Abstract
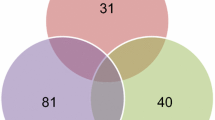
The prognosis of pediatric nephrotic syndrome (NS) correlates with the responsiveness to glucocorticoid therapy. Steroid-resistant NS (SRNS) patients progress to end-stage renal disease, while steroid-sensitive NS (SSNS) and steroid-dependent (SDNS) patients do not. We have performed proteomic profiling of urine samples from a cross section of pediatric and adolescent subjects with SSNS, SRNS, and orthostatic proteinuria (OP) to identify urinary biomarkers of steroid resistance. We performed surface-enhanced laser desorption/ionization time of flight mass spectrometry (SELDI-TOF MS) on urine from 19 subjects with SSNS/SDNS in remission, 14 with SSNS/SDNS in relapse, 5 with SRNS in relapse, and 6 with OP. Genetic algorithm search of principal component space revealed a group of five peaks distinguishing SRNS subjects, with mass/charge (m/z) values of 3,917.07, 4,155.53, 6,329.68, 7,036.96, and 11,117.4. Our analyses identified the peak at m/z 11,117.4 with an accuracy of 95% for classifying SRNS. Multidimensional protein fractionation and mass spectrometric analysis of SRNS urine samples combined with immunodepletion identified the 11,117.4 protein as β2-microglobulin (B2M). Using an unbiased protein profiling approach, we have validated previously reported findings of B2M as a biomarker associated with SRNS. Prospective studies are warranted to establish additional biomarkers that would be predictive of SRNS.





Similar content being viewed by others
Abbreviations
- B2M:
-
β2-Microglobulin
- FSGS:
-
Focal segmental glomerulosclerosis
- GA:
-
Genetic algorithm
- HPRP:
-
High-performance reverse phase
- MALDI:
-
Matrix-assisted laser desorption/ionization
- MS:
-
Mass spectrometry
- m/z :
-
Mass/charge
- NS:
-
Nephrotic syndrome
- OP:
-
Orthostatic proteinuria
- PCA:
-
Principal component analysis
- SD:
-
Steroid dependent
- SDNS:
-
Steroid-dependent nephrotic syndrome
- SELDI:
-
Surface-enhanced laser desorption/ionization
- SR:
-
Steroid resistant
- SRNS:
-
Steroid-resistant nephrotic syndrome
- SS:
-
Steroid sensitive
- SSNS:
-
Steroid-sensitive nephrotic syndrome
- TOF:
-
Time of flight
References
Hogg RJ, Portman RJ, Milliner D, Lemley KV, Eddy A, Ingelfinger J (2000) Evaluation and management of proteinuria and nephrotic syndrome in children: recommendations from a pediatric nephrology panel established at the National Kidney Foundation conference on proteinuria, albuminuria, risk, assessment, detection, and elimination (PARADE). Pediatrics 105:1242–1249
Kim JS, Bellew CA, Silverstein DM, Aviles DH, Boineau FG, Vehaskari VM (2005) High incidence of initial and late steroid resistance in childhood nephrotic syndrome. Kidney Int 68:1275–1281
Schlesinger ER, Sultz HA, Mosher WE, Feldman JG (1968) The nephrotic syndrome. Its incidence and implications for the community. Am J Dis Child 116:623–632
Srivastava T, Simon SD, Alon US (1999) High incidence of focal segmental glomerulosclerosis in nephrotic syndrome of childhood. Pediatr Nephrol 13:13–18
(1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564
(1981) Primary nephrotic syndrome in children: clinical significance of histopathologic variants of minimal change and of diffuse mesangial hypercellularity. A Report of the International Study of Kidney Disease in Children. Kidney Int 20:765–771
Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ (1989) Nephrotic syndrome: from toddlers to twenties. Lancet 1:255–259
Tarshish P, Tobin JN, Bernstein J, Edelmann CM, Jr. (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776
Seikaly M, Ho PL, Emmett L, Tejani A (2001) The 12th Annual Report of the North American Pediatric Renal Transplant Cooperative Study: renal transplantation from 1987 through 1998. Pediatr Transplant 5:215–231
Tejani A, Stablein DH (1992) Recurrence of focal segmental glomerulosclerosis posttransplantation: a special report of the North American Pediatric Renal Transplant Cooperative Study. J Am Soc Nephrol 2:S258–263
Baum MA (2004) Outcomes after renal transplantation for FSGS in children. Pediatr Transplant 8:329–333
Schachter AD, Harmon WE (2001) Single-center analysis of early recurrence of nephrotic syndrome following renal transplantation in children. Pediatr Transplant 5:406–409
Andreoli SP (2004) Racial and ethnic differences in the incidence and progression of focal segmental glomerulosclerosis in children. Adv Ren Replace Ther 11:105–109
Bonilla-Felix M, Parra C, Dajani T, Ferris M, Swinford R, Portman R, Verani R (1999) Changing patterns in the histopathology of idiopathic nephrotic syndrome in children. Kidney Int 55:1885–1890
Rennke HG (1994) How does glomerular epithelial cell injury contribute to progressive glomerular damage? Kidney Int Suppl 45:S58–63
Petricoin EF, Ardekani AM, Hitt BA, Levine PJ, Fusaro VA, Steinberg SM, Mills GB, Simone C, Fishman DA, Kohn EC, Liotta LA (2002) Use of proteomic patterns in serum to identify ovarian cancer. Lancet 359:572–577
Petricoin EF, 3rd, Ornstein DK, Paweletz CP, Ardekani A, Hackett PS, Hitt BA, Velassco A, Trucco C, Wiegand L, Wood K, Simone CB, Levine PJ, Linehan WM, Emmert-Buck MR, Steinberg SM, Kohn EC, Liotta LA (2002) Serum proteomic patterns for detection of prostate cancer. J Natl Cancer Inst 94:1576–1578
Won Y, Song HJ, Kang TW, Kim JJ, Han BD, Lee SW (2003) Pattern analysis of serum proteome distinguishes renal cell carcinoma from other urologic diseases and healthy persons. Proteomics 3:2310–2316
Huber M, Bahr I, Kratzschmar JR, Becker A, Muller EC, Donner P, Pohlenz HD, Schneider MR, Sommer A (2004) Comparison of proteomic and genomic analyses of the human breast cancer cell line T47D and the antiestrogen-resistant derivative T47D-r. Mol Cell Proteomics 3:43–55
Xu BJ, Shyr Y, Liang X, Ma LJ, Donnert EM, Roberts JD, Zhang X, Kon V, Brown NJ, Caprioli RM, Fogo AB (2005) Proteomic patterns and prediction of glomerulosclerosis and its mechanisms. J Am Soc Nephrol 16:2967–2975
Schaub S, Wilkins J, Weiler T, Sangster K, Rush D, Nickerson P (2004) Urine protein profiling with surface-enhanced laser-desorption/ionization time-of-flight mass spectrometry. Kidney Int 65:323–332
Traum AZ, Wells MP, Aivado M, Libermann TA, Ramoni MF, Schachter AD (2006) SELDI-TOF MS of quadruplicate urine and serum samples to evaluate changes related to storage conditions. Proteomics 6:1676–1680
O’Riordan E, Orlova TN, Mei JJ, Butt K, Chander PM, Rahman S, Mya M, Hu R, Momin J, Eng EW, Hampel DJ, Hartman B, Kretzler M, Delaney V, Goligorsky MS (2004) Bioinformatic analysis of the urine proteome of acute allograft rejection. J Am Soc Nephrol 15:3240–3248
Nguyen MT, Ross GF, Dent CL, Devarajan P (2005) Early prediction of acute renal injury using urinary proteomics. Am J Nephrol 25:318–326
Haubitz M, Wittke S, Weissinger EM, Walden M, Rupprecht HD, Floege J, Haller H, Mischak H (2005) Urine protein patterns can serve as diagnostic tools in patients with IgA nephropathy. Kidney Int 67:2313–2320
Winston PH (1992) Learning by simulating evolution. In: Katz B (ed) Artificial intelligence. Addison-Wesley, Reading, MA, pp 505–528
R Development Core Team (2005) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Arbus GS, Poucell S, Bacheyie GS, Baumal R (1982) Focal segmental glomerulosclerosis with idiopathic nephrotic syndrome: three types of clinical response. J Pediatr 101:40–45
Schulman SL, Kaiser BA, Polinsky MS, Srinivasan R, Baluarte HJ (1988) Predicting the response to cytotoxic therapy for childhood nephrotic syndrome: superiority of response to corticosteroid therapy over histopathologic patterns. J Pediatr 113:996–1001
Branten AJ, du Buf-Vereijken PW, Klasen IS, Bosch FH, Feith GW, Hollander DA, Wetzels JF (2005) Urinary excretion of beta2-microglobulin and IgG predict prognosis in idiopathic membranous nephropathy: a validation study. J Am Soc Nephrol 16:169–174
Caliskan S, Hacibekiroglu M, Sever L, Ozbay G, Arisoy N (1996) Urinary N-acetyl-beta-D-glucosaminidase and beta 2-microglobulin excretion in primary nephrotic children. Nephron 74:401–404
Fede C, Conti G, Chimenz R, Ricca M (1999) N-acetyl-beta-D-glucosaminidase and beta2-microglobulin: prognostic markers in idiopathic nephrotic syndrome. J Nephrol 12:51–55
Ramjee G, Coovadia HM, Adhikari M (1994) Sodium dodecyl sulphate polyacrylamide gel electrophoresis of urinary proteins in steroid-responsive and steroid-resistant nephrotic syndrome in children. Pediatr Nephrol 8:653–656
Reichert LJ, Koene RA, Wetzels JF (1995) Urinary excretion of beta 2-microglobulin predicts renal outcome in patients with idiopathic membranous nephropathy. J Am Soc Nephrol 6:1666–1669
Reichert LJ, Koene RA, Wetzels JF (1999) Acute haemodynamic and proteinuric effects of prednisolone in patients with a nephrotic syndrome. Nephrol Dial Transplant 14:91–97
Robeva R, Heslan JM, Branellec A, Laurent J, Lagrue G (1988) Enhanced beta 2-microglobulin levels in lymphocyte culture supernatants from patients with idiopathic nephrotic syndrome: inhibition of lymphocyte activation by cyclosporine. Clin Nephrol 30:211–215
Sesso R, Santos AP, Nishida SK, Klag MJ, Carvalhaes JT, Ajzen H, Ramos OL, Pereira AB (1992) Prediction of steroid responsiveness in the idiopathic nephrotic syndrome using urinary retinol-binding protein and beta-2-microglobulin. Ann Intern Med 116:905–909
Thielemans N, Lauwerys R, Bernard A (1994) Competition between albumin and low-molecular-weight proteins for renal tubular uptake in experimental nephropathies. Nephron 66:453–458
Valles P, Peralta M, Carrizo L, Martin L, Principi I, Gonzalez A, Manucha W (2000) Follow-up of steroid-resistant nephrotic syndrome: tubular proteinuria and enzymuria. Pediatr Nephrol 15:252–258
Wetzels JF, Sluiter HE, Hoitsma AJ, van Munster PJ, Koene RA (1988) Prednisolone can increase glomerular permeability to proteins in nephrotic syndrome. Kidney Int 33:1169–1174
Bokenkamp A, Grabensee A, Stoffel-Wagner B, Hasan C, Henne T, Offner G, Lentze MJ (2002) The beta2-microglobulin/cystatin C ratio-a potential marker of post-transplant lymphoproliferative disease. Clin Nephrol 58:417–422
Karlsson FA, Wibell L, Evrin PE (1980) beta 2-Microglobulin in clinical medicine. Scand J Clin Lab Invest Suppl 154:27–37
Sasaki TM, Pirsch JD, D’Alessandro AM, Knechtle SJ, Kalayoglu M, Hafez GR, Sollinger HW (1997) Increased beta 2-microglobulin (B2M) is useful in the detection of post-transplant lymphoproliferative disease (PTLD). Clin Transplant 11:29–33
Roxe DM, Siddiqui F, Santhanam S, del Greco F, Wolf J (1981) Rationale and application of beta-2-microglobulin measurements to detect acute transplant rejection. Nephron 27:260–264
Schardijn GH, Statius van Eps LW (1987) Beta 2-microglobulin: its significance in the evaluation of renal function. Kidney Int 32:635–641
Woo KT, Lee EJ, Lau YK, Lim CH (1985) Beta-2-microglobulin in the assessment of renal function of the transplanted kidney. Nephron 39:223–227
Rai AJ, Stemmer PM, Zhang Z, Adam BL, Morgan WT, Caffrey RE, Podust VN, Patel M, Lim LY, Shipulina NV, Chan DW, Semmes OJ, Eastwood Leung HC (2005) Analysis of Human Proteome Organization Plasma Proteome Project (HUPO PPP) reference specimens using surface enhanced laser desorption/ionization-time of flight (SELDI-TOF) mass spectrometry: multi-institution correlation of spectra and identification of biomarkers. Proteomics 5:3467–3474
Semmes OJ, Feng Z, Adam BL, Banez LL, Bigbee WL, Campos D, Cazares LH, Chan DW, Grizzle WE, Izbicka E, Kagan J, Malik G, McLerran D, Moul JW, Partin A, Prasanna P, Rosenzweig J, Sokoll LJ, Srivastava S, Thompson I, Welsh MJ, White N, Winget M, Yasui Y, Zhang Z, Zhu L (2005) Evaluation of serum protein profiling by surface-enhanced laser desorption/ionization time-of-flight mass spectrometry for the detection of prostate cancer: I. Assessment of platform reproducibility. Clin Chem 51:102–112
Schaub S, Wilkins JA, Antonovici M, Krokhin O, Weiler T, Rush D, Nickerson P (2005) Proteomic-based identification of cleaved urinary beta2-microglobulin as a potential marker for acute tubular injury in renal allografts. Am J Transplant 5:729–738
Schachter AD (2004) The pediatric nephrotic syndrome spectrum: clinical homogeneity and molecular heterogeneity. Pediatr Transplant 8:344–348
Acknowledgements
This work was supported in part by NIH Training Grant T32 DK 007726 (MK and AZT), and by NIH grant K23 RR 16080 (ADS). Parts of this work were presented (abstract TH-PO160) at the American Society of Nephrology Renal Week 2005, Philadelphia, PA.
Author information
Authors and Affiliations
Corresponding author
Additional information
MK and AZT contributed equally to this work.
Rights and permissions
About this article
Cite this article
Khurana, M., Traum, A.Z., Aivado, M. et al. Urine proteomic profiling of pediatric nephrotic syndrome. Pediatr Nephrol 21, 1257–1265 (2006). https://doi.org/10.1007/s00467-006-0165-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0165-8