Abstract
Purpose
To examine the methods and results of treatment in patients with an open abdomen (OA) at a single institution where an absorbable mesh closure (AMC) is most commonly used.
Methods
A retrospective study was performed in OA patients from January 2001 to June 2007. Outcomes were analyzed in terms of enteroatmospheric fistula (EAF) formation and survival.
Results
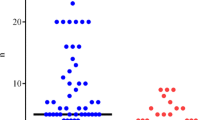
There were 73 OA patients receiving definitive closures (40 trauma and 33 nontrauma). Twenty-four patients were able to undergo a delayed primary fascial closure (DPFC) after initial vacuum pack closure (DPFC rate 33%). The DPFC rate was significantly lower in patients with an associated infection or contamination (9% vs 44%, P = 0.002). The EAF and mortality rates of the DPFC group were 0% and 13%, respectively. Absorbable mesh closure was used in 41 of 49 patients who failed DPFC (84%). There were 9 patients who had EAF (overall EAF rate 12%), 6 of whom were in the AMC group (EAF rate 15%). The overall and AMC group mortality rates were 29% and 37%, respectively.
Conclusion
Absorbable mesh closure carries high EAF and mortality rates. Therefore, DPFC should be considered as the primary closure method. Absorbable mesh closure should be reserved for patients who fail DPFC, especially those with peritonitis or contamination.
Similar content being viewed by others
References
Costa AD. Making a virtue of necessity: managing the open abdomen. ANZ J Surg 2006;76:356–363.
Fabian TC. Damage control in trauma: laparotomy wound management acute to chronic. Surg Clin North Am 2007;87:73–93.
Schecter WP, Ivatury RR, Rotondo MF, Hirshberg A. Open abdomen after trauma and abdominal sepsis: a strategy for management. J Am Coll Surg 2006;3:390–396.
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR 3rd, Fruchterman TM, Kauder DR, et al. “Damage control”: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993;35:375–382.
Stone HH, Strom PR, Mullins RJ. Management of the major coagulopathy with onset during laparotomy. Ann Surg 1983; 197:532–535.
Deenichin GP. Abdominal compartment syndrome. Surg Today 2008;38:5–19.
Djavani K, Wanhainen A, Bjorck M. Intra-abdominal hypertension and abdominal compartment syndrome following surgery for ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 2006;31:581–584.
Fabian TC, Croce MA, Pritchard FE, Minard G, Hickerson WL, Howell RL, et al. Planned ventral hernia staged management for acute abdominal wall defects. Ann Surg 1994;219:643–653.
Mayberry JC, Burgess EA, Goldman RK, Pearson TE, Brand D, Mullins RJ, et al. Enterocutaneous fistula and ventral hernia after absorbable mesh prosthesis closure for trauma: the plain truth. J Trauma 2004;57:157–163.
Sriussadaporn S, Pak-art R, Bunjongsat S. Immediate closure of open abdomen with bilateral bipedicle anterior abdominal skin flaps and subsequent retrorectus prosthetic mesh repair of the late giant ventral hernias. J Trauma 2003;54:1083–1089.
Jernigan TW, Fabian TC, Croce MA, Moore N, Pritchard FE, Minard G, et al. Staged management of giant abdominal wall defects: Acute and long term results. Ann Surg 2003;238:349–357.
Barker DE, Kaufman HJ, Smith LA, Ciraulo DL, Richart CL, Burns RP, et al. Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma 2000;48:201–206.
Barker DE, Green JM, Maxwell RA, Smith PW, Mejia VA, Dart BW, et al. Experience with vacuum-pack temporary abdominal wound closure in 258 trauma and general and vascular surgical patients. J Am Coll Surg 2007;204:784–793.
Suliburk JW, Ware DN, Balogh Z, McKinley BA, Cocanour CS, Kozar RA, et al. Vacuum-assisted wound closure achieves early fascial closure of open abdomens after severe trauma. J Trauma 2003;55:1155–1160.
Miller PR, Meredith JW, Johnson JC, Chang MC. Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg 2004;239:608–614.
Cothren CC, Moore EE, Johnson JL, Moore JB, Burch JM. One hundred percent fascial approximation with sequential abdominal closure of open abdomen. Am J Surg 2006;192:238–242.
Ekeh AP, McCarthy MC, Woods RJ, Walusimbi M, Saxe JM, Patterson LA. Delayed closure of ventral abdominal hernias after severe trauma. Am J Surg 2006;191:391–395.
Petersson U, Acosta S, Björck M. Vacuum-assisted wound closure and mesh-mediated fascial traction-a novel technique for late closure of the open abdomen. World J Surg 2007;31:2133–2137.
Ramirez OM, Raus E, Dellon AL. “Component separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 1990;86:519–526.
Kushimoto S, Yamamoto Y, Aiboshi J, Ogawa F, Koido Y, Yoshida R, et al. Usefulness of the bilateral anterior rectus abdominis sheath turnover flap method for early fascial closure in patients requiring open abdominal management. World J Surg 2007;31:2–8.
Miller RS, Morris JA, Diaz JJ, Herring MB, May AK. Complications after 344 damage-control open celiotomies. J Trauma 2005;59:1365–1374.
Cipolla J, Stawicki SP, Hoff WS, McQuay N, Hoey BA, Wainwright G, et al. A proposed algorithm for managing the open abdomen. Am Surg 2005;71:202–207.
Sriussadaporn S, Sriussadaporn S, Kritayakirana K, Park-art R. Operative management of small bowel fistulae associated with open abdomen. Asian J Surg 2006;29:1–7.
Scott BG, Welsh FJ, Pham HQ, Carrick MM, Liscum KR, Granchi TS, et al. Early aggressive closure of the open abdomen. J Trauma 2006;60:17–22.
Kim H, Bruen K, Vargo D. Acellular dermal matrix in the management of high-risk abdominal wall defects. Am J Surg 2006; 192:705–709.
Schuster R, Singh J, Safadi BY, Wren SM. The use of acellular dermal matrix for contaminated abdominal wall defects: wound status predicts success. Am J Surg 2006;192:594–597.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Prichayudh, S., Sriussadaporn, S., Samorn, P. et al. Management of open abdomen with an absorbable mesh closure. Surg Today 41, 72–78 (2011). https://doi.org/10.1007/s00595-009-4202-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-009-4202-7