Abstract
Background
Dipyrone comedication in aspirin-treated patients is associated with impaired pharmacodynamic response to aspirin (high on-treatment platelet reactivity [HTPR]). Additionally, in small observational studies, an association with impaired outcome has been described. In this uncontrolled, hypothesis-generating study, we aimed to investigate strategies to prevent this drug-drug interaction in patients with coronary artery disease (CAD).
Methods
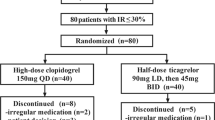
We analyzed pharmacodynamic response to aspirin in 80 dipyrone co-medicated CAD patients. Aspirin antiplatelet effects were measured using arachidonic acid (AA)-induced light-transmission aggregometry (LTA). Platelet reactivity was associated with daily dose, administration form, and frequency. Additionally, we conducted a time-series analysis in patients with HTPR to aspirin with re-evaluation of pharmacodynamic response to aspirin after 5 days.
Results
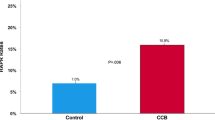
Patients’ mean age was 75.5 ± 9.8 years. Forty-three (54%) were male, 22 (27.5%) obese, and 38 (47.5%) diabetics. Baseline characteristics, cardiovascular risk factors, comorbidities, comedication, or laboratory parameters did not differ between patients with or without HTPR. HTPR to aspirin occurred in 34 out of 80 patients (42.5%). The incidence of HTPR was associated with dipyrone daily dose (< 1 g/day: HTPR 20% vs. > 3 g/day: HTPR 50%, p > 0.0001) and form of administration (i.v. 87.5% vs. oral 37.5%; p < 0.0001). A strict order of intake (aspirin 30 min prior to dipyrone) restored aspirin antiplatelet effects in all patients (HTPR before 100% vs. HTPR after 0%, p = 0.0002).
Conclusion
This study shows that dipyrone should be used with caution in aspirin-treated patients. If dipyrone seems indispensable, the lowest effective dose and a strict order of intake seem favorable.




Similar content being viewed by others
Abbreviations
- AA:
-
Arachidonic acid
- ACE:
-
Angiotensine converting enzyme
- AT II:
-
Angiotensin II
- Ca:
-
Calcium
- CABG:
-
Coronary bypass grafting
- COPD:
-
Chronic obstructive pulmonary disease
- CAD:
-
Chronic artery disease
- CKD:
-
Chronic kidney disease
- COX:
-
Cyclooxygenase
- GFR:
-
Glomerular filtration rate
- HDL:
-
High density lipoprotein
- HTPR:
-
High on-treatment platelet reactivity
- LDL:
-
Low-density lipoprotein
- LTA:
-
Light transmission aggregometry
- MACCE:
-
Major adverse cardiac and cerebrovascular events
- MI:
-
Myocardial infarction
- MoA:
-
Maximum of aggregation
- PCI:
-
Percutaneous coronary intervention
- S.D.:
-
Standard deviation
- TG:
-
Triglyceride
- T½:
-
Half-life
References
Gislason GH, Jacobsen S, Rasmussen JN, Rasmussen S, Buch P, Friberg J, Schramm TK, Abildstrom SZ, Køber L, Madsen M, Torp-Pedersen C (2006) Risk of death or reinfarction associated with the use of selective cyclooxygenase-2 inhibitors and nonselective nonsteroidal antiinflammatory drugs after acute myocardial infarction. Circulation 113(25):2906–2913
Laporte JR, Ibanez L, Vidal X, Vendrell L, Leone R (2004) Upper gastrointestinal bleeding associated with the use of NSAIDs: newer versus older agents. Drug Saf 27(6):411–420
Arellano F, Sacristan JA (1990) Metamizole: reassessment of its therapeutic role. Eur J Clin Pharmacol 38(6):617–619
Schwabe UP (2014) Deutscher Arzneiverordnungsreport 2014: Aktuelle Daten, Kosten, Trends und Kommentare. Dieter Paffrath
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K et al (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the heart failure association (HFA) of the ESC. Eur J Heart Fail 14(8):803–869
Fine RL (2007) Ethical and practical issues with opioids in life-limiting illness. Proc (Bayl Univ Med Cent) 20(1):5–12
Schmidt M, Sorensen HT, Pedersen L (2018) Diclofenac use and cardiovascular risks: series of nationwide cohort studies. BMJ 362:k3426
Lamberts M, Lip GY, Hansen ML, Lindhardsen J, Olesen JB, Raunso J et al (2014) Relation of nonsteroidal anti-inflammatory drugs to serious bleeding and thromboembolism risk in patients with atrial fibrillation receiving antithrombotic therapy: a nationwide cohort study. Ann Intern Med 161(10):690–698
Lamberts M, Fosbol EL, Olsen AM, Hansen ML, Folke F, Kristensen SL et al (2013) Ongoing treatment with non-steroidal anti-inflammatory drugs at time of admission is associated with poorer prognosis in patients with first-time acute myocardial infarction. Int J Cardiol 168(2):832–837
Schmidt M, Lamberts M, Olsen AM, Fosboll E, Niessner A, Tamargo J et al (2016) Cardiovascular safety of non-aspirin non-steroidal anti-inflammatory drugs: review and position paper by the working group for cardiovascular pharmacotherapy of the European Society of Cardiology. Eur Heart J 37(13):1015–1023
Schjerning Olsen AM, Gislason GH, McGettigan P, Fosbol E, Sorensen R, Hansen ML et al (2015) Association of NSAID use with risk of bleeding and cardiovascular events in patients receiving antithrombotic therapy after myocardial infarction. JAMA 313(8):805–814
Gerd Glaeske CS (2015) BARMER GEK Arzneimittelreport 2015. Barmer GEK
Athanasiadis A, Sechtem U, European Society of Cardiology (2014) Diagnostics and therapy of chronic stable coronary artery disease: new guidelines of the European Society of Cardiology. Herz 39(8):902–912
Berger JS, Brown DL, Becker RC (2008) Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. Am J Med 121(1):43–49
Pamukcu B (2007) A review of aspirin resistance; definition, possible mechanisms, detection with platelet function tests, and its clinical outcomes. J Thromb Thrombolysis 23(3):213–222
Polzin A, Afzal S, Balzer J, Rassaf T, Kelm M, Zeus T (2016) Platelet reactivity in MitraClip patients. Vasc Pharmacol 77:54–59
Polzin A, Schleicher M, Seidel H, Scharf RE, Merx MW, Kelm M, Zeus T (2015) High on-treatment platelet reactivity in transcatheter aortic valve implantation patients. Eur J Pharmacol 751:24–27
Polzin A, Dannenberg L, Sophia Popp V, Kelm M, Zeus T (2016) Antiplatelet effects of clopidogrel and aspirin after interventional patent foramen ovale/ atrium septum defect closure. Platelets 27(4):317–321
Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (2008) Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ 336(7637):195–198
Polzin A, Richter S, Schror K, Rassaf T, Merx MW, Kelm M et al (2015) Prevention of dipyrone (metamizole) induced inhibition of aspirin antiplatelet effects. Thromb Haemost 114(1):87–95
Polzin A, Dannenberg L, Sansone R, Levkau B, Kelm M, Hohlfeld T, Zeus T (2016) Antiplatelet effects of aspirin in chronic kidney disease patients. J Thromb Haemost 14(2):375–380
Polzin A, Zeus T, Schror K, Kelm M, Hohlfeld T (2013) Dipyrone (metamizole) can nullify the antiplatelet effect of aspirin in patients with coronary artery disease. J Am Coll Cardiol 62(18):1725–1726
Dannenberg L, Erschoff V, Bonner F, Gliem M, Jander S, Levkau B et al (2016) Dipyrone comedication in aspirin treated stroke patients impairs outcome. Vasc Pharmacol 87:66–69
Achilles A, Mohring A, Dannenberg L, Piayda K, Levkau B, Hohlfeld T, Zeus T, Kelm M, Polzin A (2017) Analgesic medication with dipyrone in patients with coronary artery disease: relation to MACCE. Int J Cardiol 236:76–81
Gurney D (2016) Platelet function testing: from routine to specialist testing. Br J Biomed Sci 73(1):10–20
Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ (2003) A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol 41(6):961–965
Breet NJ, van Werkum JW, Bouman HJ, Kelder JC, Ten Berg JM, Hackeng CM (2010) High on-aspirin platelet reactivity as measured with aggregation-based, cyclooxygenase-1 inhibition sensitive platelet function tests is associated with the occurrence of atherothrombotic events. J Thromb Haemost 8(10):2140–2148
Lim ST, Coughlan CA, Murphy SJ, Fernandez-Cadenas I, Montaner J, Thijs V et al (2015) Platelet function testing in transient ischaemic attack and ischaemic stroke: a comprehensive systematic review of the literature. Platelets 26(5):402–412
Whelton A (1999) Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Am J Med 106(5B):13S–24S
Polzin A, Hohlfeld T, Kelm M, Zeus T (2015) Impairment of aspirin antiplatelet effects by non-opioid analgesic medication. World J Cardiol 7(7):383–391
Catella-Lawson F, Reilly MP, Kapoor SC, Cucchiara AJ, DeMarco S, Tournier B, Vyas SN, FitzGerald GA (2001) Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med 345(25):1809–1817
Levy M, Zylber-Katz E, Rosenkranz B (1995) Clinical pharmacokinetics of dipyrone and its metabolites. Clin Pharmacokinet 28(3):216–234
Flusser D, Zylber-Katz E, Granit L, Levy M (1988) Influence of food on the pharmacokinetics of dipyrone. Eur J Clin Pharmacol 34(1):105–107
Bromet EJ, Dunn LO, Connell MM, Dew MA, Schulberg HC (1986) Long-term reliability of diagnosing lifetime major depression in a community sample. Arch Gen Psychiatry 43(5):435–440
Sibbing D, Aradi D, Jacobshagen C, Gross L, Trenk D, Geisler T, Orban M, Hadamitzky M, Merkely B, Kiss RG, Komócsi A, Dézsi CA, Holdt L, Felix SB, Parma R, Klopotowski M, Schwinger RHG, Rieber J, Huber K, Neumann FJ, Koltowski L, Mehilli J, Huczek Z, Massberg S, Parma R, Parma Z, Lesiak M, Komosa A, Huczek Z, Koltowski L, Kowara M, Rymuza B, Klopotowski M, Malek L, Aradi D, Veress G, Dézsi AD, Merkely B, Lux Á, Kiss RG, Papp J, Kovács A, Dézsi CA, Amer S, Ruzsa Z, Róna S, Komócsi A, Ili R, Ungi I, Nagy F, Zweiker R, Tóth-Gayor G, Huber K, Haller P, von Scheidt W, Blüthgen A, Neumann FJ, Trenk D, Leggewie S, Kreider-Stempfle HU, Remp T, Kara K, Mügge A, Wutzler A, Fichtlscherer S, Zeiher AM, Seeger F, Hinterseer M, König A, Lederle S, Jacobshagen C, Czepluch F, Maier L, Schillinger W, Sossalla S, Hummel A, Felix S, Karakas M, Sydow K, Rudolph T, Halbach M, Gori T, Münzel T, May A, Gerstenberg CM, Pilecky D, Rieber J, Deichstetter M, Sibbing D, Mehilli J, Gross L, Kääb S, Löw A, Orban M, Orban M, Sattler S, Deuschl S, Teupser D, Holdt L, Mudra H, Räder T, Schütz T, Vahldiek F, Divchev D, Ince H, Nienaber CA, Radunski H, Boekstegers P, Horstkotte J, Mueller R, Geisler T, Müller K, Schwinger R, Rasp O (2017) Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. In: Lancet, vol 390, pp 1747–1757
Trenk D, Stone GW, Gawaz M, Kastrati A, Angiolillo DJ, Muller U et al (2012) A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (testing platelet reactivity in patients undergoing elective stent placement on Clopidogrel to guide alternative therapy with Prasugrel) study. J Am Coll Cardiol 59(24):2159–2164
Gurbel PA, Price MJ, Dahlen JR, Tantry US (2017) ANTARCTIC: platelet function testing to adjust therapy. Lancet 389(10075):1193
Cayla G, Cuisset T, Silvain J, Leclercq F, Manzo-Silberman S, Saint-Etienne C, Delarche N, Bellemain-Appaix A, Range G, el Mahmoud R, Carrié D, Belle L, Souteyrand G, Aubry P, Sabouret P, du Fretay XH, Beygui F, Bonnet JL, Lattuca B, Pouillot C, Varenne O, Boueri Z, van Belle E, Henry P, Motreff P, Elhadad S, Salem JE, Abtan J, Rousseau H, Collet JP, Vicaut E, Montalescot G (2016) Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): an open-label, blinded-endpoint, randomised controlled superiority trial. Lancet 388(10055):2015–2022
Collet JP, Cayla G, Cuisset T, Elhadad S, Range G, Vicaut E et al (2011) Randomized comparison of platelet function monitoring to adjust antiplatelet therapy versus standard of care: rationale and design of the assessment with a double randomization of (1) a fixed dose versus a monitoring-guided dose of aspirin and clopidogrel after DES implantation, and (2) treatment interruption versus continuation, 1 year after stenting (ARCTIC) study. Am Heart J 161(1):5–12 e5
Price MJ, Angiolillo DJ, Teirstein PS, Lillie E, Manoukian SV, Berger PB, Tanguay JF, Cannon CP, Topol EJ (2011) Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention: a time-dependent analysis of the gauging responsiveness with a VerifyNow P2Y12 assay: impact on thrombosis and safety (GRAVITAS) trial. Circulation 124(10):1132–1137
Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A et al (2017) ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J:2017
Simpson SH, Abdelmoneim AS, Omran D, Featherstone TR (2014) Prevalence of high on-treatment platelet reactivity in diabetic patients treated with aspirin. Am J Med 127(1):95.e1–95.e9
Patrono C, Rocca B (2017) Type 2 diabetes, obesity, and aspirin responsiveness. J Am Coll Cardiol 69(6):613–615
Rothwell PM, Cook NR, Gaziano JM, Price JF, Belch JFF, Roncaglioni MC, Morimoto T, Mehta Z (2018) Effects of aspirin on risks of vascular events and cancer according to bodyweight and dose: analysis of individual patient data from randomised trials. Lancet 392(10145):387–399
Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Baggish JS, Bhatt DL, Topol EJ (2005) Analysis of risk of bleeding complications after different doses of aspirin in 192,036 patients enrolled in 31 randomized controlled trials. Am J Cardiol 95(10):1218–1222
Simon LS, Weaver AL, Graham DY, Kivitz AJ, Lipsky PE, Hubbard RC, Isakson PC, Verburg KM, Yu SS, Zhao WW, Geis GS (1999) Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA 282(20):1921–1928
Acknowledgments
The authors thank Kirsten Bartkowski for experimental support.
Funding
This work was supported by the Forschungskommission of the Medical Faculty of the Heinrich Heine University (No. 46-2016, to L.D., No. 16-2014 to A.P.).
Author information
Authors and Affiliations
Contributions
L.D., T.P., and A.A. designed the study, analyzed, and interpreted data and wrote the manuscript. D.N., S.Z., C.H., R.M., and P.M. collected data and revised the manuscript. A.P., T.H., M.K., T.Z., B.L., M.G., and Y.P. supervised the study and revised the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study conformed to the Declaration of Helsinki and was approved by the University of Düsseldorf Ethics Committee.
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Dannenberg, L., Petzold, T., Achilles, A. et al. Dose reduction, oral application, and order of intake to preserve aspirin antiplatelet effects in dipyrone co-medicated chronic artery disease patients. Eur J Clin Pharmacol 75, 13–20 (2019). https://doi.org/10.1007/s00228-018-2560-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-2560-z