Abstract
Introduction
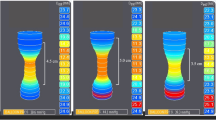
The Endoluminal Functional Lumen Imaging Probe (Endoflip) can be used to provide objective measurements of the gastroesophageal junction during fundoplication, and recent publications have suggested that this device could improve surgical outcomes. However, the impact of operative variables has not been clearly reported. The aim of this study is to determine the effect of these variables on functional lumen imaging probe (FLIP) measurements.
Methods
Following implementation of a standardized operative FLIP protocol, all data were collected prospectively and entered into a quality database. This database was queried for patients undergoing hiatal hernia repair and fundoplication. The protocol utilized various balloon volumes (30 and 40 ml), patient positions (flat and reverse Trendelenburg) and amounts of insufflation (15 mmHg pneumoperitoneum and no pneumoperitoneum).
Results
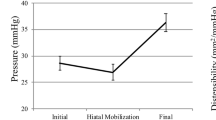
Between August 2018 and February 2020, 97 fundoplications were performed by a single surgeon. Multivariable analysis without interactions demonstrated that a 40 ml volume fill resulted in significantly higher minimum diameter (Dmin), cross-sectional area (CSA), intra-balloon pressure (IBP) and distensibility index (DI) compared to a 30 ml volume fill (p < 0.001). While reverse Trendelenburg positioning resulted in a significantly higher Dmin, IBP and CSA compared to the flat position (all p < 0.05), there was little impact of positioning on DI. Lastly, pneumoperitoneum significantly increased IBP (p < 0.001) but did not affect Dmin (p = 0.697) or CSA (p = 0.757), which resulted in a significant decrease in DI (p < 0.001) when compared to measurements without pneumoperitoneum. Multivariable analysis allowing for interactions demonstrated significant two-way interactions between balloon volume and pneumoperitoneum (p = 0.047), as well as patient position and pneumoperitoneum (p < 0.001).
Conclusion
Surgeons should consider balloon volume and the presence or absence of pneumoperitoneum when interpreting distensibility during or after fundoplication. Additionally, we suggest a formal standardized protocol for FLIP measurements to utilize a 40 ml volume fill in reverse Trendelenburg without pneumoperitoneum.



Similar content being viewed by others
References
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB (2020) Using impedance planimetry (EndoFLIPTM) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34:1761–1768. https://doi.org/10.1007/s00464-019-06925-5
Turner B, Helm M, Hetzel E, Gould JC (2019) Is that “floppy” fundoplication tight enough? Surg Endosc. https://doi.org/10.1007/s00464-019-06947-z
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31:193–198. https://doi.org/10.1007/s00464-016-4956-0
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28:178–182. https://doi.org/10.1097/SLE.0000000000000527
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27:637–644. https://doi.org/10.1111/dote.12130
Nathanson LK, Brunott N, Cavallucci D (2012) Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP®). Surg Endosc 26:1051–1055. https://doi.org/10.1007/s00464-011-1996-3
Teitelbaum EN, Boris L, Arafat FO, Nicodème F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555. https://doi.org/10.1007/s00464-013-3121-2
Kwiatek MA, Kahrilas K, Soper NJ, Bulsiewicz WJ, McMahon BP, Gregersen H, Pandolfino JE (2010) Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg 14:268–276. https://doi.org/10.1007/s11605-009-1086-1
Campagna RAJ, Carlson DA, Hungness ES, Holmstrom AL, Pandolfino JE, Soper NJ, Teitelbaum EN (2019) Intraoperative assessment of esophageal motility using FLIP during myotomy for achalasia. Surg Endosc. https://doi.org/10.1007/s00464-019-07028-x
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr Ujiki received speaker payments from Medtronic for instructional courses on the use of Endoflip. Disclosures outside the scope of this work: Drs. Linn, Haggerty, and Ujiki receive payment for lectures from Gore. Dr. Ujiki is a board member for Boston Scientific, is a paid consultant to Olympus and Apollo, and receives payment for lectures from Apollo and Erbe. Dr. Haggerty received consultant and speaker fees from the renal division of Medtronic for work with peritoneal dialysis catheters and insertion techniques, development of educational materials, and serving as a lecturer and proctor for hands-on courses. Drs. Bailey Su, Mikhail Attaar, Harry Wong, Zachary Callahan, Woody Denham, Ms. Kristine Kuchta and Mr. Stephen Stearns have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, B., Attaar, M., Wong, H. et al. Using a standardized intra-operative endoflip protocol during fundoplication to identify factors that affect distensibility. Surg Endosc 35, 5717–5723 (2021). https://doi.org/10.1007/s00464-020-08034-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08034-0