Abstract
Background
Endoscopic resection for early gastric cancer (EGC) plays a central role in the treatment of EGC in Japan. However, there is still room for improvement, and it is necessary to summarize the recently obtained knowledge from Japan for further improvement.
Methods
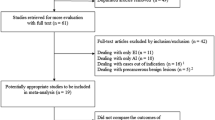
We conducted a PubMed search to select relevant articles in the 5 years until September 18, 2016, using the keywords “gastric cancer” and “endoscopic treatment,” “endoscopic submucosal dissection,” “endoscopic mucosal resection,” or “polypectomy” and filtering article types as “clinical study” or “clinical trial.”
Results
Among the 329 articles selected automatically from the keywords “polypectomy” (1 article), “endoscopic mucosal resection” (29 articles), “endoscopic submucosal dissection” (77 articles), and “endoscopic treatment” (222 articles) in combination with “gastric cancer,” 32 relevant articles from Japanese investigators were chosen. Seven articles were categorized into “equipment,” 4 into “preparation and sedation,” 17 into “complications and their prevention,” and 4 into “therapeutic outcomes.” Among them, CO2 insufflation, propofol sedation, and how to prevent post-endoscopic submucosal dissection (ESD) ulcer bleeding and achieve post-ESD ulcer healing were intensively investigated. Long-term outcomes of endoscopic mucosal resection and ESD were also reported as favorable outcomes.
Conclusions
Endoscopic resection for EGC is still developing toward an ideal form, pursuing a more reliable, safer, and faster minimally invasive treatment.
Similar content being viewed by others
Introduction
The Japanese have made great efforts to overcome gastric cancer for several decades. However, gastric cancer morbidity and mortality in Japan are still high, and the latest statistics for the Japanese population revealed that gastric cancer was the second commonest cancer in 2012 (132,159 cases) and the third leading cause of cancer-related deaths in 2014 (47,903 cases) [1]. Helicobacter pylori eradication therapy is now widely performed, and the infection rate in the younger generation has dramatically decreased in Japan, which will lead to substantial reduction of gastric cancer incidence and death in the future. In the meantime, our strategy to prevent gastric cancer death should be mainly early detection and curative treatment, preferably by use of endoscopic resection methods, considering the patient’s quality of life. Owing to the development of endoscopic technology, it is estimated that approximately 42,000 endoscopic resections [30 polypectomies, 234 endoscopic mucosal resections (EMRs), and 3241 endoscopic submucosal dissections (ESDs) in June 2015] for early gastric cancer (EGC) are performed yearly in Japan [2]. Although endoscopic resection is well accepted as a standard treatment for EGC without possible lymph node metastasis, Japanese researchers still pursue greater improvement toward the ideal form. In this review, knowledge accumulated in the last 5 years from Japan is summarized.
Methods
PubMed (http://www.ncbi.nlm.nih.gov/pubmed) was used to perform electronic searches of the literature. The search included all English-language entries in the 5 years until September 18, 2016. The following keywords were used in all fields: “gastric cancer” and “endoscopic treatment,” “endoscopic submucosal dissection,” “endoscopic mucosal resection,” or “polypectomy.” To select only clinical evidence, filtering of article types as “clinical study” or “clinical trial” was done.
Results
A PubMed search with the keywords “polypectomy,” “endoscopic mucosal resection,” “endoscopic submucosal dissection,” or “endoscopic treatment, in combination with “gastric cancer” automatically picked up 1, 29, 77, and 222 articles respectively. After assessment of the titles, abstracts, and full texts, 32 relevant articles from Japanese investigators regarding endoscopic treatments for EGC were identified. They were categorized into “equipment,” “preparation and sedation,” “complications and their prevention,” and “therapeutic outcomes” as follows.
Equipment
Two studies [one randomized controlled trial (RCT) and one case series study] regarding videoendoscopes were identified [3, 4]. Tatsumi et al. [3] compared the water-jet videoendoscope with a conventional videoendoscope under the hypothesis that the former would shorten the procedure time, but they did not reveal a significantly shorter procedure time with use of the water-jet videoendoscope (median 51 min vs 62 min, p = 0.201). Higuchi et al. [4] reported the good outcomes of 30 patients with an ulcer scar (100 % of the en bloc resection rate without serious adverse events) by use of double-endoscope ESD (the water-jet videoendoscope as the main operation endoscope and an ultrathin videoendoscope as a lesion traction endoscope).
Three RCTs regarding CO2 insufflation were identified [5–7]. Takada et al. [5] revealed similar levels of transcutaneous CO2 tension and arterial blood CO2 partial pressure during and shortly after ESD in the CO2 group and in the air group in patients without severe pulmonary dysfunction. Maeda et al. [6] revealed that CO2 insufflation significantly reduced the volume of intestinal gas but not the visual analog scale score of abdominal pain and distension shortly after ESD compared with air insufflation. They speculated the unexpected results regarding pain and distention derived from sufficient sedation and analgesia during ESD. Mori et al. [7] revealed that duodenal occlusion by a balloon further reduced the amount of intestinal gas and the visual analog scale score of nausea due to abdominal distension shortly after ESD.
Two studies (one RCT and one case series study) regarding submucosal injection solution were identified [8, 9]. Sumiyama et al. [8] could not reveal the usefulness of a thiol compound called mesna, which chemically softens the connective tissue, over normal saline with regard to the time for submucosal dissection (mean 18.62 min vs 24.58 min, p = 0.128) [8]. Kusano et al. [9] showed possible application of 0.6 % sodium alginate, which is used as a safe viscosity-enhancing stabilizer and coagulator, anti-peptic ulcer agent, and hemostatic agent, as a submucosal injection solution.
Preparation and sedation
As the preparation for ESD, gastric irrigation with 2 L saline solution before the start of ESD significantly reduced the white blood cell counts and the severity of fever and pain at 1 day after ESD in an RCT setting [10]. In terms of gastric peristaltic inhibition, l-menthol, which relaxes gastrointestinal tract smooth muscle cells immediately after it has been sprayed on the gastric wall, successfully inhibited gastric peristalsis during ESD in an RCT setting, but similar outcomes regarding procedure time, efficacy, and safety were obtained in both the l-menthol group and the placebo group [11].
Two studies regarding propofol sedation (one RCT and one case series study) were identified [12, 13]. Sasaki et al. [12] revealed that propofol had modest advantages over midazolam in terms of safety and efficacy during ESD, but significantly earlier recovery from sedation was obtained in the propofol group. Gotoda et al. [13] reported possible safety and efficacy of gastroenterologist-guided propofol sedation even for elderly patients by retrospective medical record reviews.
Complications and their prevention
The overall ESD-related complication rate was 4.0 %, based on a national administrative database from a total of 27,385 patients at 867 hospitals in Japan from 2009 to 2011 [14]. In that study there was no significant difference in complications between elderly (80 years or older; n = 5525) and nonelderly (younger than 80 years; n = 21,860) patients (4.3 % vs 3.9 %, p = 0.152), although the risk-adjusted length of hospital stay was significantly longer and medical costs during hospitalization were significantly higher in elderly patients. The most frequent complication was bleeding, followed by perforation, aspiration pneumonia, and ischemic disease.
Accordingly, post-ESD ulcer bleeding and healing are recent major research fields in this category. As new attempts to prevent post-ESD ulcer bleeding, TDM-621 (a synthetic infectious-agent-free peptide) and a shielding method that used polyglycolic acid sheets and fibrin glue were tested in clinical trials [15, 16]. The former, applied through an endoscopic catheter, was used for oozing hemorrhage during ESD, showing promising results in 12 patients [15]. The latter was used to cover the mucosal defect immediately after ESD for prevention of post-ESD ulcer bleeding. The post-ESD ulcers in high-risk patients (antithrombotic users or patients with large tumors) showed at a bleeding rate of 6.7 %, which was significantly reduced in comparison with the rate in with the historical control group [16].
A different approach to lessen post-ESD bleeding was taken by Yoshida et al. [17] to detect the nonbleeding visible vessels effectively by use of an infrared imaging system. They revealed that blue points did not need coagulation and gray points had a potential risk of bleeding and needed preventative hemostasis.
The necessity of scheduled second-look endoscopy at 1 day after ESD was investigated in an RCT setting [18]. According to this study, second-look endoscopy without any suspicion of post-ESD ulcer bleeding was not routinely recommended because it did not contribute to the prevention of post-ESD ulcer bleeding thereafter for patients with an average bleeding risk.
Three RCTs regarding antisecretory agents for prevention of post-ESD ulcer bleeding were identified [19–21]. Proton pump inhibitor (PPI) administration starting 3 days before ESD could not reduce post-ESD ulcer bleeding compared with PPI administration starting on the day of the procedure [19]. Because conflicting results were reported in terms of the effects of PPIs and histamine H2 receptor antagonists (H2RAs) for prevention of post-ESD ulcer bleeding and for post-ESD ulcer healing, Imaeda et al. [20] and Tomita et al. [21] compared them, but could not reveal the superiority of PPIs over H2 receptor antagonists H2RAs with regard to both post-ESD ulcer bleeding and post-ESD ulcer healing.
Five RCTs regarding post-ESD ulcer healing were identified [22–26]. Arai et al. [22] revealed that 2 weeks of PPI treatment had effects similar to those of 4 weeks of PPI treatment with regard to post-ESD ulcer healing. Takayama et al. [23] revealed that 1 week of PPI treatment followed by 7 weeks of rebamipide treatment had effects similar to those of 8 weeks of PPI treatment with regard to post-ESD ulcer healing. Kobayashi et al. [24] compared 8 weeks of treatment with a PPI alone and 8 weeks of treatment with a PPI plus rebamipide. Although ulcer healing was evaluated 4–6 weeks after ESD, the healing ratio with regard to scar stage was similar in both groups, but the quality of basal healing was significantly better in the combination group among patients with large resection in the subanalysis. Nakamura et al. [25] revealed the ratio of progression to the healing stage in the PPI plus rebamipide group was significantly higher, especially at an early stage, compared with 8 weeks of treatment with a PPI alone and 4 weeks of PPI treatment plus 8 weeks of rebamipide treatment. Higuchi et al. [26] compared 8 weeks of PPI treatment with 1 week of H. pylori eradication therapy and rebamipide treatment for the subsequent 7 weeks. Although no adverse effect was observed in both groups, the healing ratio with regard to scar stage at 8 weeks after ESD was significantly higher in the PPI group. However, the combination therapy of eradication therapy and rebamipide was an optimal therapeutic option for healing smaller ulcers in the subanalysis [26]. As the risk factors of delayed healing with PPI monotherapy at 4 weeks after ESD, submucosal fibrosis and injury of the proper muscle layer during ESD were identified by a single-center retrospective study [27].
Regarding other complications, three studies were identified [28–30]. Watari et al. [28] investigated the incidence of “silent” free air and aspiration pneumonia detected by CT after ESD. Silent free air without endoscopic perforation and aspiration pneumonia were detected in 37.3 and 6.6 % of all ESD cases respectively. These findings were observed more in patients with a longer procedure time, although they had little effect on the patient’s treatment and length of hospitalization. Mori et al. [29] evaluated the effect of local steroid injection immediately after ESD on granulation formation and gastric deformity. They concluded that local steroid injection might promote the formation of flat and sufficient granulation tissue without fibrotic contraction, which caused less deformity in the stomach. Higuchi et al. [30] investigated whether gastric motility was affected by ESD. Their study revealed that ESD did not significantly affect any of the gastric emptying parameters measured by the [13C]octanoic acid breath test.
Therapeutic outcomes
Four studies regarding short-term and/or long-term outcomes in specific or general ESD patients were identified [31–34]. As the short-term outcomes in patients at high risk of thromboembolism who were regularly taking antiplatelet agents, Ono et al. [31] reported a 26 % post-ESD ulcer bleeding rate, which led to early termination of the prospective cohort study. All bleeding complications occurred at a mean of 11.2 days after ESD, after resumption of thienopyridine derivative therapy postoperatively (start at a mean of 2.3 days after ESD).They confirmed that the administration of thienopyridine derivatives and that of multiple agents were significant factors contributing to the bleeding complications (p < 0.05).
By using long-term outcomes in patients with secondary ESD (sESD) after noncurative resection with positive lateral margins at the initial ESD, Hoteya et al. [32] investigated the optimal timing of the sESD. Although both early sESD (performed shortly after the initial ESD; mean of 9 days after the initial ESD) and late sESD (performed after the detection of recurrent tumors; mean of 685 days after the initial ESD) showed good outcomes with no severe complications (curative resection rates of 100 and 86.7 % respectively), the dissection speed was faster in early sESD group.
As long-term outcomes in general EMR and ESD patients, Tanabe et al. [33] revealed that the 5-year residual-tumor-free/recurrence-free rate was significantly higher in the ESD group than in the EMR group (99.5 % vs 96.6 %; p < 0.05), although the overall survival curves were similar. For metachronous gastric cancer development, Kawanaka et al. [34] revealed that H. pylori eradication did not produce significant changes in the molecular alterations related to carcinogenesis, including microsatellite instability, suggesting that H. pylori eradication might not prevent the development of metachronous gastric cancers in background mucosa with intestinal metaplasia where EGCs indicating ESD commonly develop.
Discussion
Endoscopic resection, mainly ESD, has had a great impact on gastric cancer treatment strategies and, in recent years, it is estimated that approximately one third of all gastric cancers have been treated by endoscopic resection in Japan. Selection of polypectomy, EMR, or ESD among endoscopic resection is not still clearly determined, but most cases, even small lesions without fibrosis, are treated by ESD. This is because ESD is a more reliable technique for en bloc plus R0 resection of any lesion, resulting in more precise histological assessment of resected tumors and lower residual/recurrent tumor rates [33]. Although gastric ESD is generally considered in the near completion stage with a small room for improvement, major unmet needs still exist, which are greater reduction of the procedure time and more enhanced safety.
To shorten the procedure time, the recent trend is to use a traction method. Besides the double-endoscope method [4], various types of traction methods have been investigated without conclusive outcomes [35]. These techniques would be useful for complex lesions (e.g., fibrotic lesions) or difficult locations (e.g., greater curvature in the body, the fornix, prepylorus), and further clinical studies to reveal the appropriate application of the best methods are warranted.
To obtain enhanced safety during ESD, CO2 insufflation and propofol sedation have been mainly investigated. It was difficult to show clinical advantages of CO2 insufflation for skillful endoscopists without perforation in two studies [5, 6], but it seems to be useful for beginner endoscopists with a longer procedure time and greater possibility of perforation. Perforation itself is manageable even when air insufflation is used, and it is speculated that the possibility to lead to subsequent deteriorated status should be low when CO2 insufflation is used [36]. Propofol sedation is widely used for gastrointestinal tract endoscopy in Western countries, but its use in endoscopic practices in Japan is uncommon, because administration of propofol by endoscopists is very restricted because of a government regulation and anesthesiologists rarely come to an endoscopy unit. However, we recognize the use seems to be convenient and safe from two studies [12, 13]. The evidence will hopefully lead to common use of propofol sedation for, at least, therapeutic endoscopy, including gastric ESD, in Japan.
As post-ESD complications, post-ESD ulcer bleeding is still a major problem. As shown by a study of patients with high risk of thromboembolism [31], we have to recognize that the strategy to raise intragastric pH by use of antisecretory agents (PPI or H2RA) seems to have limitations in preventing bleeding complications [19–21]. A synergic effect with another approach, such as a shielding method [16], is necessary. Several studies have targeted post-ESD ulcer healing as a primary end point by using antisecretory agents and/or mucoprotective agents [23–27]. These studies clearly elucidated the difference between peptic ulcer and artificial post-ESD ulcer. Acid suppression is not so important for the healing process after the bleeding phase (1–2 weeks after ESD). Although these studies are very interesting to understand the mechanisms of ulcer healing, clinical significance seems to be low except for stricture formation. In case of stricture, the standpoint of local steroid injection on the ulcer base after ESD should be investigated, although stricture formation in the wide gastric lumen is infrequently experienced.
Although single-center retrospective studies showed excellent long-term outcomes of gastric ESD patients with expanded criteria, regardless of the size, ulcerative findings, and histological types [33, 37, 38], these should be confirmed by multicenter prospective clinical trials. The final reports from two nationwide phase II trials (JCOG0607 and JCOG1009/1010) are expected to have conclusive outcomes [39, 40]. In addition to recurrence of and survival from the primary cancers, development of metachronous gastric cancers is an important issue, because the whole stomach is preserved after endoscopic resection. Although an RCT from Japan revealed H. pylori eradication after gastric endoscopic resection significantly reduced development of metachronous gastric cancers at the 3-year follow-up [41], it is still controversial whether H. pylori eradication would really reduce development of metachronous gastric cancers after gastric endoscopic resection from recent evidence [34, 42–44]. Further studies are necessary in this area, especially regarding appropriate prevention and surveillance of metachronous cancers.
As the future perspective, because the Japanese population is aging, we will treat more vulnerable patients such as elderly patients and patients with several comorbidities. In this scenario, we should seek more patient-friendly treatments for EGC, and more ESDs as a diagnostic measure would be performed to lessen overtreatment. Even after noncurative resection of ESD, such as slightly deeper submucosal invasion or ulcer findings with a larger tumor size, follow-up without additional gastrectomy would be permissible, considering the risks and benefits, when en bloc plus R0 resection is obtained.
In terms of secure en bloc plus R0 resection, laparoscopic and endoscopic cooperative surgery, including classic laparoscopic and endoscopic cooperative surgery [45] and nonexposed endoscopic wall-inversion surgery [46], is reported as an investigational step preceding endoscopic full-thickness resection. When laparoscopy is combined with ESD, lymph node dissection is also applicable [47]; this must be a better way to expand the indication of local resection for EGC with possible nodal metastasis.
In conclusion, this review of the recent literature showed that there is still room for improvement in endoscopic resection for EGC, and the related knowledge has slowly but steadily accumulated. We will keep pursuing more reliable, safer, and faster endoscopic resection and ESD for EGC.
References
National Cancer Center Japan. (Estimated cancer morbidity and mortality in 2015). 2015. http://www.ncc.go.jp/jp/information/press_release_20150428.html. Accessed 11 Aug 2016.
The Japanese Ministry of Health, Labour and Welfare. (Survey of medical care activities in public health insurance in 2015). 2016. http://www.e-stat.go.jp/SG1/estat/GL08020101.do?_toGL08020101_&tstatCode=000001029602. Accessed 11 Aug 2016.
Tatsumi K, Uedo N, Ishihara R, Yamamoto S, Yamamoto S, Masuda E, et al. A water-jet videoendoscope may reduce operation time of endoscopic submucosal dissection for early gastric cancer. Dig Dis Sci. 2012;57(8):2122–9.
Higuchi K, Tanabe S, Azuma M, Sasaki T, Katada C, Ishido K, et al. Double-endoscope endoscopic submucosal dissection for the treatment of early gastric cancer accompanied by an ulcer scar (with video). Gastrointest Endosc. 2013;78(2):266–73.
Takada J, Araki H, Onogi F, Nakanishi T, Kubota M, Ibuka T, et al. Safety and efficacy of carbon dioxide insufflation during gastric endoscopic submucosal dissection. World J Gastroenterol. 2015;21(26):8195–202.
Maeda Y, Hirasawa D, Fujita N, Obana T, Sugawara T, Ohira T, et al. A prospective, randomized, double-blind, controlled trial on the efficacy of carbon dioxide insufflation in gastric endoscopic submucosal dissection. Endoscopy. 2013;45(5):335–41.
Mori H, Kobara H, Fujihara S, Nishiyama N, Izuishi K, Ohkubo M, et al. Effectiveness of CO2-insufflated endoscopic submucosal dissection with the duodenal balloon occlusion method for early esophageal or gastric cancer: a randomized case control prospective study. BMC Gastroenterol. 2012;24(12):37.
Sumiyama K, Toyoizumi H, Ohya TR, Dobashi A, Hino S, Kobayashi M, et al. A double-blind, block-randomized, placebo-controlled trial to identify the chemical assistance effect of mesna submucosal injection for gastric endoscopic submucosal dissection. Gastrointest Endosc. 2014;79(5):756–64.
Kusano T, Etoh T, Akagi T, Ueda Y, Shiroshita H, Yasuda K, et al. Evaluation of 0.6 % sodium alginate as a submucosal injection material in endoscopic submucosal dissection for early gastric cancer. Dig Endosc. 2014;26(5):638–45.
Mori H, Kobara H, Rafiq K, Nishiyama N, Fujihara S, Oryu M, et al. Effects of gastric irrigation on bacterial counts before endoscopic submucosal dissection: a randomized case control prospective study. PLoS One. 2013;8(6):e65377.
Fujishiro M, Kaminishi M, Hiki N, Oda I, Fujisaki J, Uedo N, et al. Efficacy of spraying l-menthol solution during endoscopic treatment of early gastric cancer: a phase III, multicenter, randomized, double-blind, placebo-controlled study. J Gastroenterol. 2014;49(3):446–54.
Sasaki T, Tanabe S, Azuma M, Sato A, Naruke A, Ishido K, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012;44(6):584–9.
Gotoda T, Kusano C, Nonaka M, Fukuzawa M, Kono S, Suzuki S, et al. Non-anesthesiologist administrated propofol (NAAP) during endoscopic submucosal dissection for elderly patients with early gastric cancer. Gastric Cancer. 2014;17(4):686–91.
Murata A, Muramatsu K, Ichimiya Y, Kubo T, Fujino Y, Matsuda S. Endoscopic submucosal dissection for gastric cancer in elderly Japanese patients: an observational study of financial costs of treatment based on a national administrative database. J Dig Dis. 2014;15(2):62–70.
Yoshida M, Goto N, Kawaguchi M, Koyama H, Kuroda J, Kitahora T, et al. Initial clinical trial of a novel hemostat, TDM-621, in the endoscopic treatments of the gastric tumors. J Gastroenterol Hepatol. 2014;29(Suppl 4):77–9.
Tsuji Y, Fujishiro M, Kodashima S, Ono S, Niimi K, Mochizuki S, et al. Polyglycolic acid sheets and fibrin glue decrease the risk of bleeding after endoscopic submucosal dissection of gastric neoplasms (with video). Gastrointest Endosc. 2015;81(4):906–12.
Yoshida Y, Matsuda K, Tamai N, Yoshizawa K, Nikami T, Ishiguro H, et al. A pilot study using an infrared imaging system in prevention of post-endoscopic submucosal dissection ulcer bleeding. Gastric Cancer. 2014;17(1):116–21.
Mochizuki S, Uedo N, Oda I, Kaneko K, Yamamoto Y, Yamashina T, et al. Scheduled second-look endoscopy is not recommended after endoscopic submucosal dissection for gastric neoplasms (the SAFE trial): a multicentre prospective randomised controlled non-inferiority trial. Gut. 2015;64(3):397–405.
Hikichi T, Sato M, Watanabe K, Nakamura J, Takagi T, Suzuki R, et al. Oral rabeprazole administration on a procedure day suppresses bleeding after endoscopic submucosal dissection for gastric neoplasms. Fukushima J Med Sci. 2014;60(1):68–74.
Imaeda H, Hosoe N, Suzuki H, Saito Y, Ida Y, Nakamura R, et al. Effect of lansoprazole versus roxatidine on prevention of bleeding and promotion of ulcer healing after endoscopic submucosal dissection for superficial gastric neoplasia. J Gastroenterol. 2011;46(11):1267–72.
Tomita T, Kim Y, Yamasaki T, Okugawa T, Kondo T, Toyoshima F, et al. Prospective randomized controlled trial to compare the effects of omeprazole and famotidine in preventing delayed bleeding and promoting ulcer healing after endoscopic submucosal dissection. J Gastroenterol Hepatol. 2012;27(9):1441–6.
Arai M, Matsumura T, Okimoto K, Oyamada A, Saito K, Minemura S, et al. Two-week treatment with proton pump inhibitor is sufficient for healing post endoscopic submucosal dissection ulcers. World J Gastroenterol. 2014;20(43):16318–22.
Takayama M, Matsui S, Kawasaki M, Asakuma Y, Sakurai T, Kashida H, et al. Efficacy of treatment with rebamipide for endoscopic submucosal dissection-induced ulcers. World J Gastroenterol. 2013;19(34):5706–12.
Kobayashi M, Takeuchi M, Hashimoto S, Mizuno K, Sato Y, Narisawa R, et al. Contributing factors to gastric ulcer healing after endoscopic submucosal dissection including the promoting effect of rebamipide. Dig Dis Sci. 2012;57(1):119–26.
Nakamura M, Tahara T, Shiroeda H, Matsunaga K, Otsuka T, Yonemura J, et al. The effect of short-term proton pump inhibitor plus anti-ulcer drug on the healing of endoscopic submucosal dissection-derived artificial ulcer: a randomized controlled trial. Hepatogastroenterology. 2015;62(137):219–24.
Higuchi K, Takeuchi T, Uedo N, Takeuchi Y, Naito Y, Yagi N, et al. Efficacy and safety of 1-week Helicobacter pylori eradication therapy and 7-week rebamipide treatment after endoscopic submucosal dissection of early gastric cancer in comparison with 8-week PPI standard treatment: a randomized, controlled, prospective, multicenter study. Gastric Cancer. 2015;18(3):612–7.
Horikawa Y, Mimori N, Mizutamari H, Kato Y, Shimazu K, Sawaguchi M, et al. Proper muscle layer damage affects ulcer healing after gastric endoscopic submucosal dissection. Dig Endosc. 2015;27(7):747–53.
Watari J, Tomita T, Toyoshima F, Sakurai J, Kondo T, Asano H, et al. The incidence of “silent” free air and aspiration pneumonia detected by CT after gastric endoscopic submucosal dissection. Gastrointest Endosc. 2012;76(6):1116–23.
Mori H, Rafiq K, Kobara H, Fujihara S, Nishiyama N, Kobayashi M, et al. Local steroid injection into the artificial ulcer created by endoscopic submucosal dissection for gastric cancer: prevention of gastric deformity. Endoscopy. 2012;44(7):641–8.
Higuchi N, Nakamura K, Ihara E, Akahoshi K, Akiho H, Sumida Y, et al. Preserved gastric motility in patients with early gastric cancer after endoscopic submucosal dissection. J Gastroenterol Hepatol. 2013;28(3):494–8.
Ono S, Fujishiro M, Yoshida N, Doyama H, Kamoshida T, Hirai S, et al. Thienopyridine derivatives as risk factors for bleeding following high risk endoscopic treatments: Safe Treatment on Antiplatelets (STRAP) study. Endoscopy. 2015;47(7):632–7.
Hoteya S, Iizuka T, Kikuchi D, Mitani T, Matsui A, Ogawa O, et al. Secondary endoscopic submucosal dissection for residual or recurrent tumors after gastric endoscopic submucosal dissection. Gastric Cancer. 2014;17(4):697–702.
Tanabe S, Ishido K, Higuchi K, Sasaki T, Katada C, Azuma M, et al. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a retrospective comparison with conventional endoscopic resection in a single center. Gastric Cancer. 2014;17(1):130–6.
Kawanaka M, Watari J, Kamiya N, Yamasaki T, Kondo T, Toyoshima F, et al. Effects of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic treatment: analysis of molecular alterations by a randomised controlled trial. Br J Cancer. 2016;114(1):21–9.
Tsuji K, Yoshida N, Nakanishi H, Takemura K, Yamada S, Doyama H. Recent traction methods for endoscopic submucosal dissection. World J Gastroenterol. 2016;22(26):5917–26.
Oda I, Suzuki H, Nonaka S, Yoshinaga S. Complications of gastric endoscopic submucosal dissection. Dig Endosc. 2013;25(Suppl 1):71–8.
Gotoda T, Iwasaki M, Kusano C, Seewald S, Oda I. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg. 2010;97(6):868–71.
Okada K, Fujisaki J, Yoshida T, Ishikawa H, Suganuma T, Kasuga A, et al. Long-term outcomes of endoscopic submucosal dissection for undifferentiated-type early gastric cancer. Endoscopy. 2012;44(2):122–7.
Kurokawa Y, Hasuike N, Ono H, Boku N, Fukuda H. A phase II trial of endoscopic submucosal dissection for mucosal gastric cancer: Japan Clinical Oncology Group study JCOG0607. Jpn J Clin Oncol. 2009;39(7):464–6.
Takizawa K, Takashima A, Kimura A, Mizusawa J, Hasuike N, Ono H, et al. A phase II clinical trial of endoscopic submucosal dissection for early gastric cancer of undifferentiated type: Japan Clinical Oncology Group study JCOG1009/1010. Jpn J Clin Oncol. 2013;43(1):87–91.
Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008;372(9636):392–7.
Kato M, Nishida T, Yamamoto K, Hayashi S, Kitamura S, Yabuta T, et al. Scheduled endoscopic surveillance controls secondary cancer after curative endoscopic resection for early gastric cancer: a multicentre retrospective cohort study by Osaka University ESD Study Group. Gut. 2013;62(10):1425–32.
Maehata Y, Nakamura S, Fujisawa K, Esaki M, Moriyama T, Asano K, et al. Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc. 2012;75(1):39–46.
Mori G, Nakajima T, Asada K, Shimazu T, Yamamichi N, Maekita T, et al. Incidence of and risk factors for metachronous gastric cancer after endoscopic resection and successful Helicobacter pylori eradication: results of a large-scale, multicenter cohort study in Japan. Gastric Cancer. 2016;19(3):911–8.
Nunobe S, Hiki N, Gotoda T, Murao T, Haruma K, Matsumoto H, et al. Successful application of laparoscopic and endoscopic cooperative surgery (LECS) for a lateral-spreading mucosal gastric cancer. Gastric Cancer. 2012;15(3):338–42.
Niimi K, Aikou S, Kodashima S, Yagi K, Oya S, Yamaguchi D, et al. Video of the month: a novel endoscopic full-thickness resection for early gastric cancer. Am J Gastroenterol. 2015;110(11):1535.
Goto O, Takeuchi H, Kawakubo H, Sasaki M, Matsuda T, Matsuda S, et al. First case of non-exposed endoscopic wall-inversion surgery with sentinel node basin dissection for early gastric cancer. Gastric Cancer. 2015;18(2):434–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mitsuhiro Fujishiro declares that he has received lecture honorarium from Takeda Pharmaceutical, Esai, Zeria Pharmaceutical, and Nihon Pharmaceutical, and a collaborative fund from HOYA-Pentax as a chief investigator of the University of Tokyo. The other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fujishiro, M., Yoshida, S., Matsuda, R. et al. Updated evidence on endoscopic resection of early gastric cancer from Japan. Gastric Cancer 20 (Suppl 1), 39–44 (2017). https://doi.org/10.1007/s10120-016-0647-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0647-8