Abstract
Purpose
To investigate statin use in the elderly by age (≥ 80 vs. 65–79 years) in relation to established indications.
Methods
A population-based cohort, including data from four registers, encompassing inhabitants in Region Västra Götaland, Sweden, was used. Statin users were defined as those filling statin prescriptions ≥ 75% of the year 2010. Primary care and hospital diagnoses in 2005–2010 regarding ischemic heart disease, stroke, transient ischemic attacks, and diabetes were considered established indications.
Results
A total of 278,205 individuals were analyzed. In individuals aged ≥ 80 and 65–79 years (n = 81,885 and n = 196,320, respectively), 17% (95% confidence interval 17%; 18%) and 23% (23%; 23%) respectively, were statin users. Among the statin users, 74% (73%; 74%) of those aged ≥ 80 and 60% (59%; 60%) of those aged 65–79 years had ≥ 1 established indication. Conversely, of those with ≥ 1 established indication, 30% (30%; 31%) and 53% (52%; 53%) were on statins in the respective age groups. Logistic regression revealed that age, nursing home residence, and multi-dose drug dispensing were the most prominent negative predictors for statin use; adjusted odds ratios (95% confidence interval): 0.45 (0.44; 0.46), 0.39 (0.36; 0.42), and 0.47 (0.44; 0.49), respectively.
Conclusions
In the oldest old (≥ 80 years), statin users were fewer and had more often an established indication, suggesting that physicians extrapolate scientific evidence for beneficial effects in younger age groups to the oldest, but require a more solid ground for treatment. As the oldest old, nursing home residents, and those with multi-dose drug-dispensing were statin users to a lesser extent, physicians may often refrain from treatment in those with lower life expectancy, either due to age or to severely reduced health status. In both age groups, our results however also indicate some over- as well as undertreatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Statins are effective in reducing major vascular events such as myocardial infarction and stroke. Guidelines from the American College of Cardiology/American Heart Association (ACC/AHA) as well as the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) currently recommend statin treatment for secondary prevention in individuals with established cardiovascular disease because of convincing evidence of positive effects in several randomized controlled trials (RCTs) [1,2,3,4,5]. The guidelines also recommend statins for primary prevention in individuals with diabetes and in those with a high or very high estimated cardiovascular risk [4, 5].
The absolute benefit of statin treatment depends on the baseline risk which can be estimated from age, sex, and cardiovascular risk factors [4,5,6]. To facilitate treatment decisions, the Systematic Coronary Risk Evaluation (SCORE) system has been developed, illustrating the risk for an individual according to a selection of important predictors [7]. This tool is recommended by the European guidelines [5] but only applies to individuals up to 65 years of age. The calculator within ACC/AHA guidelines has an upper age limit of 79 years [4] and Framingham data apply to those < 75 years [8]. At older ages, treatment decisions are complicated by the lack of conclusive evidence of a positive benefit-risk balance, regarding both secondary and primary prevention; the clinical trials do not include a sufficient number of older individuals. The ACC/AHA guidelines for individuals aged > 75 are based on expert opinions rather than evidence from clinical trials [4]. A recent review emphasizes the lack of evidence regarding efficacy and safety of statins in the oldest old, especially in those with multimorbidity and frailty [9].
In addition to the absence of conclusive evidence regarding beneficial effects, decisions on drug treatment in the oldest old (≥ 80 years of age) are particularly complex because of comorbidities and increased susceptibility to adverse reactions. Nevertheless, statins are used in this age group. A Danish study found that 38% of men and 32% of women aged 75–84 years used statins during 2010 [10], and a Finnish study reported that almost 40% of community-dwelling individuals ≥ 70 years used statins in 2008 [11]. To the best of our knowledge, however, statin use in the oldest old has not been compared to the use in the younger elderly. Therefore, we do not know to what extent the limited evidence base and other complexities attached to the oldest olds are associated with statin treatment practice. To shed light on this issue, we performed this study to investigate the use of statins in the elderly according to age and indication.
Methods
Study population
The study population consisted of individuals, ≥ 65 years of age in 2010, who lived in the Swedish region of Västra Götaland during the entire study period, July 1, 2005 to December 31, 2010. Region Västra Götaland has a total population of about 1.7 million residents and is the second largest region in Sweden. Individuals with re-used personal identity number, as well as individuals who were deceased or who moved into or out of the region during the study period, were excluded from the study.
Data sources
Data were collected from four registers, linked by the unique personal identity number (PIN) [12, 13].
-
The Total Population Register at Statistics Sweden provided information about who were residents in Region Västra Götaland, as well as dates of deaths and moving into/out of the region during the study period.
-
The administrative healthcare register in Region Västra Götaland (the VEGA register) contributed with information on all diagnoses from both hospital and primary care. The diagnoses in Sweden are registered according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10).
-
The Swedish Prescribed Drug Register at the Swedish National Board of Health and Welfare provided information on all dispensed prescription drugs, purchased in any pharmacy in Sweden [14].
-
The Social Service Register at the National Board of Health and Welfare presented information of whether an individual lived in a nursing home or not.
Definitions and procedures
An individual was classified as a statin user if he/she filled statin prescriptions (Codes C10AA or C10BA in the Anatomical Therapeutic Chemical classification system (ATC) [15]) covering at least 75% of the year 2010. As Swedish regulations stipulate that drugs for a maximum of 3-month use can be purchased at a time, our definition of a statin user required ≥ 3 filled statin prescriptions a year. Individuals who had ≥ 1 dispenses within the multi-dose drug-dispensing system and thus had drugs delivered every fortnight were classified as statin users if they had ≥ 20 statin dispenses over the year.
Information on living conditions was obtained from the Social Service Register. If an individual had a record in this register in 2007, 2008, 2009, or 2010, he/she was classified as living in a nursing home and if not, community dwelling.
In order to characterize individuals at the beginning of 2010, we estimated the number of drugs in the medication list, recorded as a continuous variable, on December 31, 2009, as a proxy for burden of disease [16]. For estimations of medication lists, we used the established method that is also employed by the National Board of Health and Welfare [17]. In short, for individuals receiving their drugs via ordinary prescriptions, a medication list was constructed according to the filled prescriptions during the 3-month period preceding this date. Drugs were included in the medication list if the purchase covered treatment at the date in question according to (i) the date of filling the prescription, (ii) the amount of drug dispensed, and (iii) the prescribed dosage. Multi-dose dispensed drugs were included in the medication list if filled within 14 days before December 31, 2009.
ICD-10 diagnoses in primary as well as hospital care during the time January 1, 2005 until December 31, 2010 were identified for every individual. Individuals were categorized into either of four groups based on his/her recorded diagnoses:
-
Secondary prevention: Individuals with ≥ 1 diagnosis considered an indication for secondary prevention according to the Swedish National Board of Health and Welfare [18]: ischemic heart disease (ICD-10 I20-I25), cerebrovascular disease (ICD-10 I63-I67, I69.3), TIA (ICD-10 G45), or cerebral vascular syndromes (ICD-10 G46).
-
Diabetes/primary prevention: Individuals with a diabetes diagnosis (ICD-10 E10-14) but no secondary prevention diagnosis. Individuals who purchased diabetes drugs (ATC A10) covering 75% of the year were also included in this group. Diabetes is considered a severe risk factor for CVD and patients with diabetes are recommended statin treatment for primary prevention in most cases, according to the Swedish National Board of Health and Welfare [18].
-
Other risk factor diagnoses: Individuals with ≥ 1 diagnosis that could be associated with, or is a known risk factor for, cardiovascular disease. We used a hierarchical list of diagnoses previously defined and including hypertension and hypertensive heart and renal disease (ICD-10 I10-I13, I15), non-rheumatic mitral and aortic valve disorders (ICD-10 I34, I35), heart arrhythmias (ICD-10 I45-I49), heart failure (ICD-10 I50), atherosclerosis (ICD-10 I70), aortic aneurysm (ICD-10 I71), peripheral arterial disease (ICD-10 I739), arterial embolism and thrombosis (ICD-10 I74), and vascular disorders of intestine (ICD-10 K55) [19]. Chronic kidney disease (ICD-10 N18), obesity (ICD-10 E66), and hyperlipidemia (ICD-10 E78) were also added.
-
None: None of the above-described diagnoses could be identified.
The first two categories, that is, secondary prevention and diabetes, were considered established indications.
Statistics
Statistical analyses were performed using STATA (Version 14) and SPSS (IBM SPSS Statistics for Windows, version 23.0, Armonk, NY). Individuals ≥ 80 years of age were compared to those 65–79 years using 95% confidence intervals (CIs) for proportions, calculated with the method of Wilson. We used logistic regression to obtain crude and adjusted odds ratios (ORs) with 95% CIs for (i) statin use in individuals with ≥ 1 established indication and (ii) having ≥ 1 established indication in statin users. The results were adjusted for sex, age (continuous), multi-dose drug dispensing, number of drugs (continuous), and living conditions (nursing home or community).
Sensitivity analyses
To test the robustness of the results, we performed sensitivity analyses. First, we investigated if another definition of statin use would change the results, that is, filling ≥ 1 statin prescription, or receiving ≥ 1 statin dispensing within the multi-dose dispensing system, during 2010. Second, since atherosclerosis and peripheral arterial disease are commonly considered an indication for statin treatment, these diagnoses (ICD-10 I70 and I739) were included as established indications.
Results
Characteristics of the cohort
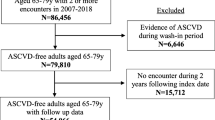
In all, 278,205 individuals were included in the analyses (Fig. 1). The median individual was 74 years old (range 65–110) and had 3 (0–38) drugs in the medication list. Summarized, 81,885 (29%) were 80 years or older; 153,142 (55%) were female; 29,385 (11%) had multi-dose drug dispensing; 13,882 (5%) were nursing home residents; and 100,235 (36%) were on ≥ 5 drugs.
A total of 86,320 (31%) individuals had ≥ 1 established indication for statin treatment; 61,173 (71%) individuals had cardiovascular disease; 42,527 (49%) had coronary heart disease; 20,802 (24%) had stroke/cerebrovascular disease; 7860 (9%) had TIA; and 38,746 (45%) had diabetes. For 25,147 (29%) individuals with diabetes, no other secondary prevention diagnosis was identified. Among the 191,885 individuals without an established indication, 83,172 (43%) had ≥ 1 risk factor diagnosis, most commonly high blood pressure (35%), dyslipidemia (9%), and atrial fibrillation (6%); 108,713 (57%) had none of the diagnoses registered.
Statin use
A total of 59,788 individuals (21%) were characterized as statins users, 37,764 (63%) of whom had ≥ 1 established indication. Statin treatment was less common in those aged ≥ 80 years compared to those 65–79 years (Table 1). In all individuals, irrespective of age, men were more likely to be on statins than women [24% (95% confidence interval (CI) 24%; 25%) vs. 19% (19%; 19%)], as were community-dwelling individuals compared to those living in nursing homes [22% (22%; 22%) vs. 10% (9%; 10%)], and individuals with ordinary prescriptions compared to multi-dose drug dispensing [22% (22%; 22%) vs. 18% (17%; 18%)].
In all statin users, as well as in subgroups by sex and number of drugs, ≥ 1 established indication was more common in those aged ≥ 80 years compared to those 65–79 years (Table 2). The proportion of individuals with ≥ 1 established indication did not differ between the age groups for patients with multi-dose drug dispensing and for those living in nursing homes.
In all, 37,764 (44% (43%; 44%)) out of 86,320 individuals with ≥ 1 established indication used statins; 27,825 (45% (45%; 46%) of those with ≥ 1 secondary prevention diagnosis, and 9939 (40% (39%; 40%)) of those with diabetes only. Among those with ≥ 1 established indication, statins were used to a lesser extent in those aged ≥ 80 years compared with those aged 65–79 years; (30% (30%; 31%) vs. 53% (52%; 53%)). Regression analyses showed that age ≥ 80 years, female sex, multi-dose drug dispensing, and living in a nursing home were associated with a lower probability of statin use (Table 3).
Without established indication
Among 22,024 statin users without an established indication, 16,806 (76%) had ≥ 1 risk factor diagnosis. Of the latter, 6590 (39%) had one risk factor diagnosis, 7342 (44%) had two, and 2874 (17%) had ≥ 3 such diagnoses. The most common diagnoses among these individuals were high blood pressure and related diagnoses (ICD-10 I10–I13, I15; n = 13,198, 60%) and hyperlipidemia (ICD-10 E78, n = 10,632, 48%) (Table 4). In all, 5218 (8.7% of all) statin users had neither an established indication nor a risk factor diagnosis.
Sensitivity analyses
When defining a statin user as having ≥ 1 filled statin prescription or ≥ 1 statin dispense within the multi-dose drug-dispensing system, the number of statin users increased from 59,788 to 104,043. The regression analyses revealed basically similar odds ratios as obtained in the main analysis. The same applied to the sensitivity analysis in which the diagnoses atherosclerosis (ICD-10 I70) and peripheral arterial disease (ICD-10 I739) were added as established indications (Appendix).
Discussion
In this population-based study, one in five older persons used statins regularly. Almost two out of three statin users had at least one established indication recorded during the preceding 5-year period. The use of statins varied by age; in people ≥ 80 years of age, statins were used more sparsely and more often with an established indication, compared with those 65–79 years of age. Further, nursing home residents and those with multi-dose drug dispensing used statins to a lesser extent.
The results suggest that physicians extrapolate scientific evidence for beneficial effects in younger age groups to the oldest olds but often require a more solid ground for treatment in the latter patients. In addition, assuming that multi-dose drug dispensing and living in a nursing home residence constitute surrogate markers of a great burden of disease, physicians seem to refrain from statin treatment in those seriously ill with lower life expectancy. Indeed, for these patients, the treated proportion among those with an established indication did not differ between the age groups. The results are consistent with studies where frail residents were less likely to be statin users [20]. In persons with at least one established indication, we found that about one third of those 80 years or older, and about half of those 65–79 years, used statins. These results are in line with other similar studies [10, 11].
Our results are reassuring as the efficacy of statins for secondary prevention of cardiovascular disease up to 75–80 years of age is considered as effective and safe as in the younger population [4]. A meta-analysis including studies on patients 65–82 years (mean age varied from 67 to 76 years) showed a relative risk reduction in all-cause mortality of 22% and coronary heart disease mortality of 26% in 5 years [21]. The same meta-analysis estimated the number of patients needed to treat over 5 years to save one life to 28 (95% CI 15;56). A subgroup analysis of the Heart Protection Study, mainly including individuals with high cardiovascular risk and established cardiovascular disease, also supports a significant effect on major cardiovascular events in the age group 75–80 years [22].
The difference in statin use between the age groups 65–79 and ≥ 80 years may be surprising; the risk of cardiovascular disease increases by age and therefore, theoretically, the oldest old could have a larger absolute benefit from treatment than their younger counterparts. However, the evidence for secondary prevention in the oldest old is, as earlier mentioned, sparse. The PROSPER study found a decrease in coronary heart disease mortality and non-fatal myocardial infarction (MI) in older people with a history of cardiovascular disease, when treated with pravastatin 40 mg compared to placebo, but still only included individuals up to 82 years [23]. A recent review [24] by Ruscica et al. concluded that statin treatment may be justified in persons 75 years or older for secondary prevention or at very high cardiovascular risk. Using the results of a large meta-analysis [25]; Ruscica et al. calculate that 167 individuals in this age group need to be treated for 1 year to prevent one vascular event, the corresponding figure for those 65–75 years being 111. According to the review, due to lack of evidence, statins are generally not justified in individuals ≥ 85 years of age [24].
Irrespective of evidence base, one may speculate regarding potential reasons for the substantial part of the elderly with an established indication but without statin treatment. First, the data available in this study did not include laboratory assessments. Individual lipid levels may sometimes have been considered when deciding against treatment, even though for secondary prevention, statin treatment is recommended regardless of lipid levels [4, 5, 18]. Second, other risk factors such as comorbidity/frailty, heredity, and smoking may add to treatment decisions, and this information is also lacking in our data. Thirdly, patient’s preferences may play an important role; adherence to statins has been shown to be limited [26]. Statins are also associated with drug-drug interactions and adverse reactions [27, 28]. Summarized, drawing conclusions on prescribing quality from our results may be a delicate task, as register data lack important information for individualized treatment decisions. Indeed, indicators of prescribing quality often have limited applicability at the individual patient level [29, 30]. Nevertheless, one cannot exclude that undertreatment may exist to some extent, as has previously been suggested [31].
We found that in one third of all statin users, no established indication could be identified during the preceding 5-year period. Some of these may have had an indication recorded before this period, and some may have indications not recorded in the register. However, it is also possible that several of these patients have statin treatment for primary prevention. This may be problematic; even though there is evidence from several RCTs on effects on all-cause mortality and cardiovascular mortality in individuals up to 75 years of age with high CVD risk but without prior CVD events [32], there is still insufficient evidence regarding benefits and harms of statin treatment for primary prevention in those ≥ 75 years of age [9, 24]. As this also applies to older people with frailty and multimorbidity, our findings that such individuals are treated with statins to a lower extent are reassuring. Summarized, it cannot be ruled out that some overtreatment exists, as has previously been suggested [31].
ACC/AHA and ESC/EAS guidelines recommend statin treatment for individuals with atherosclerosis and peripheral arterial disease, diagnoses which were not included among the established indications in the present study. However, the results did not change substantially when these diagnoses were added to the established diagnoses for statin treatment. The same was applied when all individuals filling a statin prescription were categorized as statin users. These sensitivity analyses support the robustness of the results.
Limitations
As previously mentioned, a major limitation of the present study, as in many other register studies, is that the data sources could not provide information on lipid levels, smoking status, heredity, blood pressure levels, education level, and socioeconomic status, factors that are important in decision making regarding drug treatment. However, in the analyses, we considered important variables reflecting burden of disease, including diagnoses in primary and hospital care, as well as residential status and use of multi-dose drug dispensing. That notwithstanding, it is a limitation that diagnoses may exist even if not recorded, and diagnoses may be registered earlier than the 5-year period covered. Moreover, data on statin doses are lacking.
Another limitation is that the data are some years old. However, the prevalence of statin use in older people has changed only slightly since 2010; according to national public register data, 34% of those aged ≥ 80 years filled a statin prescription in 2016 compared with 27% in 2010 [33]. For those 65–79 years, both in 2010 and 2016, 32% filled a statin prescription. Moreover, although atorvastatin is now often included among recommended statins, Swedish guidelines have not changed in any substantial way since 2010 regarding statin treatment.
Conclusion
In conclusion, this study shows that statins are used more sparsely and more often together with an established indication in the oldest old, compared with those 65–79 years of age. Our results suggest that physicians extrapolate scientific evidence for beneficial effects in younger age groups to the oldest ones but require a more solid ground for treatment. The findings that nursing home residents and those with multi-dose drug dispensing, irrespective of age, used statins to a lesser extent, suggests that physicians may refrain from treatment in those seriously ill with less life expectancy. In both age groups, our results also indicate some over- as well as undertreatment with statins.
References
Heart Protection Study Collaborative Group (2002) MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet (London, England) 360(9326):7–22. https://doi.org/10.1016/s0140-6736(02)09327-3
The long term intervention with pravastatin in ischaemic disease (lipi) study group (1998) Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 339(19):1349–1357. https://doi.org/10.1056/nejm199811053391902
Serruys PW, de Feyter P, Macaya C, Kokott N, Puel J, Vrolix M, Branzi A, Bertolami MC, Jackson G, Strauss B, Meier B (2002) Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. Jama 287(24):3215–3222
ACC/AHA (2013) 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. http://circ.ahajournals.org/content/circulationaha/early/2013/11/11/01.cir.0000437738.63853.7a.full.pdf. Accessed 17 Aug 2018
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, Bart van der Worp H, van Dis I, Verschuren WM (2016) 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & rehabilitation (EACPR). Atherosclerosis 252:207–274. https://doi.org/10.1016/j.atherosclerosis.2016.05.037
Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, Blumenthal R, Danesh J, Smith GD, DeMets D, Evans S, Law M, MacMahon S, Martin S, Neal B, Poulter N, Preiss D, Ridker P, Roberts I, Rodgers A, Sandercock P, Schulz K, Sever P, Simes J, Smeeth L, Wald N, Yusuf S, Peto R (2016) Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet (London, England) 388(10059):2532–2561. https://doi.org/10.1016/s0140-6736(16)31357-5
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24(11):987–1003
D'Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB (2008) General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 117(6):743–753. https://doi.org/10.1161/circulationaha.107.699579
Singh S, Zieman S, Go AS, Fortmann SP, Wenger NK, Fleg JL, Radziszewska B, Stone NJ, Zoungas S, Gurwitz JH (2018) Statins for primary prevention in older adults-moving toward evidence-based decision-making. J Am Geriatr Soc 66(11):2188–2196. https://doi.org/10.1111/jgs.15449
Wallach-Kildemoes H, Stovring H, Holme Hansen E, Howse K, Petursson H (2016) Statin prescribing according to gender, age and indication: what about the benefit-risk balance? J Eval Clin Pract 22(2):235–246. https://doi.org/10.1111/jep.12462
Upmeier E, Korhonen MJ, Helin-Salmivaara A, Huupponen R (2013) Statin use among older Finns stratified according to cardiovascular risk. Eur J Clin Pharmacol 69(2):261–267. https://doi.org/10.1007/s00228-012-1328-0
Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaelsson K, Neovius M, Stephansson O, Ye W (2016) Registers of the Swedish total population and their use in medical research. Eur J Epidemiol 31(2):125–136. https://doi.org/10.1007/s10654-016-0117-y
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24(11):659–667. https://doi.org/10.1007/s10654-009-9350-y
Wettermark B, Hammar N, Fored CM, Leimanis A, Otterblad Olausson P, Bergman U, Persson I, Sundstrom A, Westerholm B, Rosen M (2007) The new Swedish prescribed drug register—opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16(7):726–735. https://doi.org/10.1002/pds.1294
ACC/AHA (2013) Guidelines for ATC classification and DDD assignment 2013. WHO Collaborating Centre for Drug Statistic Methodology. http://www.whocc.no/filearchive/publications/1_2013guidelines.pdf. Accessed 17 Aug 2018
Brilleman SL, Salisbury C (2013) Comparing measures of multimorbidity to predict outcomes in primary care: a cross sectional study. Fam Pract 30(2):172–178. https://doi.org/10.1093/fampra/cms060
Johnell K, Fastbom J, Rosen M, Leimanis A (2007) Inappropriate drug use in the elderly: a nationwide register-based study. Ann Pharmacother 41(7):1243–1248. https://doi.org/10.1345/aph.1K154
Socialstyrelsen (2012) Nationella riktlinjer. http://www.socialstyrelsen.se/riktlinjer/nationellariktlinjer. Accessed 17 Aug 2018
Wallach Kildemoes H, Hendriksen C, Andersen M (2012) Drug utilization according to reason for prescribing: a pharmacoepidemiologic method based on an indication hierarchy. Pharmacoepidemiol Drug Saf 21(10):1027–1035. https://doi.org/10.1002/pds.2195
Campitelli MA, Maxwell CJ, Giannakeas V, Bell CM, Daneman N, Jeffs L, Morris AM, Austin PC, Hogan DB, Ko DT, Lapane KL, Maclagan LC, Seitz DP, Bronskill SE (2017) The variation of statin use among nursing home residents and physicians: a cross-sectional analysis. J Am Geriatr Soc 65(9):2044–2051. https://doi.org/10.1111/jgs.15013
Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJ, Eisenberg MJ (2008) Statins for secondary prevention in elderly patients: a hierarchical bayesian meta-analysis. J Am Coll Cardiol 51(1):37–45. https://doi.org/10.1016/j.jacc.2007.06.063
Farmer JA, Gotto AM Jr (2003) The Heart Protection Study: expanding the boundaries for high-risk coronary disease prevention. Am J Cardiol 92(1a):3i–9i
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG (2002) Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet (London, England) 360(9346):1623–1630
Ruscica M, Macchi C, Pavanello C, Corsini A, Sahebkar A, Sirtori CR (2018) Appropriateness of statin prescription in the elderly. Eur J Intern Med 50:33–40. https://doi.org/10.1016/j.ejim.2017.12.011
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet (London, England) 376(9753):1670–1681. https://doi.org/10.1016/s0140-6736(10)61350-5
Citarella A, Kieler H, Sundstrom A, Linder M, Wettermark B, Berglind IA, Andersen M (2014) Family history of cardiovascular disease and influence on statin therapy persistence. Eur J Clin Pharmacol 70(6):701–707. https://doi.org/10.1007/s00228-014-1659-0
Bellosta S, Corsini A (2012) Statin drug interactions and related adverse reactions. Expert Opin Drug Saf 11(6):933–946. https://doi.org/10.1517/14740338.2012.712959
Leporini C, Degli Esposti L, Sangiorgi D, Ursini F, Scicchitano F, Russo E (2015) Adverse drug reactions, medication adherence and physicians’ prescribing behavior: which relationship? A database analysis on statin use. Value Health 18(7):A374. https://doi.org/10.1016/j.jval.2015.09.770
Lonnbro J, Wallerstedt SM (2017) Clinical relevance of the STOPP/START criteria in hip fracture patients. Eur J Clin Pharmacol 73(4):499–505. https://doi.org/10.1007/s00228-016-2188-9
Wallerstedt SM, Belfrage B, Fastbom J (2015) Association between drug-specific indicators of prescribing quality and quality of drug treatment: a validation study. Pharmacoepidemiol Drug Saf 24(9):906–914. https://doi.org/10.1002/pds.3827
Finnikin S, Ryan R, Marshall T (2017) Statin initiations and QRISK2 scoring in UK general practice: a THIN database study. Br J Gen Pract 67:e881–e887. https://doi.org/10.3399/bjgp17X693485
Chou R, Dana T, Blazina I, Daeges M, Jeanne TL (2016) Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US preventive services task force. Jama 316(19):2008–2024. https://doi.org/10.1001/jama.2015.15629
Socialstyrelsen (2017) Statistikdatabas. http://www.socialstyrelsen.se/statistik/statistikdatabas/lakemedel. Accessed 17 Aug 2018
Funding
The study was supported by the Swedish Research Council for Health, Working Life and Welfare, the Swedish Research Council (521-2013-2639), and the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (ALFGBG428711). The funding sources did not influence design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
The study complies with the Declaration of Helsinki. Ethics approval was obtained from the Regional Ethical Review Board in Gothenburg (Dnr 782-11).
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Sensitivity analysis 1
Sensitivity analysis 2
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sundvall, H., Fastbom, J., Wallerstedt, S.M. et al. Use of statins in the elderly according to age and indication—a cross-sectional population-based register study. Eur J Clin Pharmacol 75, 959–967 (2019). https://doi.org/10.1007/s00228-019-02645-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02645-w