Abstract
Social workers are called to respond to disasters to provide assessment, crisis counseling and trauma treatment as part of the recovery effort. While research has identified the types of interventions appropriate in assisting trauma survivors, little empirical research exists to help address the distress responses that social workers experience when exposed to the trauma material of disaster survivors and their families. Case examples can inform social work practice using evidence informed interventions and recording the outcomes. This article presents three case histories of social workers responding to disasters, the course of their secondary traumatic stress responses and their struggle to overcome the psychological adversity they faced.
Similar content being viewed by others
Introduction
Disasters that overwhelm the response capacity of the affected communities occur an average of 100 times annually across the United States (CMHS, 2001). Over the past 15 years large scale disasters such as earthquakes, floods, tornados, school shootings, cluster suicides and terrorist attacks have increased awareness of the psychological effects of traumatic events (Norris, Friedman & Watson, 2002; Hamblen, Watson, Norris, & Pfefferbaum, 2005; Norris et al., 2006). The 9/11/01 terrorist attacks affected the psyche of the United States causing anxiety and changing the perception of safety throughout the country (Galea et al., 2002; Schuster et al., 2001). The most devastating hurricane in US history hit the Gulf Coast in 2005 and subsequent flooding stranded thousands who were left crying for help (Weisler, Barbee, & Townsend, 2006). These events and their aftermath caused extreme emotional pain for survivors. Many lost loved ones, homes and entire communities changing their perception of social support. This is one of the primary indicators of the course of psychological recovery post disaster (Norris & Kaniasty, 1996; Weisler, Barbee, & Townsend, 2006).
Mental health services are an integral component of each of the states ‘All Hazards Plans’ as well as the National Incident Management System (CMHS, 2003; FEMA, 2006). While the funding for the mental health component of national disaster response efforts is only approximately 1% of the overall budget, the grant awards for disaster crisis counseling over the last 5 years have exceeded the totals provided to states during the previous 30 years cumulatively (SAMHSA, 2006). This is an indication of the increased recognition of the need to attend to the psychological affects of disasters, both natural and man-made.
Social Workers Respond
Less recognized are the damaging effects of secondary traumatic stress experienced by the mental health response staffs who are called to action in disaster mental health recovery efforts (Bride, 2007; Figley, 2002). Depending on the size and scope of the event, disaster mental health services may be continued beyond the immediate response phase and social workers are often a large segment of those staffs engaged in the continuing psychological response effort (CMHS, 2001). This was the case in the 9/11/01 terrorist attacks in New York City where approximately 50% of the staffs providing crisis counseling were social workers (NYSOMH, 2005). Alabama Department of Public Health officials estimate that 75% of their disaster mental health staffs in the 2005 Hurricane response were social workers (Knight & West, 2007). The Louisiana Hurricane Katrina state mental health disaster response program administrators report that at least 30% of their crisis counselors are social workers (Cook, 2007) and in Mississippi at least 25% of staffs working in the state’s Hurricane Katrina Project Recovery program were social workers (Hillman, 2007).
These staffs attend to survivors performing various roles including monitoring and assessment, crisis counseling, connecting survivors with loved ones, setting up shelters, providing case management and more. While many of these services fall within the purview of typical social work activities, delivering them in the highly intensely emotional post disaster environment creates an unusual set of circumstances. Working under these extreme conditions may contribute to an increased risk of developing secondary traumatic stress in these workers (Figley, 1999; Meyers & Wee, 2005; Young, Ford, Ruzek, Friedman, & Guzman, 1998).
Compassion Fatigue/Secondary Traumatic Stress
Compassion Fatigue (CF) is defined as the experience of posttraumatic stress symptoms in trauma counselors as a result of listening to the trauma material of clients or exposure to a client or a loved one’s trauma (Figley, 1995, 1999; Kassam-Adams, 1999; Stamm, 1995, 1999). Figley (1994, 1995, 1999) and Stamm (1999) pioneered the field of Compassion Fatigue and increased awareness that staffs who work in traumatizing settings are at risk for emotional suffering as a result. Figley (1999) indicates that the term compassion fatigue can be used interchangeably with secondary traumatic stress. Additionally, Stamm (1999) notes that compassion fatigue and secondary traumatic stress are most alike in meaning. To maintain consistency in the terminology used for the empirically validated constructs of acute and posttraumatic stress disorder (AMA, 2000) the term secondary traumatic stress will be utilized understanding that it is interchangeable with compassion fatigue.
McCann and Pearlman (1990) have introduced and researched (Pearlman & MacIan, 1995) Vicarious Trauma (VT) utilizing a definition that closely associates it with compassion fatigue. They have identified key areas where trauma counselors may experience shifts in their cognitive and emotional states such as their sense of meaning, personal safety, spiritual beliefs and trust (Pearlman, 1999).
The disaster environment may include difficult emotional conditions, exposure to gruesome sites, sickening odors, danger, destruction of physical surroundings and social order breakdown (Meyers & Wee, 2005; Young et al., 1998). Temperature and/or weather extremes, lack of sanitary facilities, unstable travel or walking grounds, deep water, mud, debris or shifting objects create physically stressful working environments (Meyers & Wee, 2005; Young et al., 1998). The workload is often further pressured with the need for staffs to work long hours without breaks adding the individual stressors of fatigue and hunger as contributing variables to the risk of STS. Yet, the concern for the development of STS in the social workers responding to the extraordinary conditions of disaster work is only recently gaining the attention of administrators, managers and researchers (Bride, 2007; Catherall, 1999; Figley, 2002).
Models of Intervention
The current post crisis models of intervention for response staffs are limited and research on their effectiveness is just recently increasing (Meyers & Wee, 2005). Operational Debriefing developed by and for military personnel focuses on the functional aspects of a mission’s outcome from a factual perspective. The goals include identifying areas for improvement, planning and documentation of historical records (VA, 2007). Psychological Debriefing also originated in the military where soldiers shared stories as a method of increasing group cohesion and morale. Psychiatrists screened for ‘battle fatigue’ (Litz & Grey, 2002).
Police, fire, medical and other emergency services personnel used the military models of debriefing until Mitchell and Resnik (1981) introduced and trained extensively across the country in Critical Incident Stress Debriefing (CISD). CISD addresses the emotional status of emergency response personnel in post crisis situations in a group processing exercise that is accompanied by education regarding the normal responses to stressful situations and referrals for follow up services as appropriate. The model includes recommendations for self care such as monitoring one’s physiology during the immediate post vention period. The acceptability and popularity of the model has apparently been due to the focus on stress concerns rather than the stigmatizing reference to potential mental health problems (Everly & Mitchell, 1999). Despite strong controversy over variations in the use of CISD as well as a review by Rose, Bisson, and Weseley (2001) that suggests a potential risk of harm, the model remains in extensive use throughout the crisis response industry. It may have value as an educational and supportive rather than a treatment model and has been noted to facilitate more adaptive coping (Litz & Grey, 2002).
The lack of sufficient evidence based research should not prevent the field from evaluating the studies that do exist. Recommendations that may correspond to the activities that suit the needs of staff in the field and fit with their abilities to implement them as preventative or response measures should be considered (Catherall, 1999; Munroe, 1999; Young, Ruzek, Wong, Salzer, & Naturale, 2006). Catherall (1999) and Munroe (1999) discuss how administrators and managers are responsible to warn staffs of their risk for developing STS and emphasize preventative measures such as peer support and structured supervision. Figley (1999) has also recommended these professional supports for staffs working with trauma clients. Figley (1999) and Stamm (1999) and Stamm, Bieber, and Pearlman (1991) have suggested the use of their self-assessment tools to help individuals identify and more readily recognize STS symptoms. Pearlman (1990, 1999) and Pearlman and MacIan (1995) recommend several techniques that may assist in mitigating the development of VT by addressing the individual’s spiritual, physical and emotional needs. Young et al., (2006), Ruzek (2006), Wee and Meyers (2002) and Young et al. (1998) offer comprehensive and valuable recommendations specifically for disaster response staffs.
Stress management exercises are included in disaster training curriculum to help relieve STS and avoid further development of various types of stress responses (CMHS, 2003; Young et al., 2006). These interventions should also be guided by what services are available and accessible in the environment and the time frames within which services are delivered (Jackson & Cook, 1999). The use of these and other secondary traumatic stress interventions, though, has not been sufficiently researched in the population of social workers responding to disasters (Bride, 2007; Meyers & Wee, 2005). This brings us to examining case studies as a way of learning about the occurrence of secondary traumatic stress and looking at how clinicians use their assessment skills, access the current knowledge base and develop interventions for post crisis care based on the immediate needs of the responders in each specific disaster situation. Case examples may provide an informed approach to researching secondary traumatic stress interventions and their outcomes in the future.
Case Studies
The following are three case studies of disaster social workers who suffered with STS responses in the midst of their fieldwork. In each of these cases, a combination of some or all of the following components of secondary traumatic stress interventions were utilized:
-
(a) Caisis counseling-In the disaster field, this term is generally used when referring to the model that incorporates: active listening of survivors disaster experience; validation of survivors expressed reactions and feelings; normalization of the natural reactions to an abnormal event; informing survivors (without minimizing their experience) that others who have gone through similar experiences often have similar responses in an effort to destigmatize the survivor’s reactions and decrease their fear of developing a serious mental illness; psychoeducation regarding the most common physical, cognitive, behavioral and emotional responses to stressful events; coping skills enhancement-drawing on current or previously utilized strengths and introduction of new coping mechanisms when survivors lack them; resource and referral linkages-connecting survivors with family, friends, group support, case management, financial assistance and other agencies and organizations providing disaster assistance where appropriate; immediate planning and focus on continued recovery as well as hope for the future.
-
(b) Psychoeducation regarding identification, symptoms, preventive measures and treatment for secondary traumatic stress as well as the risk around its development is important for staffs (Figley, 1999). This is a therapeutic technique that has an evidence base in its use with varying populations in a collaborative, strengths based approach (Lukens & McFarlane, 2004).
-
(c) Voluntary individual and/or group narrative exercises-The goal of a narrative is to seek factual information about the individual’s experience, thoughts, questions or specific problems and to identify the problem causing the distress (i.e., the trauma), then to look at how the symptoms are effecting the person’s life and how the problem might be addressed (White & Epston, 1990). In the group setting, sharing similar experiences serves to decrease a sense of isolation and enhance social support.
-
(d) Stress management education and training-These techniques include a wide range of physical and cognitive exercises from the relaxation response (Selye, 1976) to cognitive restructuring as well as pleasurable activity planning and implementation (Hamblen et al., 2003).
-
(e) Self assessment is a useful tool in address secondary traumatic stress as many staffs do not recognize when they are having difficulty. A formal, scientific tool may be an acceptable source of information in professionals who intellectualize emotional issues. The ProQOL-IV (Stamm, 2006) is a reliable and valid tool that is easily self administered in a short period of time and allows full confidentiality in completing and scoring the tool.
-
(f) Self care recommendations and strategies involve physical, spiritual and social areas of one’s lifestyle that need to be maintained during and after disaster work. Examples of these include maintaining a healthy diet; physical exercise, balancing work and play, rest, self awareness, spiritual replenishment and maintaining networks of friends and family (Pearlman, 1999). Disaster specific professional and organizational supports that are believed to assist in the mitigation of the development of STS include supervision, peer support, debriefings, consultation, communication, recognition of staffs, closure and follow up activities (CMHS, 2001; Meyers & Wee, 2002; Norris et al., 2006; Young et al., 1998).
-
(g) Post deployment education and instruction address the practical issues and expectations that staff may have in the physical and emotional realms once their disaster assignment is complete. These may include addressing concerns of family members, reentering the workplace, establishing normalcy and learning from their experiences in the field.
-
(h) Evaluation-As with any intervention, giving participants an opportunity to provide feedback as to the outcome of the activity is important. Standard satisfaction questionnaires may be useful as well as open-ended questions that allow for qualitative data to be gathered and analyzed.
Individual engagement strategies, stress management techniques and self-care activities varied where cultural assessment determined their appropriateness.
A Large Scale Man Made Disaster: The Case of Peg. O
Peg O. was 23-year-old bachelor’s level social worker who had been employed for just a few months in her first job when the 9/11/01 terrorist attack on the World Trade Center in New York City occurred. Peg volunteered to work as a representative of her agency at Pier 90 where services were being offered to family members and survivors. The environment at the Pier was an intense and complex mix of physical and emotional sensory stimulation. Most disaster service delivery agencies set up booth-type structures without front or top enclosures. This resulted in a high noise level and in most instances, little or no privacy.
Along the right side of the Pier, there was a temporary, solid wall that surrounded the city’s incident command center, a few small meeting areas and the lavatories. All along this wall, pictures, notes, flowers, poems, letters, artwork and plea’s to help finding missing loved ones were posted. There was not an area on or near the wall that didn’t attract one’s attention as you walked by, expressing the pain and grief of family members, friends and co-workers.
Peg reported being overwhelmed at times by the intense emotions that she was exposed to at this work place. She described walking by a booth one day and observing a family member frantically digging through a large paper bag, then collapsing onto a folding chair in obvious distress crying, “I don’t have it. I can’t find it.” Peg indicated she had all to do to stop herself from intruding upon the scene and looking for the required papers herself.
Peg complained about the poor operations structure at the Pier indicating that the information dissemination and application processes should be streamlined making it easier for emotionally distraught survivors and their families to obtain services. When the Pier closed, Peg decided to work on policy issues related to service delivery. She began working with one of the operations managers, plotting out where disaster services could be realistically implemented for the population she was assigned to address. Peg continued to see several groups of survivors and followed their progress as she visited provider agencies throughout the city.
At the 6-month point, Peg came to an individual supervision session in a panic. She reported having to quit the job saying she was very stressed and was beginning to have returning symptoms from a panic disorder that she had suffered with a few years earlier. The supervisor invited her to calm herself and talk about what was happening. Peg provided the history of her previous episode with panic during college. Her current symptoms of a pounding heart, rapid breathing, excessive sweating and then exhaustion began to reoccur almost every morning before work for the past 2 months. She stated, “Now that you know about this, for sure I’ll have to quit.” The manager replied that it would be her preference that Peg remain in the job and asked if she would be willing to work on a plan that would allow her to continue working and gain symptom control. Peg was quite relieved that the manager wanted her to stay and immediately offered that she would seek a local therapist. “A necessary first step,” the manager agreed, “and we can do more in the way of supporting you here on the job as well.”
The manager arranged for Peg to begin to work closely with a supervisor who was more available so that individual weekly meetings could occur. Peg was instructed to prepare a structured agenda including a review of at least one job task that would require assistance to complete, one difficult ‘case’ or issue that the division was struggling with and one issue that seemed to touch her emotionally. The agenda was designed to address the pressure that helpers often put on themselves thinking they have to do everything themselves (Norris, et al., 2006). It also eliminated her ‘asking for help’ by having to list a problem issue on each agenda. Discussing one issue that touched her emotionally gave the supervisor opportunity to review psychoeducational information and normalize emotional responses to disaster work.
The supervisor provided secondary traumatic stress education as part of their meetings. Peg was reminded that people who have previously experienced a mental disorder or trauma are at higher risk for developing STS especially when exposed the stories of disaster survivors. The supervisor discussed coping skills with Peg and they explored what worked best in the past. She also suggested Peg explore information about cognitive behavioral treatment for exposure to trauma as supported in the research literature (Bryant, Harvey, Dang, Sackville & Basten, 1998).
Peg’s expression of symptoms also brought to light the problem that her division was separated from the larger group activities resulting in that division having the least management support. Peg verbalized that this separation eliminated peer support and left her division feeling less important and less supported in general.
The manager worried that other staff members may also be distressed and arranged for all the staffs to attend stress management in-services that were being offered by the project’s administration. Weekly ‘all staff” meetings were scheduled at a time when Peg’s entire division could attend allowing for increased communications and peer interaction. Additionally, Peg’s supervisor suggested that she complete a self-assessment on a monthly basis to help her monitor her stress more closely.
Within 3 weeks of individual supervision addressing STS, attendance at a stress management in-service and inclusion in the ‘all staff’ meetings, Peg reported that her nightmares had disappeared and that her panic attacks were less frequent. She indicated that being able to connect more with staffs and exchange ideas allowed her to learn and grow on a professional level. It also established a ‘cushion’ of support that helped her feel less overwhelmed and isolated. She added that receiving positive feedback from peers about her contributions to the effort helped boost her confidence and self-concept. Over several months, Peg needed individual therapy with less frequency. In this case, Peg’s pre-existing condition was treated separately and the secondary traumatic stress interventions were applied in the work setting. The supervisor reinforced psychoeducation, coping techniques and self-care interventions. She assured that Peg was provided with information about her disaster related STS symptoms in addition to the treatment of her panic disorder. As importantly, the manager recognized that there were structural supports in the agency that could help support Peg and the rest of the staffs to avoid any further development or worsening of STS responses.
A Natural Disaster of Large Scale and Scope: The Case of Patty C.
Patty C. is a 32-year-old licensed clinical social worker who has been providing outpatient services in a local clinic for the past 8 years since receiving her MSW. Like many therapists across the country, Patty volunteered to join the disaster mental health response effort after the Gulf Coast Hurricanes. She was deployed 3 months after the storm when the recovery effort was slow and the severe devastation of the storms remained highly evident.
Patty would oversee a staff of eight mental health professionals assigned to various Disaster Recovery Centers (DRC’s) along the coast. She drove through each of the devastated towns to familiarize herself with the staff’s coverage points and stopped to observe what was left of the destroyed communities. In some towns, she observed people cleaning up debris and standing over slabs of concrete or pavement that she realized must have once been the foundation of a home or a driveway. In one town, a church had survived and there was a hub of people accepting meals and clothing that were being distributed. But in general Patty noted that most of the land was flattened for miles with no signs of surviving homes.
Patty began to experience an anxiety that increased over the next couple of days and found she could not eat or sleep very well as she was obsessing about the people she had seen. One day Patty attended a community meeting and found herself yelling that more has to be done to help the survivors. She stormed out of the meeting and drove up and down the coast for hours. At the end of the week, Patty reported to the oversight manager that she was having difficulty sleeping but otherwise stated she was fine. By the next morning, though, she appeared to be in a hyper manic state pacing and talking aloud constantly to herself. One of the team members aware of Patty’s increasing distress called the managing supervisor who arranged for a back up team leader, Anne, to come in the next day.
Anne found Patty looking very tired and stressed. She was clearly distracted, unable to focus on conversation or any task for more than a few minutes. Anne discussed her concern about Patty’s lack of sleep and inquired about any prior physical or emotional problems. Patty easily reported no prior health or mental health problems, but stated she was in therapy to discuss family relational issues. She was not taking any medication and had a recent physical reporting no problems. Anne suggested that Patty turn over her team leader responsibilities and attempt to get some rest, sleep and nourishment. She introduced some breathing and stretching exercises and Patty was very receptive. She admitted to Anne that she was relieved to be free of her team leader responsibilities, which she stated she had been unprepared for.
At evening report, Patty participated in a group debriefing that Anne conducted. They reviewed the post deployment guidelines and psychoeducational information about direct and secondary traumatic stress responses in the disaster environment. Patty recognized her symptoms and asked, “That’s me, isn’t it? Not sleeping, not eating, stomach trouble, anxious.” She proceeded to tell Anne how she felt completely overwhelmed by the disaster environment and the psychic pain of the survivors. She was angry at the lack of progress in the recovery process and unable to focus on her duties. Anne listened, validated and normalized her responses. They worked on an intervention plan that included breathing exercises, yoga (which Patty indicated she usually engaged in at home every day, but had not done so since arriving) and walking. They discussed the need for Patty to plan eating a few small meals during the day and taking a stomach aide as well as drinking plenty of water and some calming tea. Patty admitted to the possibility that she was dehydrated. Anne introduced the idea that Patty should go home the next day, follow up with her physician and therapist and continue a regimen of rest, exercise and healthful eating.
That night, Patty was able to sleep for quite a few hours and seemed calmer by the next morning. She participating in a stretching exercise and walked with several team members after breakfast. Arrangements were made for Patty to return home but she resisted the idea. She insisted that she was not going to leave until there was more help. She needed to be reassured that help would continue to be available in the region. Anne stressed that Patty needed to continue to rest and prepare to return home. During that evening’s debriefing, Patty cried as she told the team she had to leave. Anne offered appreciation for Patty’s contribution to the disaster effort. Other team members chimed in giving her positive feedback about being welcoming and helping them get to their fieldwork. Patty needed continuous gentle guidance to finish packing and reiteration of the positive feedback from the team. Anne confirmed that Patty’s husband would meet her at the airport.
A follow up call informed Anne that Patty had kept her physician appointment and reported slightly elevated blood pressure. She recognized with the help of her therapist that she needed to continue to exercise and maintain a healthy eating routine. In the next follow up call, Patty informed Anne that she was feeling her old self again. She verbalized that she wished she could go back into the field but recognized she should not do so. A few months later, Patty sent Anne a local newspaper article in which she was interviewed about the lack of progress in the Katrina response effort. Patty stated that while it wasn’t the New York Times, she felt pleased she had brought some media attention to the needs of the disaster survivors.
Mass Violence: A School Shooting at a Southwesterntown
Mass violence incidents involving the death of only one child can have a large-scale community effect (Cohen et al., 2005). In this case, the community responded to the shooting death of several high school students by a fellow student by immediately coming together to support the students and each other in the early aftermath. The parents who lost children had meetings in each other’s homes where their loved ones’ classmates were invited to console each other and receive attention from the adults.
School faculty and concerned parents developed a plan to line the sidewalks across the entire front of the school on the morning the students’ reentry was scheduled. They welcomed the students with open arms and joined them in the auditorium for a breakfast and an assembly meeting. There the principal discussed how important it was for the students to continue their studies and their lives, while still honoring the memory of their friends. With hugs and tears, parents said goodbye and classes resumed.
Three months later, the social work agency charged with counseling students in the school regarding the shooting, scheduled a meeting with an STS consultant. Despite initial resistance, the social workers described the details of their work and discussion ensued as to how the work was becoming more difficult. They were concerned about students who were traumatized by direct exposure to the shooting, as they seemed to be isolating from many of their classmates who were not directly involved.
The staffs indicated that this separation was causing a rift in the entire community as the two groups were beginning to disagree on every issue that came up in relation to the incident. For example, there was growing hostility about how to proceed with the graduating class activities and in what manner the lost students would be memorialized. Discussions had stopped and it was getting nearer to graduation with no celebration or memorial plans in the works. Staffs, too, had begun to separate, taking sides on these issues and arguing daily. The STS consultant observed that the staffs seemed to be over identifying with the groups they allied themselves with and were unable to assist in resolving arguments. They missed opportunities to enhance the groups’ coping skills and encourage the natural resiliency of the community.
The consultant validated the severity of the incident and the staff’s concerns. She provided opportunity for an expanded group narrative by asking pointed questions focusing on factual information regarding the recovery process to date. When the workers moved off point, she gently guided them back to discussing the chronology of their interventions and community responses. She noted that discussions seemed to stop after the parents requested a memorial in the center of town. In that same time frame, the trial of the young man who perpetrated the shootings was scheduled.
The social workers reported that they had provided grief counseling to parents who lost a loved one and traditional therapy to the most severely affected students. They were beginning to identify those that would require long-term treatment. There was no report of the provision of crisis counseling to the entire school. Nor was there any report of outreach to the general community providing psychoeducational information, which would assist in normalizing distress responses to the incident. The STS consultant decided to provide the staffs with a basic overview of common distress responses in mass violence situations and normalized the increase in tension, stress and even the occurrence of social structure breaks. She expanded her discussion to the issue of secondary traumatic stress and gave examples of what she had observed following other mass violence situations when staffs were overwhelmed and stressed. Afterwards, the workers were quiet for some time until one of them said, “We have something to learn here, don’t we.”
The consultant suggested that staff spend some time planning how to continue the good work that they had begun. They agreed to attend a meeting scheduled later in the week between school personnel and concerned parents. After several hours, the consultant suggested they break for a walk and something to eat. The staff suddenly realized that they had not taken their meal breaks together since the incident. Many noted that they had abruptly ended their exercise routines at home and few had engaged in any pleasurable activities that they could easily recall. After the break, the consultant guided the staff through a stress management breathing exercise. Then she conducted a self-care scheduling intervention urging staff to list their three favorite leisure activities and block out the time in their schedules when (within the week) they would next plan to participate in them.
After the STS interventions that day, the social workers seemed more enthusiastic and empowered as they declared that now they knew how to move forward. It had become clear that working only with those directly affected and providing traditional therapy was just one part of the intervention needed. They planned to provide psychoeducation for all of the students, families and other community members. One of the modalities for doing this included distributing informational handouts that provided normalization of distress responses and ways to enhance coping skills. They brainstormed looking for suggestions as to how to help the community reconnect by engaging in activities and rituals that would also show sensitivity for the continuing grieving process. Their first and toughest task was how to give the graduating class permission to celebrate in the midst of tragedy.
Over the next month, the social workers conducted education and support meetings with various groups of students, parents and community members using a narrative process, coping skills enhancement techniques and resiliency building activities. Staffs who worked with the parents of the children who had died facilitated discussion between them and the parents of the child they once referred to as ‘the shooter,’ but now called him by name. At the time of his criminal proceedings, they advocated for him to receive mental health treatment and not be tried as an adult. Their healing process was no longer at a standstill. Although the pain of their losses would always be with them, they were intent on creating a healthy and joyful community for the children who remained with them.
Conclusion
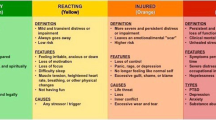
Case studies remain a valuable tool for understanding human behavior that enriches our field of practice. This is especially true in the study of the psychological aftermath of disasters, where there is a significant lack of evidence-based research. Social workers responding to disasters need to be aware of their risk of experiencing the same types of symptoms suffered by their traumatized clients (Munroe, 1999). Distress effects such as sleeplessness, nightmares, stomachaches, headaches, fatigue, memory loss, irritability and sadness are a few of the examples from the physical, cognitive, emotional and behavioral realms of the experience of secondary traumatic stress.
In each of these three cases, social workers experienced symptoms of secondary traumatic stress that effected both their personal and professional functioning. Peg experienced the reoccurrence of a previous mental health problem that required professional treatment. In the workplace, supervision and organizational supports were provided to decrease the stress that had triggered her symptoms. These interventions also helped to mitigate potential STS in staffs working with Peg under the strain of disaster circumstances.
Patty was unprepared for the devastation she was exposed to and experienced an inability to perform her duties due to her distress. Of note were her sleep problems that likely resulted in more serious cognitive and emotional symptoms. Once Patty was relieved of her disaster assignment, received structured support and implemented self-care activities, she was able to recover fairly quickly. While many STS responses may not appear so rapidly or intensely, disaster circumstances may create the opportunity for this to occur. Figley (1999) makes a differentiation between STS and VT indicating that STS can occur even after exposure to only one incident.
Human caused trauma can make it difficult for those exposed to make meaning of the event (Pearlman, 1990). Our last group of social workers who were overidentifying with the community members they were assigned to assist, failed to recognize their own distress. In this case, it appeared that the staffs also required education regarding traumatic incident responses and the types of non-traditional interventions necessary to assist in the recovery effort. This information increased their skills as well as their confidence and effectiveness.
The need for research in disaster mental health response work has been emphasized over the past decade although there is still recognition that the disaster environment creates difficulties in conducting such work (Norris et al., 2006; North & Pfefferbaum, 2002). Disaster circumstances do not allow for random controlled trials and interviewing subjects carries the risk of retraumatization (Collogan, Tuma, Dolan-Sewell, Borja & Fleischman, 2004; Norris, 2006; North & Pfefferbaum, 2002; Padgett, 2002). However, these research difficulties may not be applicable to the population of social workers responding to disasters and traumatic incidents. National, state and local disaster preparedness activities need to include policy, guidelines and funding for supporting evaluation and research in all aspects of disaster mental health response including how to mitigate the development of secondary traumatic stress in our social work response staff (Norris et al., 2006).
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th edn, Text Revision ed.). Washington, DC: American Psychiatric Association.
Bride, B. E. (2007). Prevalence of secondary traumatic stress among social workers. Social Work, 52, 63–70.
Bryant, R. A., Harvey, A. G., Dang, S., Sackville, T., & Basten, C. (1998). Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology, 66, 862–866.
Catherall, D. R. (1999). Coping with secondary traumatic stress: The importance of the therapist’s professional peer group. In B. H. Staumm, Ph.D. (Ed.) Secondary traumatic stress self-care issues for clinicians, researchers and educators (2nd ed.). (pp. 80–94). Baltimore: The Sidran Press.
Center For Mental Health Services. (2001, September 21). An overview of the crisis counseling assistance and training program (CCP-PG-01). Rockville, MD: Center for Mental Health Services.
Center For Mental Health Services. (2003). Mental health all hazards disaster planning guidance. (SMA-3829). Rockville, MD: US Department of Health and Human Services.
Cohen, J. A., Mannarino, A. P., Gibson, L. E., Cozza, S. J., Brymer, M. J., & Murray, L. (2005). Interventions for children and adolescents following disaster. In Ritchie, E. C., Watson, P. J., & Friedman, M. J. (Eds.) Interventions Following Mass Violence and Disaster (pp. 227–256). New York: The Guildford Press.
Collogan, L. K., Tuma, F., Dolan-Sewell, R., Borja, S., & Fleischman, A. R. (2004). Ethical Iissues pertaining to research in the aftermath of disaster. Journal of Traumatic Stress, 17(5), 363–373.
Cook, C. (January 9, 2007). Personal communication. Director, Louisiana Department of Health and Hospitals, Louisiana Spirit Crisis Counseling Assistance and Training Program.
Everly, G. S., & Mitchell, J. T. (1999). Critical incident stress management. A new era and standard of care in crisis intervention (second Ed). Ellicott City, MD: Chevron Publishing.
Federal Emergency Management Agency (2006). Retrieved from: http://www.Fema.gov.
Figley, C. R. (1994). Compassion fatigue: The stress of caring too much. Panama City, FL: Visionary Productions, Inc.
Figley, C. R. (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel.
Figley, C. R. (1999). Compassion fatigue: Toward a new understanding of the costs of caring. In B. H. Stamm (Ed.) Secondary traumatic stress. Self care issues for clinicians, researchers & educators (2nd ed.) (pp. 3–29). Baltimore, MD: Sidran Press.
Figley, C. R. (Ed.) (2002). Introduction. Treating Compassion Fatigue (pp.1–14). New York: Brunner-Routledge.
Galea, S., Ahern, J., Resnick, H., Kilpatrick, D., Mucuvalas, M., & Gold, J. (2002). Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine, 346(13), 982–987.
Hamblen, J., Gibson, L. E., Mueser, K., Rosenberg, S., Jankowski, K., Watson, P. J., & Friedman, M., J. (2003). Brief cognitive interventions for postdisaster distress. White River Junction, VT: Veterans Administration: National Center for PTSD.
Hamblen, J. L., Watson, P. J., Norris, F. H., & Pfefferbaum, B. J. (2005). Provider perspectives on disaster mental health services in Oklahoma City. Journal of Aggression, Maltreatment and Trauma, 10(12), 649–661.
Hillman, J. (January 10, 2007). Personal Communication. Director, Mississippi Department of Mental Health and Mental Retardation, Project Recovery Crisis Counseling Assistance & Training Program.
Jackson, G., & Cook, C. (1999). Crisis counseling program for the rural community. (SMA-99–3378). Rockville, MD: US Department of Health and Human Services.
Kassam-Adams, N. (1999). The risks of treating sexual trauma: Stress and secondary trauma in psychotherapists. In B. H. Stamm (Ed.) Secondary traumatic stress. Self care issues for clinicians, researchers & educators (2nd ed.). (pp. 37–51). Baltimore: Sidran Press.
Knight, A. & West, M. (January 16, 2007). Personal communication, Alabama State Departments of Health and Mental Health Disaster Response.
Litz, B., & Grey, M. (2002). Early intervention for trauma: Current status and future directions. Clinical Psychology: Science and Practice, 9, 112–134.
Lukens, E., & McFarlane. W. (2004). Psychoeducation as evidence based practice: Considerations for practice, research and policy. Brief Treatment and Crisis Intervention, 4(3), 205–225.
McCann, L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3(1), 131–149.
Mitchell, J. T., & Resnick, H. L. P. (1981). Emergency response to crisis. London: Prentice Hall International, Inc.
Munroe, J. F. (1999). Ethical issues associated with secondary trauma in therapists. In B. H. Stamm (Ed.) Secondary traumatic stress self care issues for clinicians, researchers and educators (2nd ed.). (pp. 211–230). Baltimore: Sidran Press.
Meyers, D., & Wee, D. (2002). Strategies for managing disaster mental health stress. In Charles R. Figley (Ed.), Treating compassion fatigue (pp. 181–212). New York: Brunner-Routledge.
Meyers, D., & Wee, D. (2005). Disaster mental health services. New York: Brunner-Routledge.
New York State Office of Mental Health. (2005). 2005–2009 Statewide Comprehensive Plan for Mental Health Services Appendix 5: Project Liberty Service Delivery. Retrieved, from http://www.omh.state.ny.us/omhweb/statewideplan/2005/appendix5.htm.
Norris, F. H., (2006). Disaster research methods: Past progress and future directions. Journal of Traumatic Stress, 19(2), 173–184.
Norris, F. H., Hamblen, J. L., Watson, P. J., Ruzek, J. I., Gibson, L. E., Pfefferbaum, B. J., Price, J. L., Stevens, S. P., Young, B. H., Friedman, M. J. (2006). Toward understanding and creating system of postdisaster care: A case study of New York’s response to the World Trade Center disaster. In E. C. Ritchie, P. J. Watson & M. J. Friedman (Eds.) Interventions following mass violence and disaster (pp. 343–365). New York: The Guildford Press.
Norris, F. H., Friedman, M. J., & Watson, P. J. (2002). 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry: Interpersonal and Biological Processes, 65(3), 240–260.
Norris, F. H., & Kaniasty, K. (1996). Received and perceived social support in times of stress: A test of the social support deteriorations deterrence model. Journal of Personality and Social Psychology, 71(3), 498–511.
North, C. S., & Pfefferbaum, B. (2002). Research on the mental health effects of terrorism. The Journal of the American Medical Association, 288(5), 633–636.
Padgett, D. (2002). Social work research on disasters in the aftermath of the September 11 tragedy: Reflections from New York City. Social Work Research, 26(3) 185–188.
Pearlman, L. A. (1999). Self care for trauma therapists: Ameliorating vicarious traumatization. In B. S. Staumm, Ph.D. (Ed.) Secondary traumatic stress self-care issues for clinicians, researchers and educators (2nd ed.). (pp. 51–64). Baltimore, MD: The Sidran Press.
Pearlman, L. A., & MacIan, P. (1995). Vicarious traumatization: An empirical study of the effects of trauma work on trauma therapists. Professional Psychology: Research and Practice, 26(6), 558–565.
Pearlman, L. A., & McCann, L. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3(1), 131–149.
Rose, S., Bisson, J., & Weseley, S. (2001). Psychological debriefing for prevention Posttraumatic Stress Disorder (PTSD). (Cochrane Review). In: The Cochrane Library, 3.
Ruzek, J. I. (2006). Disaster mental health training: Guidelines, considerations and recommendations. In E.C. Ritchie, P. J. Watson, M. J. Friedman (Eds.) Interventions following mass violence and disaster. (pp. 55–79). New York: The Guildford Press.
Schuster, M. A., Stein, B. D., Jaycox, L. A., Collins, R. L., Marshall, G. N., & Elliott, M. N. (2001). A national survey of stress reactions after the September 11, 2001 terrorist attacks. New England Journal of Medicine, 345(20), 1507–1512.
Stamm, B. H. (Ed.) (1995). Secondary traumatic stress self- care issues for clinicians, researchers and educators. Baltimore, MD: The Sidran Press.
Stamm, B. H. (1999). Introduction to the second edition. In B. H. Stamm (Ed.) Secondary traumatic stress: Self-care issues for clinicians, researchers and educators (2nd ed.) (pp. xix–xxxi). Baltimore: Sidran Press.
Stamm, B. H., Bieber, S. L., & Pearlman, L. A. (October, 1991). A preliminary report on scale construction and generalizability of the TSI Belief Scale. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies. Washington, DC.
Selye, H. (1976). The stress of life. New York: McGraw-Hill.
Substance Abuse and Mental Health Services Administration (2006). Retrieved from: http://www.samhsa.gov/publications/allpubs/SMA03-3829.
Veterans Administration (n.d.). Post trauma acute stress reaction civilian population. Retrieved from, www.oqp.med.va.gov/cpg/PTSD.
Wee, D. F., & Meyers, D. (2002). Stress response of mental health workers following disaster: The Oklahoma City Bombing. In Charles R. Figley (Ed.) Treating Compassion Fatigue (pp. 57–81). New York: Brunner-Routledge.
Weisler, R. H., Barbee, J. G., & Townsend, M. H. (2006). Mental health and recovery in the Gulf Coast after Hurricanes Katrina and Rita. Journal of the American Medical Association, 296(5), 585–588.
White, M., & Epston, D. (1990). Narrative means to therapeutic ends. New York, NY: W.W. Norton & Co.
Young, B. H., Ruzek, J. I., Wong, M., Salzer, M. S., & Naturale, A. J. (2006). Disaster mental health training: Guidelines, considerations and recommendations. In E. C. Ritchie, P. J. Watson & M. J. Friedman (Eds.), Interventions following mass violence and disaster (pp. 55–79). New York: The Guildford Press.
Young, B. H., Ford, J. D., Ruzek, J. I., Friedman, M. F., & Guzman, F. D. (1998). Disaster mental health services: A guidebook for clinicians and administrators. St. Louis, MO: Dept. of Veterans Affairs Employee Education System.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Naturale, A. Secondary Traumatic Stress in Social Workers Responding to Disasters: Reports from the Field. Clin Soc Work J 35, 173–181 (2007). https://doi.org/10.1007/s10615-007-0089-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10615-007-0089-1