Abstract
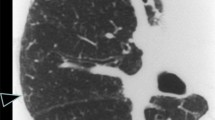
Talc is a mineral widely used in the ceramic, paper, plastics, rubber, paint, and cosmetic industries. Four distinct forms of pulmonary disease caused by talc have been defined. Three of them (talcosilicosis, talcoasbestosis, and pure talcosis) are associated with aspiration and differ in the composition of the inhaled substance. The fourth form, a result of intravenous administration of talc, is seen in drug users who inject medications intended for oral use. The disease most commonly affects men, with a mean age in the fourth decade of life. Presentation of patients with talc granulomatosis can range from asymptomatic to fulminant disease. Symptomatic patients typically present with nonspecific complaints, including progressive exertional dyspnea, and cough. Late complications include chronic respiratory failure, emphysema, pulmonary arterial hypertension, and cor pulmonale. History of occupational exposure or of drug addiction is the major clue to the diagnosis. The high-resolution computed tomography (HRCT) finding of small centrilobular nodules associated with heterogeneous conglomerate masses containing high-density amorphous areas, with or without panlobular emphysema in the lower lobes, is highly suggestive of pulmonary talcosis. The characteristic histopathologic feature in talc pneumoconiosis is the striking appearance of birefringent, needle-shaped particles of talc seen within the giant cells and in the areas of pulmonary fibrosis with the use of polarized light. In conclusion, computed tomography can play an important role in the diagnosis of pulmonary talcosis, since suggestive patterns may be observed. The presence of these patterns in drug abusers or in patients with an occupational history of exposure to talc is highly suggestive of pulmonary talcosis.



Similar content being viewed by others
References
Nam K, Gracey DR (1972) Pulmonary talcosis from cosmetic talcum powder. JAMA 221:492–493
Gibbs AE, Pooley FD, Griffiths DM, Mitha R, Craighead JE, Ruttner JR (1992) Talc pneumoconiosis: a pathologic and mineralogic study. Hum Pathol 23:1344–1354
Marchiori E, Souza AS Jr, Muller NL (2004) Inhalational pulmonary talcosis: high-resolution CT findings in 3 patients. J Thorac Imaging 19(1):41–44
Abraham JL, Brambilla C (1980) Particle size for differentiation between inhalation and injection pulmonary talcosis. Environ Res 21(1):94–96
Feigin DS (1986) Talc: understanding its manifestations in the chest. AJR Am J Roentgenol 146:295–301
Marchiori E, Souza AS Jr, Franquet T, Muller NL (2005) Diffuse high-attenuation pulmonary abnormalities: a pattern-oriented diagnostic approach on high-resolution CT. AJR Am J Roentgenol 184:273–282
Sussman S, Pentz MA, Spruijt-Metz D, Miller T (2006) Misuse of “study drugs”: prevalence, consequences, and implications for policy. Subst Abuse Treat Prev Policy 1:15
Iqbal A, Aggarwal B, Menon B, Kulshreshtha R (2008) Talc granulomatosis mimicking sarcoidosis. Singapore Med J 49:e168–e170
Cruthirds TP, Cole FH, Paul RN (1977) Pulmonary talcosis as a result of massive aspiration of baby powder. South Med J 70:626–628
Marchiori E, Franquet T, Gasparetto TD, Goncalves LP, Escuissato DL (2008) Consolidation with diffuse or focal high attenuation: computed tomography findings. J Thorac Imaging 23:298–304
Ward S, Heyneman LE, Reittner P, Kazerooni EA, Godwin JD, Muller NL (2000) Talcosis associated with IV abuse of oral medications: CT findings. AJR Am J Roentgenol 174:789–793
Low SE, Nicol A (2006) Talc induced pulmonary granulomatosis. J Clin Pathol 59:223
Cook RC, Fradet G, English JC, Soos J, Müller NL, Connolly TP, Levy RD (1998) Recurrence of intravenous talc granulomatosis following single lung transplantation. Can Respir J 5:511–514
Paré JP, Cote G, Fraser RS (1989) Long-term follow-up of drug abusers with intravenous talcosis. Am Rev Respir Dis 139:233–241
Krimsky WS, Dhand S (2008) Pulmonary talc granulomatosis mimicking malignant disease 30 years after last exposure: a case report. J Med Case Report 2:225
Sieniewicz DJ, Nidecker AC (1980) Conglomerate pulmonary disease: a form of talcosis in intravenous methadone abusers. AJR Am J Roentgenol 135:697–702
Caceres M, Braud R, Garrett HE Jr (2009) An unusual presentation of spontaneous pneumothorax secondary to talc-induced pulmonary granulomatosis. Ann Thorac Surg 87:1941–1943
Ben-Haim SA, Ben-Ami H, Edoute Y, Goldstien N, Barzilai D (1988) Talcosis presenting as pulmonary infiltrates in an HIV-positive heroin addict. Chest 94:656–658
Stern EJ, Frank MS, Schmutz JF, Glenny RW, Schmidt RA, Godwin JD (1994) Panlobular pulmonary emphysema caused by i.v. injection of methylphenidate (Ritalin): findings on chest radiographs and CT scans. AJR Am J Roentgenol 162:555–560
Schmidt RA, Glenny RW, Godwin JD, Hampson NB, Cantino ME, Reichenbach DD (1991) Panlobular emphysema in young intravenous Ritalin abusers. Am Rev Respir Dis 143:649–656
Gysbrechts C, Michiels E, Verbeken E, Verschakelen J, Dinsdale D, Nemery B, Demedts M (1998) Interstitial lung disease more than 40 years after a 5 year occupational exposure to talc. Eur Respir J 11:1412–1415
Padley SP, Adler BD, Staples CA, Miller RR, Muller NL (1993) Pulmonary talcosis: CT findings in three cases. Radiology 186:125–127
Shlomi D, Shitrit D, Bendayan D, Sahar G, Shechtman Y, Kramer MR (2008) Successful lung transplantation for talcosis secondary to intravenous abuse of oral drug. Int J Chron Obstruct Pulmon Dis 3:327–330
Akira M, Kozuka T, Yamamoto S, Sakatani M, Morinaga K (2007) Inhalational talc pneumoconiosis: radiographic and CT findings in 14 patients. AJR Am J Roentgenol 188:326–333
Callens SF, Kitetele F, Lelo P, Shabani N, Lusiama J, Wemakoy O, Colebunders R, Behets F, Van Rie A (2007) Pulmonary cystic disease in HIV positive individuals in the Democratic Republic of Congo: three case reports. J Med Case Reports 1:101
Marchiori E, Ferreira A, Saez F, Gabetto JM, Souza AS Jr, Escuissato DL, Gasparetto EL (2006) Conglomerated masses of silicosis in sandblasters: high-resolution CT findings. Eur J Radiol 59:56–59
Chau CH, Yew WW, Lee J (2003) Inhaled budesonide in the treatment of talc-induced pulmonary granulomatosis. Respiration 70:439
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marchiori, E., Lourenço, S., Gasparetto, T.D. et al. Pulmonary Talcosis: Imaging Findings. Lung 188, 165–171 (2010). https://doi.org/10.1007/s00408-010-9230-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-010-9230-y