Abstract
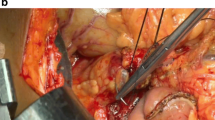
The factors influencing the healing process of pancreaticojejunostomy (P-J) following pancreaticoduodenectomy (PD) are still ill defined, allowing the recommendation of various anastomotic methods. We conduced a prospective study to determine the risk factors influencing the protracted healing of P-J, examining 100 consecutive patients who underwent PD followed by P-J, performed as an end-to-side “mucosa-to-mucosa” anastomosis using vertical mattress sutures (VMS method). Protracted healing of P-J was classified as either peripancreatic sepsis (PPS), defined as prolonged suppurative discharge of less than 50 ml a day from the drain beneath the P-J for more than 1 week; or a pancreatic fistula (PF), defined as prolonged discharge of more than 50 ml a day with a high amylase content (>1000 IU) for more than 1 week. There were 80 patients with a malignant neoplasm, and 20 with benign disease. The overall incidence of healing problems following P-J was 9%, which included 6 patients (6%) with PPS and 3 (3%) with PF. Apart from an advanced age of more than 70 years, none of the patients' characteristics or postoperative complications influenced the healing of P-J. The type of reconstruction, an anastomotic stent, the duct size, and a “soft” pancreas were not risk factors either. In conclusion, no factors, apart from the age or any special problem of an individual patient, influenced the dehiscence of P-J when the VMS method was used after PD.
Similar content being viewed by others
References
Grace PA, Pitt HA, Tompkins DK (1986) Decreased morbidity and mortality after pancreatoduodenectomy. Am J Surg 151:141–149
Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Colemanand J (1993) One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg 217:430–448
del Castillo CF, Rattner DW, Warshaw AL (1995) Standards for pancreatic resection in the 1990s. Arch Surg 130:295–300
Cullen JJ, Sarr MG, Ilstrup DM (1994) Pancreatic anastomotic leak after pancreaticoduodenectomy: incidence, significance, and management. Am J Surg 168:295–298
Martin FM, Rossi RL, Munson JL (1989) Management of pancreatic fistulas. Arch Surg 124:571–573
Miedema BW, Sarr MG, van Heerden JA (1992) Complications following pancreaticoduodenectomy. Current management. Arch Surg 127:945–949.
Lerult JP, Gianello PR, Otte JB, Kestens PJ (1984) Pancreaticoduodenal resection: surgical experience and evaluation of risk factors in 103 patients. Ann Surg 199:432–437
Coopermen AM, Hoerr SO (1978) Cancer of the pancreatic region. In: Cooperman AM, Hoerr SO (eds) Surgery of the pancreas. A text and atlas. Mosby, St. Louis pp 185–186
Matsumoto Y, Fujii H, Miura K, Inoue S (1992) Successful pancreatojejunal anastomosis for pancreatoduodenectomy. Surg Gynecol Obstet 175:555–562
Marcus SC, Cohen H, Ranson JC (1995) Optimal management of the pancreatic remmant after pancreaticoduodenectomy. Ann Surg 221:635–648
Gambee LP (1956) Ten years' experience with a single layer anastomosis in colon surgery. Am J Surg 92:222–227
Maetani S (1972) Modified method of pancreaticojejunal anastomosis following pancreatoduodenectomy. Sur Gynecol Obstet 134:1003–1004
Matsusue S, Kashihara S, Kuramoto S, Tanaka H, Nakamura Y, Sakai S, Nishikawa H, Masumoto H, Maetani S (1980) Pancreacticoduodenectomy and pancreaticojunostomy (in Japanese). Nihon Shoukakigeka Gakkai Zasshi (Jpn J Gastroent Surg) 13:379–1384
Matsusue S (1982) Healing process and patency of pancreaticojejunostomy following pancreaticoduodenectomy (in Japanese with English abstract). Nippon Geka Gakkai Zasshi (J Jpn Surg Soc) 83:760–768
Matsusue S, Nishimura S, Koizumi S, Nakamura T, Takeda H (1995) Preventive effect of simultaneously infused lipid against thrombophlebitis during postoperative peripheral parenteral nutrition. Surg Today 25:667–671
Warshaw AL (1995) Pancreatic surgery. A paradigm for progress in the age of the bottom line. Arch Surg 130:240–246
Nakase A, Matsumoto Y, Uchida K, Honjo I (1977) Surgical treatment of cancer of the pancreas in Japan. Ann Surg 185:52–57
Biehl T, Traverso L (1992) Is stenting necessary for a successfl pancreatic anastomosis? Am J Surg 163:530–532
Matsusue S, Walser M (1992) Healing of intestinal anastomoses in adrenalectomized rats given corticosterone. Am J Physiol 263 (Regul Integr Comp Physiol 32):R164-R168
Holbrook RF, Hargrave K, Traverso LW (1996) A prospective cost analysis of pancreaticoduodenectomy. Am J Surg 171:508–511
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Matsusue, S., Takeda, H., Nakamura, Y. et al. A prospective analysis of the factors influencing pancreaticojejunostomy performed using a single method, in 100 consecutive pancreaticoduodenectomies. Surg Today 28, 719–726 (1998). https://doi.org/10.1007/BF02484618
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02484618