Abstract
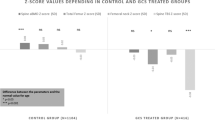
We carried out a comparative study in 78 post-menopausal women with rheumatoid arthritis (RA). Forty-four women with a mean disease duration of 17.5 years had been treated with low-dose glucocorticoid (prednisone at < 5 mg/day) for at least 12 months. They were studied for an average period of 3 years and 8 months. The remaining 34 women had been treated only with non-steroidal anti-rheumatic drugs (NSAIDs) and served as the control group. Bone mineral density (BMD) in the lumbar spine (L2–4) and femoral neck was measured by dual-energy X-ray absorptiometry (DXA). Reduction of BMD in the lumbar spine was significant in both groups (P < 0.05 ∼ 0.01), but there was no statistically significant difference between the two groups. BMD of the femoral neck decreased significantly (P < 0.05) in the prednisone group, but again the difference was not significant between the two groups. Our data suggest that low-dose prednisone administration probably does not induce significant axial bone loss in female RA patients.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 29 January 1998
Rights and permissions
About this article
Cite this article
Miyamoto, S., Kageyama, Y., Ozeki, T. et al. Effects of glucocorticoids on bone mineral density in rheumatoid arthritis patients . Arch Orth Traum Surg 119, 18–21 (1999). https://doi.org/10.1007/s004020050348
Issue Date:
DOI: https://doi.org/10.1007/s004020050348