Abstract
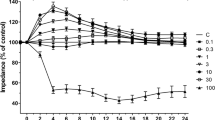
Hemorrhagic transformation is a major complication associated with tissue plasminogen activator (tPA) therapy for ischemic stroke. We studied the effect of tPA on the blood–brain barrier (BBB) function with our in vitro monolayer model generated using rat brain microvascular endothelial cells subjected either to normoxia or to hypoxia/reoxygenation (H/R) with or without the administration of tPA. The barrier function was evaluated by the transendothelial electrical resistance (TEER), the permeability of sodium fluorescein and Evans’ blue-albumin (EBA), and the uptake of lucifer yellow (LY). The permeability of sodium fluorescein and EBA was used as an index of paracellular and transcellular transport, respectively. The administration of tPA increased the permeability of EBA and the uptake of LY under normoxia. It enhanced the increase in the permeability of both sodium fluorescein and EBA, the decrease in the TEER, and the disruption in the expression of ZO-1 under H/R conditions. Administration of tPA could cause an increase in the transcellular transport under normoxia, and both the transcellular and paracellular transport of the BBB under H/R conditions in vitro. Even in humans, tPA may lead to an opening of the BBB under non-ischemic conditions and have an additional effect on the ischemia-induced BBB disruption.






Similar content being viewed by others
References
Benchenane K, Berezowski V, Fernandez-Monreal M, Brillault J, Valable S, Dehouck MP et al (2005) Oxygen glucose deprivation switches the transport of tPA across the blood-brain barrier from an LRP-dependent to an increased LRP-independent process. Stroke 36:1065–1070. doi:10.1161/01.STR.0000163050.39122.4f
Cheng T, Petraglia AL, Li Z, Thiyagarajan M, Zhong Z, Wu Z et al (2006) Activated protein C inhibits tissue plasminogen activator-induced brain hemorrhage. Nat Med 12:1278–1285. doi:10.1038/nm1498
Deli MA, Szabó CA, Dung NTK, Joó F (1997) Immunohistochemical and electron microscopy detections on primary cultures of rat cerebral endothelial cells. In: Boer AG, Sutanto W (eds) Drug transport across the blood–brain barrier: in vivo and in vitro techniques. Harwood Academic Publishers, Amsterdam, pp 23–28
Deli MA, Ábrahám CS, Takahata H, Niwa M (2001) Tissue plasminogen activator inhibits P-glycoprotein activity in brain endothelial cells. Eur J Pharmacol 411:R3–R5. doi:10.1016/S0014-2999(00)00895-5
Dohgu S, Nishioku T, Sumi N, Takata F, Nakagawa S, Naito M et al (2007) Adverse effect of cyclosporin A on barrier functions of cerebral microvascular endothelial cells after hypoxia-reoxygenation damage in vitro. Cell Mol Neurobiol 27:889–899. doi:10.1007/s10571-007-9209-2
Fischer S, Wiesnet M, Marti HH, Renz D, Schaper W (2004) Simultaneous activation of several second messengers in hypoxia-induced hyperpermeability of brain derived endothelial cells. J Cell Physiol 198:359–369. doi:10.1002/jcp. 10417
Godfrey KR, Tanswell P, Bates RA, Chappell MJ, Madden FN (1998) Nonlinear pharmacokinetics of tissue-type plasminogen activator in three animal species: a comparison of mathematical models. Biopharm Drug Dispos 19:131–140. doi:10.1002/(SICI)1099-081X(199803)19:2<131::AID-BDD87>3.0.CO;2-L
Hayashi K, Nakao S, Nakaoke R, Nakagawa S, Kitagawa N, Niwa M (2004) Effects of hypoxia on endothelial/pericytic co-culture model of the blood-brain barrier. Regul Pept 123:77–83. doi:10.1016/j.regpep.2004.05.023
Hoheisel D, Nitz T, Franke H, Wegener J, Hakvoort A, Tilling T et al (1998) Hydrocortisone reinforces the blood–brain barrier properties in a serum free cell culture system. Biochem Biophys Res Commun 244:312–316. doi:10.1006/bbrc.1997.8051
Honda M, Nakagawa S, Hayashi K, Kitagawa N, Tsutsumi K, Nagata I et al (2006) Adrenomedullin improves the blood–brain barrier function through the expression of claudin-5. Cell Mol Neurobiol 26:109–118. doi:10.1007/s10571-006-9028-x
Kis B, Deli MA, Kobayashi H, Abraham CS, Yanagita T, Kaiya H et al (2001) Adrenomedullin regulates blood–brain barrier functions in vitro. NeuroReport 12:4139–4142. doi:10.1097/00001756-200112210-00055
Koto T, Takubo K, Ishida S, Shinoda H, Inoue M, Tsubota K et al (2007) Hypoxia disrupts the barrier function of neural blood vessels through changes in the expression of claudin-5 in endothelial cells. Am J Pathol 170:1389–1397. doi:10.2353/ajpath.2007.060693
Liu D, Cheng T, Guo H, Fernandez JA, Griffin JH, Song X et al (2004) Tissue plasminogen activator neurovascular toxicity is controlled by activated protein C. Nat Med 10:1379–1383. doi:10.1038/nm1122
Mark KS, Davis TP (2002) Cerebral microvascular changes in permeability and tight junctions induced by hypoxia-reoxygenation. Am J Physiol Heart Circ Physiol 282:H1485–H1494
Nakagawa S, Deli MA, Nakao S, Honda M, Hayashi K, Nakaoke R et al (2007) Pericytes from brain microvessels strengthen the barrier integrity in primary cultures of rat brain endothelial cells. Cell Mol Neurobiol 27:687–694. doi:10.1007/s10571-007-9195-4
NINDS (1995) Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 333:1581–1587. doi:10.1056/NEJM199512143332401
NINDS (1997) Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA Stroke Study Group. Stroke 28:2109–2118
Nishioku T, Takata F, Yamauchi A, Sumi N, Yamamoto I, Fujino A et al (2007) Protective action of indapamide, a thiazide-like diuretic, on ischemia-induced injury and barrier dysfunction in mouse brain microvascular endothelial cells. J Pharmacol Sci 103:323–327. doi:10.1254/jphs.SC0060222
Niwa K, Kado T, Sakai J, Karino T (2004) The effects of a shear flow on the uptake of LDL and acetylated LDL by an EC monoculture and an EC-SMC coculture. Ann Biomed Eng 32:537–543. doi:10.1023/B:ABME.0000019173.79939.54
Perriere N, Demeuse P, Garcia E, Regina A, Debray M, Andreux JP et al (2005) Puromycin-based purification of rat brain capillary endothelial cell cultures. Effect on the expression of blood-brain barrier-specific properties. J Neurochem 93:279–289. doi:10.1111/j.1471-4159.2004.03020.x
Utepbergenov DI, Mertsch K, Sporbert A, Tenz K, Paul M, Haseloff RF et al (1998) Nitric oxide protects blood-brain barrier in vitro from hypoxia/reoxygenation-mediated injury. FEBS Lett 424:197–201. doi:10.1016/S0014-5793(98)00173-2
Vassalli JD, Sappino AP, Belin D (1991) The plasminogen activator/plasmin system. J Clin Invest 88:1067–1072. doi:10.1172/JCI115405
Wang S, Lee SR, Guo SZ, Kim WJ, Montaner J, Wang X et al (2006) Reduction of tissue plasminogen activator-induced matrix metalloproteinase-9 by simvastatin in astrocytes. Stroke 37:1910–1912. doi:10.1161/01.STR.0000226923.48905.39
Yepes M, Sandkvist M, Moore EG, Bugge TH, Strickland DK, Lawrence DA (2003) Tissue-type plasminogen activator induces opening of the blood-brain barrier via the LDL receptor-related protein. J Clin Invest 112:1533–1540
Youdim KA, Avdeef A, Abbott NJ (2003) In vitro trans-monolayer permeability calculations: often forgotten assumptions. Drug Discov Today 8:997–1003. doi:10.1016/S1359-6446(03)02873-3
Acknowledgments
tPA was obtained as a generous gift from Kyowa Hakko Kogyo Co, Japan. We wish to thank Yoshisada Shibata, Maria A. Deli, Kunihiko Tanaka, Yasuko Yamashita, Yoshihiro Takaya, Shoji Horai, Yoichi Morofuji, Takanori Shimono, and Makiko Yamaguchi for their critical reviews of the manuscript and outstanding professional guidance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hiu, T., Nakagawa, S., Hayashi, K. et al. Tissue Plasminogen Activator Enhances the Hypoxia/reoxygenation-induced Impairment of the Blood–brain Barrier in a Primary Culture of Rat Brain Endothelial Cells. Cell Mol Neurobiol 28, 1139–1146 (2008). https://doi.org/10.1007/s10571-008-9294-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-008-9294-x