine department of a tertiary care hospital. J Appl Pharmaceutical Sci 5(12):122–124
Oertle, M., Frequency and nature of drug-drug interactions in a Swiss primary and secondary acute care hospital. Swiss Medical Weekly, 2012. 142 (February) (no pagination) (w13522)
Pote S, Tiwari P, D'Cruz S (2007) Medication prescribing errors in a public teaching hospital in India: a prospective study. Pharm Pract (Granada) 5(1):17–20
Soherwardi S, Chogtu B, Faizal P (2012) Surveillance of the potential drug-drug interactions in the medicine department of a tertiary care hospital. J Clin Diagn Res 6(7 Suppl):1258–1261
Tigabu B, Daba D, Habte B (2014) Drug-related problems among medical ward patients in Jimma University specialized hospital, Southwest Ethiopia. J Res Pharmacy Practice 3(1):1–5
van Doormaal JE et al (2010) Comparison of methods for identifying patients at risk of medication-related harm. Qual Saf Health Care 19(6):e26
Vonbach P et al (2008) Prevalence of drug-drug interactions at hospital entry and during hospital stay of patients in internal medicine. European J Internal Med 19(6):413–420
Vrca VB et al (2005) Prescribing medication errors in hospitalised patients: a prospective study. Acta Pharma 55(2):157–167
Zwart-Van Rijkom JEF et al (2009) Frequency and nature of drug-drug interactions in a Dutch university hospital. Br J Clin Pharmacol 68(2):187–193
Bista DB et al (2009) Pattern of potential drug-drug interactions in the intensive care unit of a teaching hospital in Nepal: a pilot study. J Clin Diagn Res 3(4):1713–1716
Cruciol-Souza JM, Ferreira-Filho OF, Obreli-Neto PR (2012) Prevalence of potential drug-drug interactions in an intensive care unit at a Brazilian hospital. Lat Am J Pharm 31(10):1469–1475
Rodrigues AT et al (2015) Clinical relevancy and risks of potential drug-drug interactions in intensive therapy. Saudi Pharmaceutical J 23(4):366–370
Smithburger PL, Kane-Gill SL, Seybert AL (2012) Drug-drug interactions in the medical intensive care unit: an assessment of frequency, severity and the medications involved. Int J Pharmacy Practice 20(6):402–408
Uijtendaal EV et al (2014) Analysis of potential drug-drug interactions in medical intensive care unit patients. Pharmacotherapy 34(3):213–219
IUGG. List of developing countries. 2015 [cited 2017 17 February 2017]; Available from: http://www.iugg2015prague.com/list-of-developing-countries.htm
Ammenwerth E et al (2008) The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc 15(5):585–600. https://doi.org/10.1197/jamia.M2667 Epub 2008 Jun 25
Radley DC et al (2013) Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. J Am Med Inform Assoc 20(3):470–476. https://doi.org/10.1136/amiajnl-2012-001241
Shamliyan TA et al (2008) Just what the doctor ordered. Review of the evidence of the impact of computerized physician order entry system on medication errors. Health Serv Res 43(1 Pt 1):32–53. https://doi.org/10.1111/j.1475-6773.2007.00751.x
Westbrook JI et al (2013) The safety of electronic prescribing: manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals. J Am Med Inform Assoc 20(6):1159–1167
Weingart SN et al (2003) Physicians’ decisions to override computerized drug alerts in primary care. Arch Intern Med 163(21):2625–2631
Lyell D, Coiera E (2017) Automation bias and verification complexity: a systematic review. J Am Med Inform Assoc 24(2):423–431. https://doi.org/10.1093/jamia/ocw105
Vanham D et al (2017) Drug-drug interactions in the intensive care unit: do they really matter. J Crit Care 38:97–103. https://doi.org/10.1016/j.jcrc.2016.09.014
Alyamani NA, Hopf Y, Williams DJ (2009) Prescription quality in an acute medical ward. Pharmacoepidemiol Drug Saf 18(12):1158–1165
Contributions of authors statement
WYZ was responsible for the conception of the work, data collection, data analysis and interpretation and drafting of the manuscript. LR was responsible for data collection, data analysis and interpretation and critical revision of the manuscript. LL was responsible for data analysis and interpretation. RD was responsible for conception of the work and critical revision of the manuscript. JW was responsible for conception of the work and critical revision of the manuscript. MB was responsible for conception of the work, data analysis and interpretation and critical revision of the manuscript.
Funding
This review was funded by the Australian National Health and Medical Research Council Program Grant no. 1054146.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 72 kb)
Rights and permissions
About this article
Cite this article
Zheng, W.Y., Richardson, L.C., Li, L. et al. Drug-drug interactions and their harmful effects in hospitalised patients: a systematic review and meta-analysis. Eur J Clin Pharmacol 74, 15–27 (2018). https://doi.org/10.1007/s00228-017-2357-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2357-5