Abstract
Chlamydia psittaci is a zoonotic pathogen with a broad host range that can lead to severe respiratory and systemic disease in humans. Currently, an effective commercial vaccine against C. psittaci infection is not available. The chlamydial plasmid is an important virulence factor and encodes plasmid proteins that play important roles in chlamydial infection and the corresponding immune response. In this study, we assessed the efficacy of vaccination with plasmid proteins at preventing C. psittaci lung infection in a murine model. BALB/c mice were immunized intraperitoneally, three times at 2-week intervals, with purified recombinant CPSIT_p8 protein and then infected with C. psittaci. Immunization significantly decreased chlamydial load in the lungs of infected mice, resulted in a lower level of IFN-γ, and reduced the extent of inflammation. In vivo or in vitro neutralization of C. psittaci with sera collected from immunized mice did not reduce the amount of viable C. psittaci in the lungs of mice, indicating that CPSIT_p8-specific antibodies do not have neutralizing capacity. Furthermore, confocal fluorescence microscopy using a mouse anti-CPSIT_p8 antibody revealed that CPSIT_p8 was localized inside the inclusion of C. psittaci 6BC-infected cells. Our results demonstrate that CPSIT_p8 protein induces significant protective immunity against challenge with C. psittaci in mice and represents a promising new vaccine candidate for the prevention of C. psittaci infection.
Similar content being viewed by others
Introduction
Chlamydia psittaci is an obligate intracellular pathogen that causes ornithosis or psittacosis, a mainly avian respiratory disease with a significant financial impact on bird breeding and poultry farming. C. psittaci primarily infects birds but can spread from birds to humans. In humans, the resulting psittacosis is largely a respiratory disease, but C. psittaci can be transmitted diverse organs, and in a few poorly managed cases has resulted in death (Harkinezhad et al. 2009; Voigt et al. 2012). C. psittaci has a characteristic biphasic developmental cycle during growth, comprising a metabolically inactive, infectious form known as an elementary body (EB) and a noninfectious reticulate body (RB), which is metabolically active and divides intracellularly (Abdelrahman and Belland 2005). After completing development, the EBs are released and subsequently either disseminate or infect nearby host cells (Hybiske and Stephens 2007).
Although chlamydial infections can be treated effectively with widely available antimicrobial drugs, vaccination is considered a desirable strategy for reducing the spread of chlamydial diseases (Igietseme et al. 2011; Longbottom and Livingstone 2006; Xu et al. 2011). Previous studies have shown that vaccines based on chimeric hepatitis B surface antigen (HBsAg) C-terminally fused to the Chlamydia trachomatis major outer membrane protein (MOMP) multi-epitope can induce a specific protective immune response against chlamydial infection in a murine model (Zhu et al. 2014). To date, however, there is still no vaccine available to prevent chlamydial infection despite considerable efforts over a number of years.
C. psittaci possesses an important virulence factor in the form of a highly conserved, approximately 7.5 kb “cryptic” plasmid containing eight open reading frames (ORFs) (Pawlikowska-Warych et al. 2015), one of which encodes the protein CPSIT_p8 (Pgp4). Plasmidless clinical isolates are rare under natural conditions, indicating the importance of the plasmid in chlamydial pathogenesis (Comanducci et al. 1990). An improved understanding of the function of this plasmid in the biology and pathogenesis of chlamydial disease would be highly beneficial for vaccine development. The plasmid is thought to regulate glycogen synthase genes, including glgA, on the chlamydial chromosome; the accumulation of glycogen is essential for divisions inside the chlamydial inclusion (Carlson et al. 2008; Wang et al. 2011). Indeed, the chlamydial plasmid functions as a transcriptional regulator of multiple chromosomal genes, which are likely important virulence factors for chlamydial pathogenicity (Carlson et al. 2008; Frazer et al. 2012; O’Connell et al. 2011). The functions of the plasmid-encoded and regulated proteins in chlamydial pathogenesis and protective immunity remain largely unclear. However, the plasmid-mediated virulence is known to boost proinflammatory cytokine stimulation by the triggering of Toll-like receptors (TLRs) in murine models (O’Connell et al. 2011). It has been shown that the pgp4 gene affects the capacity to accumulate glycogen in chlamydial inclusions and that the encoded Pgp4 protein is a transcriptional regulator of chlamydial plasmid and chromosomal genes, which are likely responsible for virulence (Song et al. 2013, 2014). Immunization with recombinant Pgp3 or Pgp4 protein results in a significantly lower Chlamydia muridarum load in the lungs of infected mice and a lower level of IFN-γ consistent with a reduction in inflammation (Mosolygo et al. 2014). It has been reported that Pgp3 is a plasmid-encoded virulence factors for the induction of hydrosalpinx by C. muridarum and is a target for the attenuation of chlamydial pathogenicity (Liu et al. 2014). Thus, the roles of some C. trachomatis and C. muridarum plasmid-encoded proteins are well-defined. When the C. psittaci CPSIT_p8 sequence, which likely encodes Pgp4, was analyzed using the SmartBLAST database from NCBI, we found 75 % sequence identity between C. psittaci and C. trachomatis Pgp4 and 76 % sequence identity between C. psittaci and C. muridarum Pgp4. Therefore, we predict that CPSIT_p8 may have similar functions to those of Pgp4 from other species, as mentioned above.
In this study, we set out to assess the localization of CPSIT_p8 protein and the protective capacity of vaccination with recombinant protein CPSIT_p8 against C. psittaci lung infection in a mouse model. The results reveal that CPSIT_p8 is localized within the inclusion of C. psittaci 6BC-infected cells and that multiple immunization with CPSIT_p8 reduces the chlamydial load and inflammation in the lungs of mice after intranasal C. psittaci infection. Thus, CPSIT_p8 protein is a potential vaccine candidate against C. psittaci infection.
Materials and methods
Cell culture and propagation of C. psittaci
HeLa 229 cells (ATCC, CCL-2.1) were grown at 37 °C with 5 % CO2 in complete Dulbecco’s modified Eagle medium (DMEM; HyClone, USA) with 10 % fetal bovine serum (FBS; Invitrogen, Grand Island, NY, USA). C. psittaci 6BC (ATCC VR-125) EBs were propagated in HeLa 229 cell monolayers, purified by density gradient centrifugation and stored at −80 °C (Caldwell et al. 1981). Infectious EB titers were determined by indirect immunofluorescence. Serial dilutions of the chlamydial EBs were inoculated onto HeLa 229 cell monolayers and, after 45 h culture, the cells were fixed and stained with a FITC-labeled monoclonal antibody against chlamydial LPS (Meridian Diagnostics, Inc., Cincinnati, OH). The titer of infectious EBs was expressed in inclusion-forming units (IFUs).
Cloning, expression, and purification of recombinant CPSIT_p8
The full-length CPSIT_p8 gene (GenBank accession no. NC_015217) was amplified by polymerase chain reaction (PCR) from a preparation of C. psittaci 6BC genomic DNA and cloned into the expression vector pET30a via BamHI (5′-end) and NotI (3′-end) restriction sites to express N-terminally His-tagged protein. The forward primer for CPSIT_p8 was 5′-CGCGGATCCATGAATGATAAACAGAATATGAC-3′ and the reverse primer was 5′-TTTTCCTTTTGCGGCCGCTTATTCAGCTTTTGAGAACATA-3′, which included restriction sites (underlined) for BamHI and NotI, respectively. The sequence of the CPSIT_p8 construct within the pET30a vector was confirmed by DNA sequencing. E. coli BL21 strains harboring the expression vectors were grown in Luria-Bertani medium containing kanamycin (50 μg/ml). Protein expression was induced by isopropyl-β-D-thiogalactoside (IPTG) at a final concentration of 0.2 mM for 8 h at 30 °C. Bacteria were collected and lysed in a buffer containing 300 mM NaCl, 50 mM Tris-HCl (pH 9.9), 10 mM imidazole, 1 % Triton X-100, and 20 % glycerol. The His-tagged proteins were purified using Ni-nitrilotriacetic acid (NTA) beads (QIAGEN Inc., Germany) according to the manufacturer’s instructions. Proteins were subsequently washed with 20 and 50 mM imidazole and eluted with 150 mM imidazole in 300 mM NaCl, 50 mM Tris-HCl (pH 9.9), and 10 % glycerol. Subsequently, the fusion proteins were concentrated with an Amicon Ultra-15 unit (Millipore, Billerica, MA) and endotoxins were removed with a polymyxin B cartridge (Sigma, St. Louis, MO, USA). The protein concentrations were assessed by using a bicinchoninic acid protein assay kit (Pierce, Rockford, IL, USA).
Animals and immunization
Pathogen-free female BALB/c mice (6–8 weeks old) were purchased from Hunan SJA Laboratory Animal Co. Ltd. A total of three groups of mice with 16 animals in each group were injected intraperitoneally (i.p.) with either purified recombinant CPSIT_p8 (experimental group) or Freund’s adjuvant (FA; negative control group) or phosphate buffered saline (PBS; blank control group), respectively. Experimental group mice were immunized three times at 2-week intervals with 30 μg of purified recombinant CPSIT_p8 protein emulsified in FA (complete adjuvant for the first injection and incomplete adjuvant subsequently; Sigma) in a volume of 0.1 ml (Tu et al. 2014). Fourteen days after the final immunization, serum samples were harvested by retro-orbital bleeding for the antibody production, in vitro neutralization of C. psittaci and in vivo neutralization experiments.
Immunoblotting analysis
Purified recombinant CPSIT_p8 protein was diluted 1:4 in 5× sample loading buffer with 5 % β-mercaptoethanol and boiled for 10 min at 100 °C, subsequently separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) on 12 % (wt/vol) gels, and blotted onto a polyvinylidene fluoride (PVDF) membrane (0.22 μm; Millipore) using a semidry Trans-Blot SD apparatus (Bio-Rad). The membranes were blocked at room temperature (RT) for 3 h with Tris-buffered saline (TBS) containing 5 % skim milk and 0.05 % Tween 20 (Sigma) (Zhao et al. 2013). The membranes were then incubated overnight at 4 °C with a pool of sera collected from CPSIT_p8-immunized or control mice, or an anti-His-tag mouse monoclonal antibody (1:500 dilution in TBS containing 5 % skim milk and 0.05 % Tween 20). After washing four times with TBS containing 0.05 % Tween 20 (TBST), the membranes were incubated for 1 h at 37 °C with horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Abcm, UK). Finally, to detect protein bands, ECL Prime Western Blotting Detection Reagent (Auragene) was used as recommended and visualized with a G:BOX Chemi XX9 (Syngene, UK) digital imager.
Immunofluorescence and confocal microscopy
HeLa 229 cells grown on coverslips were infected with C. psittaci 6BC at the MOIs indicated and incubated for 36 h. Infected cells were washed with PBS and fixed with 4 % paraformaldehyde for 30 min. The adherent cells were washed three times with PBS and then permeabilized in 0.3 % Triton-100/PBS for 10 min. The cells were then blocked with complete DMEM containing 10 % FBS overnight at 4 °C. After washing, the cells were incubated with rabbit anti-C. psittaci 6BC antibody and mouse anti-CPSIT_p8 antibody for 2 h at RT and then washed four times with PBS. Cy2-labeled (green fluorescence) goat anti-rabbit immunoglobulin G (IgG) (Jackson ImmunoResearch Laboratories, USA) and Cy3-labeled (red fluorescence) goat anti-mouse IgG (Jackson ImmunoResearch Laboratories, USA) were added to the cells and incubated for 1 h at RT. All samples were additionally stained with 4, 6-diamidine-2-phenylindole dihydrochloride (DAPI; Sigma) for nuclear DNA. All antibodies were diluted with complete DMEM containing 10 % FBS. After washing, the coverslips bearing the adherent cells were mounted on glass microscope slides. Images of infected and immunostained HeLa 229 cells were obtained with a Leica LCS SP8 STED confocal laser scanning microscopy using LAS X software (Leica, Germany).
Challenge of mice and culture of C. psittaci from lung tissue
Fourteen days after the final immunization, mice were challenged intranasally (i.n.) with 5 × 105 IFUs of C. psittaci in 30 μl of sucrose-phosphate-glutamicacid (SPG) buffer under ether anesthesia (Bode et al. 2012; Dutow et al. 2014; Tammiruusu et al. 2007). The immunized and control mice were weighed before, and 4, 7, and 10 days after, the i.n. challenge with C. psittaci. Mice were euthanized 10 days after infection, and the lungs were harvested, weighed, and homogenized in SPG (1.2 ml/100 mg) buffer to test C. psittaci titers and cytokine levels. Lung homogenates from individuals from each group of mice were centrifuged (4 °C, 15 min, 6000 rpm) and serial dilutions of the lung supernatants were inoculated onto HeLa 229 cell monolayers. Intracellular inclusions were detected by fluorescence microscopy. Lungs of three mice from each group were embedded in paraffin for histopathological assessment and were sectioned and stained with hematoxylin-eosin (H&E) and an UltraSensitive™SP (Rabbit) IHC Kit (Maixin, China).
Measurements of cytokine levels from the lungs
The supernatants of lung homogenates harvested from immunized and subsequently C. psittaci-infected mice were centrifuged as described above, and cytokine levels were detected with Ready-SET-Go! kits (eBioscience Inc., CA, USA) except IL-17 (R&D Systems, Inc., Minneapolis, MN, USA). The sensitivities of the IL-4, IL-6, IL-10, IL-12, IL-17, and IFN-γ tests were in the ranges 4–500, 4–500, 32–4000, 31.3–2000, 0–700, and 15–2000 pg/ml, respectively. The clarified supernatants were assayed in duplicate according to the manufacturer’s guidelines.
In vivo neutralization of the mice
Groups of five naive BALB/c mice were challenged i.n. with 5 × 105 IFUs of C. psittaci in 30 μl of SPG 24 h before the mice were injected i.p. with 200 μl of pooled serum obtained from mice immunized with CPSIT_p8, Freund’s adjuvant or PBS. The mice were euthanized on day 10 after C. psittaci infection and treated as described above.
In vitro neutralization of C. psittaci
Sera obtained from mice immunized with CPSIT_p8, Freund’s adjuvant or PBS were mixed with 5 × 105 C. psittaci IFUs and incubated for 1 h at RT. Groups of five naive BALB/c mice were challenged i.n. with the serum-treated C. psittaci. The mice were euthanized on day 10 after C. psittaci infection and treated as described above.
Statistical analysis
Using SPSS 18.0 software, statistical comparisons between groups for chlamydial load and cytokine levels after infection were made by one-way analysis of variance (ANOVA) with the Student-Newman-Keuls test. The criterion for statistical significance was set at P < 0.05.
Results
Expression, purification, and identification of recombinant protein CPSIT_p8
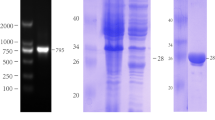
The CPSIT_p8 gene was successfully amplified by PCR from C. psittaci 6BC genomic DNA (Fig. 1a) and subsequently cloned into the expression vector pET30a. The construct was transformed into E. coli BL21 and expressed as a His-tagged protein with a predicted size of 17 kDa, which was assessed by SDS-12 % PAGE analysis to have a purity of >95 %. The CPSIT_p8 fusion protein was purified from cell-free supernatants using Ni-NTA beads (Fig. 1b) and identified by immunoblotting with an anti-His tag monoclonal antibody (Fig. 1c).
Expression, purification, and identification of His-tagged CPSIT_p8 protein. Amplification of the CPSIT_p8 (309 bp) gene from a preparation of C. psittaci 6BC genomic DNA (a). SDS-PAGE analysis of the expression of CPSIT_p8 in E. coli BL21 harboring the pET30a-CPSIT_p8 plasmid with (+) or without (−) IPTG, together with purified His-tagged CPSIT_p8 (b). Western blot analysis of His-tagged CPSIT_p8 protein with anti-His monoclonal antibody (c), CPSIT_p8-immunized mice sera (d), and FA- or PBS-immunized mice sera (e)
Subcellular localization of CPSIT_p8 in C. psittaci 6BC-infected cells
The intracellular localization of CPSIT_p8 in C. psittaci-infected HeLa 229 cells was determined by indirect immunofluorescence using a mouse polyclonal anti-CPSIT_p8 antibody. CPSIT_p8 was identified inside the inclusion of C. psittaci-infected cells (Fig. 2).
Subcellular localization of CPSIT_p8 in C. psittaci 6BC-infected cells (1000×). a HeLa 229 cells were infected with C. psittaci 6BC and were then cultivated for 36 h before harvesting. The cells were fixed; immunolabeled with anti-CPSIT_p8 (red), anti-C. psittaci 6BC (green) antibodies, and DAPI (blue, nuclei); and viewed under a confocal laser scanning microscopy. All signals were merged. b Cells were analyzed in a sequential series of Z-stack images at 0.22-μm intervals by confocal laser scanning microscopy
CPSIT_p8 can elicit protective immunity against C. psittaci infection
To investigate whether an immune response to CPSIT_p8 can protect against C. psittaci infection, BALB/c mice were immunized i.p. three times at 2-week intervals with recombinant CPSIT_p8 mixed with Freund’s adjuvant. The humoral immune response to CPSIT_p8 protein was assessed by immunoblotting with sera collected from immunized mice 14 days after the final immunization. Sera obtained from Freund’s adjuvant- and PBS-immunized mice (without CPSIT_p8) were used as controls. As anticipated, the immunization schedule involving injection with CPSIT_p8 induced production of CPSIT_p8-specific antibodies (Fig. 1d), while the sera of both control groups of mice did not react with the recombinant CPSIT_p8 protein (Fig. 1e). Two weeks after the final immunization, the mice were challenged i.n. with C. psittaci to determine whether the CPSIT_p8-specific immune response protected mice against C. psittaci infection. Mice were weighed on days 4, 7, and 10 after the infection, but there was no significant difference between experimental (CPSIT_p8-immunized) and control (data not shown) groups. The protective effect of CPSIT_p8 was demonstrated by examining the C. psittaci load in the lungs of mice (Fig. 3). Immunization of mice with recombinant protein CPSIT_p8 elicited a significantly lower chlamydial burden, compared to controls.
C. psittaci titers in the lungs of CPSIT_p8 immunized mice after C. psittaci infection. Mice immunized with FA and PBS were used as controls. Mice were infected with 5 × 105 IFUs of C. psittaci 2 weeks after the final immunization with CPSIT_p8 and then euthanized 10 days later. Lung homogenates were inoculated onto HeLa 229 cell monolayers, and the chlamydial inclusions were counted by indirect immunofluorescence. Means ± SD of C. psittaci titers (IFU/lung) in the lung homogenates from 10 individual mice in three independent experiments are shown. **P < 0.05
Inflammatory infiltrates were notably reduced in H&E-stained lung sections of C. psittaci-infected mice immunized with CPSIT_p8 protein (Fig. 4a) compared to Freund’s adjuvant- (Fig. 4b) and PBS- (Fig. 4c) immunized mice. The integrity of alveolar structure is maintained in the lungs of CPSIT_p8 immunized mice, compared to controls, which suffered deterioration. Assessment of lung tissue sections by streptavidin-peroxidase (S-P) immunohistochemistry revealed that C. psittaci-infected mice immunized with CPSIT_p8 protein (Fig. 5a) have fewer pathological features, such as edema, hyperemia, and inflammatory cell infiltration, compared to Freund’s adjuvant- (Fig. 5b) and PBS- (Fig. 5c) immunized mice. Besides, immunization of mice with recombinant CPSIT_p8 protein caused a notably lower chlamydial load (brown granule), compared to controls.
C. psittaci load and pathological changes in lung tissue assessed by S-P immunohistochemistry. Lungs of CPSIT_p8- (a), FA- (b), and PBS- (c) immunized mice were sectioned and stained with S-P immunohistochemistry 10 days after infection with C. psittaci. The UltraSensitive™SP (Rabbit) IHC Kit, with a rabbit anti-C. psittaci 6BC as the first antibody, was used to detect C. psittaci inclusion. Mice immunized with FA and PBS were used as controls. Those with brown granules (red arrow) in the nuclei of lung tissue cells contain a C. psittaci inclusion
A potential vaccine candidate must satisfy two criteria: it must stimulate a protective immune response and must eliminate the unregulated inflammation that leads to pathological changes during infection. We investigated the second criterion, i.e., that of increased inflammation, in the lungs of CPSIT_p8-immunized and control mice following C. psittaci intranasal infection by measuring the concentrations of IL-4, IL-6, IL-10, IL-12, IL-17, and IFN-γ with an enzyme-linked immunosorbent assay (ELISA) (Fig. 6). There were no significant differences in the levels of IL-4, IL-6, IL-10, IL-12, or IL-17 between the CPSIT_p8-immunized and the control mice. Nevertheless, the level of IFN-γ in the lungs of protein-immunized mice was significantly lower, compared to controls.
Production of cytokines in the lungs of CPSIT_p8-, FA-, and PBS-immunized mice. Lung homogenates were detected using an IL-4, IL-6, IL-10, IL-12, IL-17, and IFN-γ ELISA kit according to the manufacturer’s protocols. Means ± SD of the results from 10 individual mice lungs in three independent experiments. ***P < 0.001
Effect of passive immunization with CPSIT_p8-specific antibodies on the outcome of C. psittaci intranasal infection
Because immunization with CPSIT_p8-induced specific antibody responses, we next evaluated the ability of these antibodies to provide passive immunity against intranasal infection with C. psittaci. For the in vivo neutralization of C. psittaci, sera of CPSIT_p8-immunized or control mice were collected 2 weeks after the final immunization and injected i.p. into naive mice 24 h after C. psittaci infection. The mice were euthanized 10 days later, and the recoverable chlamydial load in the lungs was determined. The titer of viable C. psittaci was not notably lower in the lungs of mice treated with serum of CPSIT_p8-immunized compared to control mice (Fig. 7). To evaluate the infectivity of in vitro serum-treated C. psittaci, naive mice were infected with C. psittaci EBs incubated at RT with sera of CPSIT_p8-immunized or control mice. However, the antibodies in the sera of CPSIT_p8-immunized mice did not offer protection against C. psittaci infection: the chlamydial load in the lungs of infected mice was not reduced (Fig. 7).
In vivo and in vitro neutralization of C. psittaci with the sera of CPSIT_p8-immunized or control mice. Naive mice were injected with the sera of immunized or control mice after C. psittaci i.n. infection or were infected with C. psittaci treated in vitro with sera collected from immunized or control mice. The C. psittaci titer in the lungs was determined by indirect immunofluorescence 10 days after infection. Means ± SD of C. psittaci titers (IFU/lung) in the lung homogenates from five individual mice in three independent experiments are shown
Discussion
C. psittaci 6BC contains a single circular chromosome of 1.172 Mb and a highly conserved plasmid of 7553 bp, the latter of which plays an important role in chlamydial pathogenesis (Pawlikowska-Warych et al. 2015; Voigt et al. 2012). Four plasmids of avian strains of C. psittaci have been well characterized and are predicted to include eight ORFs (Lusher et al. 1989; Thomas et al. 1997). Currently, the immunological and functional roles of Pgp3 or Pgp4 are well-defined in some chlamydial species as described above, but C. psittaci plasmid-encoded Pgp4 is less well understood.
In this study, CPSIT_p8 (Pgp4) is one of the proteins encoded by the C. psittaci plasmid. We successfully cloned the CPSIT_p8 gene, expressed recombinant CPSIT_p8 protein in E. coli BL21, and purified the protein using His-tag affinity chromatography. The size of the recombinant CPSIT_p8 was slightly larger than predicted, possibly due to the His-tag at the N-terminus. The CPSIT_p8 reacted with an anti-His-tag monoclonal antibody and with sera collected from CPSIT_p8-immunized mice in immunoblotting experiments. This showed that recombinant CPSIT_p8 can induce the production of specific antibodies in mice.
We set out to reveal whether immunization with CPSIT_p8 protein was able to stimulate a sufficiently strong and specific immune response to offer mice protection against C. psittaci infection. Overall, our results provide clear evidence that immunization with CPSIT_p8 can reduce chlamydial load in infected mice. It has been shown previously that DNA immunization with the C. trachomatis pgp3 gene can inhibit the spread of the infection in C3H/HeN mice (Donati et al. 2003). A pORF5 DNA vaccine was also assessed in a murine model in which vaccinated mice showed notably reduced bacterial shedding upon chlamydial infection and an accelerated resolution of the genital infection. Moreover, the immunized mice displayed protective immunity against the pathological consequences of chlamydial infection (Li et al. 2008b). Another study showed that immunization of C57BL/6N mice with recombinant Pgp3 or Pgp4 resulted in a significantly lower chlamydial load and reduced pathological changes in lung tissue after C. muridarum infection (Mosolygo et al. 2014). The degree of prevention was similar to that in our study, in which the amount of recoverable chlamydia was reduced 10 days after infection. IFN-γ is a necessary component of the response to chlamydial infection and is required for full resolution of genital infection. The function of IFN-γ in the chlamydia-infected cells in vitro involves indoleamine dioxygenase, which may be correlated with chlamydial clearance (Rottenberg et al. 2000). In our study, amplification of the inflammation was reduced in the lungs of C. psittaci-infected mice immunized with CPSIT_p8 proteins, as demonstrated by a reduced level of IFN-γ. Pgp3, a potential Toll-like receptors agonist, is a unique plasmid protein secreted into the host-cell cytosol during chlamydial infection (Li et al. 2008a). Plasmid-encoded Pgp3 is an essential virulence factor of C. muridarum pathogenicity in mice (Liu et al. 2014), While Pgp4 is a non-structural, non-secreted protein and is a transcriptional regulator of chlamydial virulence-associated gene expression (Song et al. 2013). In this study, we showed that CPSIT_p8 is localized inside the inclusion of C. psittaci-infected cells; thus, CPSIT_p8 is a non-secreted protein and may be an important regulator of chlamydial gene expression. The protective effect of CPSIT_p8 is a new finding and is reminiscent of the role of Pgp3 described above.
To identify which element of the immune system is responsible for the protective efficacy of the CPSIT_p8-specific immunity, we performed neutralization experiments under in vitro and in vivo conditions. It has been shown previously that neither Pgp3 nor Pgp4 were able to elicit the production of neutralizing antibodies in mice (Mosolygo et al. 2014). Similarly, we found that CPSIT_p8 also did not give rise to neutralizing antibodies, as the amount of recoverable C. psittaci in in vitro and in vivo neutralization experiments was similar in both experimental and control mice. It is therefore more likely that antibodies against CPSIT_p8 play a role in the cellular immune response, perhaps by boosting antigen uptake and presentation (Moore et al. 2003). We have, in fact, assessed the CPSIT_p8-specific cellular immune response (data not shown): our preliminary results show that splenocytes from CPSIT_p8-immunized mice exhibit both increased IFN-γ production and minimal IL-4 production in vitro, indicating a strong Th1 immune response.
In summary, CPSIT_p8 protein is localized inside the inclusion of C. psittaci 6BC-infected cells. Multiple immunization with recombinant CPSIT_p8 protein led to a significantly reduced chlamydial load in the lungs of mice infected with C. psittaci, but CPSIT_p8-specific antibodies had no neutralizing ability. We also note with interest that immunization with the regulatory plasmid protein CPSIT_p8 can cause protection similar to that with Pgp3. These results provide novel and important information for understanding chlamydial pathogenic mechanisms and development of chlamydial subunit vaccines.
References
Abdelrahman YM, Belland RJ (2005) The chlamydial developmental cycle. FEMS Microbiol Rev 29(5):949–959
Bode J, Dutow P, Sommer K, Janik K, Glage S, Tummler B, Munder A, Laudeley R, Sachse KW, Klos A (2012) A new role of the complement system: C3 provides protection in a mouse model of lung infection with intracellular Chlamydia psittaci. PLoS One 7(11):e50327
Caldwell HD, Kromhout J, Schachter J (1981) Purification and partial characterization of the major outer membrane protein of Chlamydia trachomatis. Infect Immun 31(3):1161–1176
Carlson JH, Whitmire WM, Crane DD, Wicke L, Virtaneva K, Sturdevant DE, Kupko JJ 3rd, Porcella SF, Martinez-Orengo N, Heinzen RA, Kari L, Caldwell HD (2008) The Chlamydia trachomatis plasmid is a transcriptional regulator of chromosomal genes and a virulence factor. Infect Immun 76(6):2273–2283
Comanducci M, Ricci S, Cevenini R, Ratti G (1990) Diversity of the Chlamydia trachomatis common plasmid in biovars with different pathogenicity. Plasmid 23(2):149–154
Donati M, Sambri V, Comanducci M, Di Leo K, Storni E, Giacani L, Ratti G, Cevenini R (2003) DNA immunization with pgp3 gene of Chlamydia trachomatis inhibits the spread of chlamydial infection from the lower to the upper genital tract in C3H/HeN mice. Vaccine 21(11–12):1089–1093
Dutow P, Fehlhaber B, Bode J, Laudeley R, Rheinheimer C, Glage S, Wetsel RA, Pabst O, Klos A (2014) The complement C3a receptor is critical in defense against Chlamydia psittaci in mouse lung infection and required for antibody and optimal T cell response. J Infect Dis 209(8):1269–1278
Frazer LC, Darville T, Chandra-Kuntal K, Andrews CW Jr, Zurenski M, Mintus M, AbdelRahman YM, Belland RJ, Ingalls RR, O’Connell CM (2012) Plasmid-cured Chlamydia caviae activates TLR2-dependent signaling and retains virulence in the guinea pig model of genital tract infection. PLoS One 7(1):e30747
Harkinezhad T, Verminnen K, De Buyzere M, Rietzschel E, Bekaert S, Vanrompay D (2009) Prevalence of Chlamydophila psittaci infections in a human population in contact with domestic and companion birds. J Med Microbiol 58(Pt 9):1207–1212
Hybiske K, Stephens RS (2007) Mechanisms of host cell exit by the intracellular bacterium Chlamydia. Proc Natl Acad Sci U S A 104(27):11430–11435
Igietseme JU, Eko FO, Black CM (2011) Chlamydia vaccines: recent developments and the role of adjuvants in future formulations. Expert Rev Vaccines 10(11):1585–1596
Li Z, Chen D, Zhong Y, Wang S, Zhong G (2008a) The chlamydial plasmid-encoded protein pgp3 is secreted into the cytosol of Chlamydia-infected cells. Infect Immun 76(8):3415–3428
Li Z, Wang S, Wu Y, Zhong G, Chen D (2008b) Immunization with chlamydial plasmid protein pORF5 DNA vaccine induces protective immunity against genital chlamydial infection in mice. Sci China C Life Sci 51(11):973–980
Liu Y, Huang Y, Yang Z, Sun Y, Gong S, Hou S, Chen C, Li Z, Liu Q, Wu Y, Baseman J, Zhong G (2014) Plasmid-encoded Pgp3 is a major virulence factor for Chlamydia muridarum to induce hydrosalpinx in mice. Infect Immun 82(12):5327–5335
Longbottom D, Livingstone M (2006) Vaccination against chlamydial infections of man and animals. Vet J 171(2):263–275
Lusher M, Storey CC, Richmond SJ (1989) Plasmid diversity within the genus Chlamydia. J Gen Microbiol 135(5):1145–1151
Moore T, Ekworomadu CO, Eko FO, MacMillan L, Ramey K, Ananaba GA, Patrickson JW, Nagappan PR, Lyn D, Black CM, Igietseme JU (2003) Fc receptor-mediated antibody regulation of T cell immunity against intracellular pathogens. J Infect Dis 188(4):617–624
Mosolygo T, Szabo AM, Balogh EP, Faludi I, Virok DP, Endresz V, Samu A, Krenacs T, Burian K (2014) Protection promoted by pGP3 or pGP4 against Chlamydia muridarum is mediated by CD4(+) cells in C57BL/6N mice. Vaccine 32(40):5228–5233
O’Connell CM, AbdelRahman YM, Green E, Darville HK, Saira K, Smith B, Darville T, Scurlock AM, Meyer CR, Belland RJ (2011) Toll-like receptor 2 activation by Chlamydia trachomatis is plasmid dependent, and plasmid-responsive chromosomal loci are coordinately regulated in response to glucose limitation by C. trachomatis but not by C. muridarum. Infect Immun 79(3):1044–1056
Pawlikowska-Warych M, Sliwa-Dominiak J, Deptula W (2015) Chlamydial plasmids and bacteriophages. Acta Biochim Pol 62(1):1–6
Rottenberg ME, Gigliotti Rothfuchs A, Gigliotti D, Ceausu M, Une C, Levitsky V, Wigzell H (2000) Regulation and role of IFN-gamma in the innate resistance to infection with Chlamydia pneumoniae. J Immunol 164(9):4812–4818
Song L, Carlson JH, Whitmire WM, Kari L, Virtaneva K, Sturdevant DE, Watkins H, Zhou B, Sturdevant GL, Porcella SF, McClarty G, Caldwell HD (2013) Chlamydia trachomatis plasmid-encoded Pgp4 is a transcriptional regulator of virulence-associated genes. Infect Immun 81(3):636–644
Song L, Carlson JH, Zhou B, Virtaneva K, Whitmire WM, Sturdevant GL, Porcella SF, McClarty G, Caldwell HD (2014) Plasmid-mediated transformation tropism of chlamydial biovars. Pathog Dis 70(2):189–193
Tammiruusu A, Penttila T, Lahesmaa R, Sarvas M, Puolakkainen M, Vuola JM (2007) Intranasal administration of chlamydial outer protein N (CopN) induces protection against pulmonary Chlamydia pneumoniae infection in a mouse model. Vaccine 25(2):283–290
Thomas NS, Lusher M, Storey CC, Clarke IN (1997) Plasmid diversity in Chlamydia. Microbiology 143(Pt 6):1847–1854
Tu J, Hou B, Wang B, Lin X, Gong W, Dong H, Zhu S, Chen S, Xue X, Zhao KN, Zhang L (2014) A multi-epitope vaccine based on Chlamydia trachomatis major outer membrane protein induces specific immunity in mice. Acta Biochim Biophys Sin (Shanghai) 46(5):401–408
Voigt A, Schofl G, Saluz HP (2012) The Chlamydia psittaci genome: a comparative analysis of intracellular pathogens. PLoS one 7(4):e35097
Wang Y, Kahane S, Cutcliffe LT, Skilton RJ, Lambden PR, Clarke IN (2011) Development of a transformation system for Chlamydia trachomatis: restoration of glycogen biosynthesis by acquisition of a plasmid shuttle vector. PLoS Pathog 7(9):e1002258
Xu W, Liu J, Gong W, Chen J, Zhu S, Zhang L (2011) Protective immunity against Chlamydia trachomatis genital infection induced by a vaccine based on the major outer membrane multi-epitope human papillomavirus major capsid protein L1. Vaccine 29(15):2672–2678
Zhao H, Li HY, Han JF, Deng YQ, Li YX, Zhu SY, He YL, Qin ED, Chen R, Qin CF (2013) Virus-like particles produced in Saccharomyces cerevisiae elicit protective immunity against Coxsackievirus A16 in mice. Appl Microbiol Biotechnol 97(24):10445–10452
Zhu S, Feng Y, Rao P, Xue X, Chen S, Li W, Zhu G, Zhang L (2014) Hepatitis B virus surface antigen as delivery vector can enhance Chlamydia trachomatis MOMP multi-epitope immune response in mice. Appl Microbiol Biotechnol 98(9):4107–4117
Acknowledgments
This project was supported by the Natural Science Foundation of China (Grant No. 31270218, Grant No. 81171588) and the Special Foundation of Hunan Provincial Science and Technology Department (2013TT1003), the construct program of Hunan Provincial Key Laboratory for Special Pathogens Prevention and Control Foundation (Grant No. 2014-5), and Hunan Province Cooperative Innovation Center for Molecular Target New Drug Study (Grant No. 2015-351).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All animal procedures and treatments were approved by the Animal Welfare and Ethics Committee of the University of South China and were performed in accordance with the regulations of the institution.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Liang, M., Wen, Y., Ran, O. et al. Protective immunity induced by recombinant protein CPSIT_p8 of Chlamydia psittaci . Appl Microbiol Biotechnol 100, 6385–6393 (2016). https://doi.org/10.1007/s00253-016-7494-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-016-7494-8