Abstract
Some studies have suggested that infertility is a risk factor for endometrial, ovarian and breast cancer. The study aimed to create a comprehensive picture of the association between infertility and the risk of ovarian, endometrial and breast cancer, and whether any association could be explained by ovulatory disturbances, endometriosis or nulliparity. In a population-based cohort of 2,882,847 women, cox regression analysis was used to investigate cancer incidence among infertile women. Overall, infertility was associated with a higher incidence rate of ovarian (adjusted hazard ratio [aHR] 1.53, 95% confidence interval [CI] 1.38–1.71) and endometrial cancer (aHR 1.25, 95% CI 1.11–1.40), but not of breast cancer (aHR 0.96, 95% CI 0.92–1.01). Ovarian cancer incidence was higher in women diagnosed with endometriosis, and in nulliparous women with ovulatory disturbances, compared to women with none of the diagnoses. Endometrial cancer incidence was higher in women with ovulatory disturbances, but not in women with endometriosis. These findings suggest that infertility could have long-term consequences of importance to physicians and public health workers.
Similar content being viewed by others
Introduction
Infertility is among the most common diseases affecting young adults. It is estimated that one in seven couples trying to conceive are diagnosed with infertility [1], and female causes likely contribute to more than half of cases [2, 3]. Hormonal disorders affecting ovulation, including polycystic ovary syndrome (PCOS), are the most common causes of female infertility. Tubal factor infertility is also common, while endometriosis contributes to a smaller number of cases [2].
Cancers of the ovary, endometrium and breast are related to several hormonal and reproductive risk factors. Nulliparity, early menarche and late menopause are associated with higher risk of these malignancies, while the risk declines with each live birth [4,5,6]. The risk of breast cancer also increases with higher age at first birth [4], whereas pregnancy later in life seems to lower the risk of ovarian and endometrial cancer [5, 6]. Similarly, oral contraceptive use has been linked to a temporary increase in breast cancer risk [4], and a lower risk of ovarian and endometrial cancer [5, 6].
A number of previous studies have investigated the associations between fertility treatments using hormonal stimulation and the risk of breast and gynecological cancers. A recurring issue in these studies is the potential confounding by the underlying infertility [7,8,9]. Since both causes and consequences of infertility could influence cancer risk, the relationship is complex. The associations between endometriosis and ovarian cancer, as well as between PCOS and endometrial cancer, are fairly well established [10, 11]. Sustained estrogen stimulation to the endometrium without an opposed antiestrogenic effect of progesterone, which is the usual feature of chronic anovulation and PCOS, has a recognized carcinogenic effect in the development of some endometrial cancers. The association between endometriosis and ovarian cancer is less understood and inflammatory features associated with endometriosis have been proposed as predisposing to ovarian cancer [12]. Additionally, some studies have suggested that infertility per se is a risk factor for endometrial, ovarian and breast cancer [13,14,15,16,17], though this is debated [18,19,20]. It is also unclear whether these associations are attributable to any specific underlying cause of infertility.
The aim of this study was to create a comprehensive picture of the association between infertility and the risk of ovarian, endometrial and breast cancer in a large population-based cohort of Swedish women. We also aimed to investigate if such associations could be explained by either ovulatory disturbances, endometriosis or nulliparity.
Materials and methods
Study population
The study population comprised women born 1942–1992 who were registered in the population-based Swedish Multi-Generation Register (MGR) (n = 3,626,265). The MGR includes individuals born since 1932 and residing in Sweden 1961 or later, with links to their parents [21]. We used the personal identification number, which is uniquely assigned to all Swedish residents, for linkage between the MGR and other Swedish registers.
Women with invalid personal identification numbers (n = 4868) were excluded. Furthermore, as inclusion criteria women had to be alive and residing in Sweden at age 20 with less than five children. Hence, we excluded women who died prior to age 20 (n = 32,707), who immigrated after age 20 (n = 701,160), and women with more than four children prior to age 20 (n = 12). In addition, women diagnosed with any malignant disease before age 20 were excluded (n = 4671). After these criteria were applied, the cohort comprised 2,882,847 women. In all regression analyses, women missing information on education and/or country of birth were also excluded (n = 111,826). In the analyses of ovarian cancer incidence, 78 women who had bilateral oophorectomy before age 20 were also excluded. In the analyses of endometrial cancer incidence, 77 women with hysterectomy before age 20 were excluded.
Exposure information
Information on diagnoses related to infertility was obtained from the National Patient Register (NPR), where in-patient care has been recorded since 1964 and specialist out-patient care since 2001, according to the current version of the International Classification of Diseases (ICD) [22]. The corresponding ICD codes for these diagnoses during the study period are listed in Supplementary Table 1.
To address the underlying cause of infertility, we used diagnoses of endometriosis and ovulatory disturbances in combination with infertility as a proxy for infertility due to these disorders. Prior to 2001, diagnoses of endometriosis and ovulatory disturbances were only recorded in in-patient records, and thus women with these diagnoses in out-patient care prior to 2001 will not be captured by the proxy. Ovulatory disturbances were defined as having a diagnosis of ovarian dysfunction, (including PCOS), menstrual disturbances (including absent, rare or scanty menstruation) or infertility due to anovulation. Women diagnosed with endometriosis or infertility due to endometriosis were categorized as having endometriosis.
We included diagnoses of female infertility, ovulatory disturbances and endometriosis at age 15 or later. Median ages at diagnosis were 30.6 years for infertility (inter-quartile range [IQR] 27.2–34.2), 27.4 years for ovulatory disturbances (IQR 22.4–33.3) and 35.4 years for endometriosis (IQR 28.4–43.7).
Cancer
Since 1958, diagnoses of cancer in all Swedish residents have been recorded in the Swedish Cancer Register (SCR). The register includes date of diagnosis, hospital and tumor site coded using the 7th and current version of ICD.
In the present study, the cancers of interest were defined as morphologically verified malignant tumors of the breast (ICD-7 code 170), ovary, fallopian tube and broad ligaments (ICD-7 175), or uterine body (ICD-7 172). Women with a first diagnosis of these cancers during follow-up were considered cases. Women with any diagnosis of malignant disease (ICD-7 140-205) before start of follow-up were excluded, and women diagnosed with a malignant disease other than those studied during the study period were censored at date of diagnosis. The 83 women who were diagnosed with both ovarian and endometrial primary malignant tumors on the same date were included as cases for both cancer types.
Other covariates
The woman’s date of birth, parity and birthdate of each child were obtained from the MGR.
From the Total Population Register we obtained each woman’s country of birth as well as any migrations in or out of Sweden. Date of death was obtained from the Cause of Death Register and highest attained education level from the Education Register.
The NPR was used to identify women who had gone through bilateral oophorectomy, hysterectomy and salpingectomy. Surgeries performed up to 60 days before cancer diagnosis were assumed to be related to the cancer treatment and not included as covariates or censoring events (483 bilateral oophorectomies, 498 hysterectomies and 634 salpingectomies).
Statistical analyses
Person-time at risk was accrued from the date of the 20th birthday until the date of first breast or gynecological cancer diagnosis, or censoring at date of other cancer diagnosis, death, emigration or birth of the fifth child. Censoring at fifth child was done to simplify analyses, since follow-up time was split on parity and only 1% of cancer cases occurred in women with five or more children. In the analysis of ovarian cancer incidence, follow-up time was also censored at date of bilateral oophorectomy, while date of hysterectomy was used for censoring in analyses of endometrial cancer, since these women were no longer at risk for each respective tumor.
Cox proportional hazard models were used to estimate hazard ratios (HRs, which can be interpreted as incidence rate ratios), with 95% confidence intervals (CIs) for the cancers of interest, using attained age as the timescale.
In the main models, infertility was entered as a time-dependent exposure at the date of diagnosis. Women with and without infertility diagnosis were subdivided into three groups having ovulatory disturbances, endometriosis, or neither, resulting in six exposure categories. These categories were entered into the models as time-dependent exposures, i.e. a woman changed exposure category at the earliest date of diagnosis and could therefore contribute person-time to more than one category. Women diagnosed with both ovulatory disturbances and endometriosis were included in the category ovulatory disturbances (n = 2356).
Calendar time (split into 10-year intervals), parity/age at first birth and salpingectomy were included in the models as time-dependent covariates. When not used for censoring, hysterectomy and bilateral oophorectomy were also included as time-dependent covariates. Country of birth (Nordic, non-Nordic) and education level (9-year compulsory, secondary school < 3 or 3 years, higher education < 3 or ≥ 3 years) were included as fixed covariates. Current parity (nulliparous; 1, 2, 3 or 4 children) and age at first birth (< 25, 25–35 or ≥ 35 years) were combined into 13 categories.
The proportional hazards assumption was assessed using tests based on Schoenfeld residuals. The hazards were proportional overall, with some indication of stronger relative effects on ovarian cancer in younger ages where rates (and number of events) were low. Since early and late onset cancers may have different risk factors, we investigated potential differences between pre- and postmenopausal cancer by splitting follow-up time at the 50th birthday (as an approximation of menopause). For each outcome, we also examined interactions with nulliparity, through splitting follow-up time at the date of first birth. Interactions were assessed using likelihood ratio tests comparing models with and without interaction terms. In sensitivity analyses, women diagnosed with both ovulatory disturbances and endometriosis were excluded from the main models, to investigate whether any associations with ovulatory disturbances were influenced by co-occurring endometriosis. For each outcome, multivariable adjusted models not including parity/age at first birth were fitted to examine potential mediation through these factors.
Data was prepared using SAS software (version 9.4, SAS Institute Inc., Cary, N.C., USA) and statistical analyses performed using Stata (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). All tests were two-sided with a significance level of 5%.
The Ethical Review Board in Stockholm, Sweden approved this study (ethical approval 2013/1849-31/2, amendment 2014/118-32).
Results
Study population characteristics, by diagnosis of infertility, are presented in Table 1. Women born before 1950 and after 1980 were less likely to have a diagnosis of infertility. Infertile women were more likely to have higher education, to be older at their first birth and to have fewer children at the end of the study follow-up. Among infertile women, 19,299 (16.4%) were diagnosed with ovulatory disturbances and 14,030 (11.9%) with endometriosis, compared to 41,617 (1.5%) and 54,797 (2.0%) women with no infertility diagnosis. A history of salpingectomy or hysterectomy was more common among infertile women.
Of the 2,882,847 women in the cohort, 117,500 (4.1%) had a diagnosis of infertility. The mean follow-up time was 23.4 years among non-infertile women and 25.8 years among women with infertility. In non-infertile women, 52,601 women were diagnosed with breast cancer, 6337 with ovarian cancer and 6152 with endometrial cancer during 64,765,032 years of follow-up. Among women with a diagnosis of infertility, there were 2133 breast cancer, 392 ovarian cancer and 318 endometrial cancer cases, respectively, during 3,035,653 person-years. Among non-infertile women, the crude incidence rates were 81.2 cases of breast cancer, 9.8 cases of ovarian cancer and 9.0 cases of endometrial cancer per 100,000 person-years. The corresponding rates among infertile women, were 70.3 breast cancer cases, 12.9 ovarian cancer cases and 10.5 endometrial cancer cases per 100,000 person-years, respectively.
Breast cancer
Results for breast cancer incidence are presented in Table 2. Neither infertility nor related diagnoses were associated with a higher incidence of breast cancer in the multivariable adjusted analysis. Parity and age at first birth did not seem to influence these results (Supplementary Table 2).
We found no evidence for an effect modification by parity (adjusted p value = 0.2580). These results are presented in Supplementary Table 3.
When stratifying by age, the effect modification was statistically significant (adjusted p value 0.0124) (Supplementary Table 3). While none of the diagnoses were associated with post-menopausal breast cancer incidence, the incidence of pre-menopausal breast cancer was somewhat lower among women diagnosed with infertility and endometriosis (adjusted HR [aHR] = 0.79 [95% CI 0.65–0.95]), or infertility alone (aHR 0.92, 95% CI 0.86–0.99).
Ovarian cancer
Among all infertile women, the adjusted HR of ovarian cancer was 1.53 (95% CI 1.38–1.71) compared to women without infertility (Table 3). The incidence of ovarian cancer was higher among women with ovulatory disturbances (aHR 1.53, 95% CI 1.18–1.98), endometriosis (aHR 1.77, 95% CI 1.53–2.05) and infertility (aHR 1.53, 95% CI 1.36–1.72), compared to women with none of these diagnoses. Women diagnosed with both infertility and ovulatory disturbances did not have a significantly higher incidence of ovarian cancer (aHR 1.12, 95% CI 0.68–1.87), though the small number of cases in this group produced uncertain estimates. The highest incidence of ovarian cancer was seen in women diagnosed with both infertility and endometriosis (aHR 2.19, 95% CI 1.70–2.82). The associations between infertility, related diagnoses and ovarian cancer were slightly stronger when not adjusting for parity and age at first birth (Supplementary Table 2).
Results from the models stratified by parity and by age are presented in Supplementary Table 4. The effect modification was statistically significant (adjusted p value = 0.0333). Among nulliparous women, diagnoses of ovulatory disturbances, endometriosis or infertility were all associated with a higher incidence of ovarian cancer, compared to women with none of these diagnoses. Parous women diagnosed with endometriosis, infertility or a combination of both also had a higher incidence of ovarian cancer. Ovulatory disturbances, with or without infertility, were not significantly associated with an increased incidence of ovarian cancer in parous women.
The associations with ovarian cancer were modified by age (adjusted p value = 0.0002) (Supplementary Table 4). Compared to women with no infertility-related diagnosis, women with ovulatory disturbances had a higher incidence of ovarian cancer before menopause, but not after. The incidence of both pre- and post-menopausal ovarian cancer was higher in women diagnosed with endometriosis, infertility, or both. These associations were stronger before menopause. Women diagnosed with ovulatory disturbances and infertility did not have significantly higher incidence of either pre- or postmenopausal ovarian cancer.
Endometrial cancer
Infertile women had a higher incidence of endometrial cancer (aHR 1.25, 95% CI 1.11–1.40) compared to fertile women (Table 4). Women diagnosed with either infertility (aHR 1.21, 95% CI 1.07–1.38) or ovulatory disturbances (aHR 1.45, 95% CI 1.12–1.88) had a higher incidence of endometrial cancer, and the highest incidence was found in women with both these diagnoses (aHR 2.90, 95% CI 2.05–4.08). However, the incidence of endometrial cancer was not increased among women exclusively diagnosed with endometriosis (aHR 0.94, 95% CI 0.76–1.17), or in combination with infertility (aHR 0.87, 95% CI 0.58–1.30). The associations with infertility and ovulatory disturbances were stronger when not adjusting for parity and age at first birth (Supplementary Table 2).
The associations between ovulatory disturbances, infertility, and endometrial cancer appeared to be stronger in nulliparous women (adjusted p value = 0.0414) (Supplementary Table 5). Being diagnosed with both infertility and ovulatory disturbances was associated with a higher incidence of endometrial cancer in both nulliparous (aHR 3.46, 95% CI 2.22–5.38) and parous women (aHR 2.28, 95% CI 1.32–3.93). Nulliparous women diagnosed with either ovulatory disturbances (aHR 2.20, 95% CI 1.51–3.20) or infertility (1.28, 95% CI 1.08–1.53) also had increased incidences of endometrial cancer (Table 4).
When stratifying by age, the higher incidence of endometrial cancer was only present in women below the age of 50 (adjusted p value < 0.0001) (Supplementary Table 5). After adjustments, the incidence of pre-menopausal endometrial cancer was higher in women diagnosed with ovulatory disturbances (aHR 4.09, 95% CI 2.79–5.99), infertility (aHR 1.66, 95% CI 1.29–2.13), or both (aHR 8.09, 95% CI 5.38–12.15). None of the diagnoses were associated with a significantly higher incidence of post-menopausal endometrial cancer.
Sensitivity analysis
Excluding the 2356 women diagnosed with both ovulatory disturbances and endometriosis for the analyses of breast cancer, ovarian cancer and endometrial cancer did not alter the interpretation of the results in any of the analyses.
Discussion
In this large population-based study, we examined the risk of cancer in women with a diagnosis of infertility, and examined explanatory variables such as ovulatory disturbances, and endometriosis as well. Our overall findings indicate that infertile women had higher risks of ovarian and endometrial cancer, but the risk of breast cancer was not found to be increased. Ovulatory disturbances were associated with higher ovarian cancer risk among nulliparous women, and with higher endometrial cancer risk overall. Endometriosis was associated with a higher risk of ovarian cancer but not of endometrial cancer.
Breast cancer
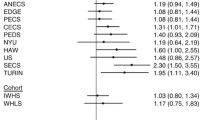
We found no increase in breast cancer risk among women with infertility or related diagnoses. These findings are in line with several previous studies on breast cancer risk in women with infertility [23,24,25], PCOS, [26], or endometriosis [27]. However, in a recent study, Jensen et al. [14] found a slightly higher risk of breast cancer in a cohort of infertile women, compared to the general population. The reported standardized incidence ratios (SIRs) were based on population rates adjusted for parity, age and calendar time. In our study, infertility was associated with a higher risk of breast cancer in the age-adjusted models, but not in the fully adjusted analysis. It is possible that the risk reported by Jensen et al. was influenced by factors such as higher age at first birth among infertile women. Most previous studies have presented SIRs adjusted only for age and calendar year, which could explain why the risk of breast cancer was found higher in some of them [15, 17, 28,29,30]. It is reasonable to assume that parity and age at first birth act as mediators rather than confounders in the studied association. They can also be seen as a proxy for several different exposures, mainly changes in the tissue that occur during pregnancy and lactation that influence breast cancer risk. However, we found no associations with breast cancer risk whether adjusting for parity and age at first birth or not.
Ovarian cancer
Infertile women had a higher incidence rate of ovarian cancer in our study. These results are similar to those of a large prospective cohort study [16], as well as two studies on infertile populations [14, 15]. In contrast, no increased risk was found in two case–control studies [31, 32] and two smaller studies involving infertile women only [17, 23]. Like most previous studies [27, 30, 33,34,35,36], we found a higher risk of ovarian cancer among women diagnosed with endometriosis. The association was similar in nulliparous and parous women, and also seemed to persist after menopause, though less pronounced. The mechanism behind this association is not entirely understood and several hypotheses have been proposed, including an increased oxidative stress caused by retrograde menstruation as well as changes in the microenvironment that promotes carcinogenesis [12]. We also found a higher risk of ovarian cancer among women diagnosed with ovulatory disturbances, which appeared to be confined to nulliparous premenopausal women. Women diagnosed both with infertility and ovulatory disturbances did not have a significantly higher risk of ovarian cancer, although it should be noted that estimates were based on small numbers. Increased levels of androgens in PCOS could theoretically influence ovarian cancer risk [11]. Previous studies on women with PCOS [26, 37], and women with androgen excess or menstrual disorders [29], have not found statistically significant associations with ovarian cancer. However, these studies included few ovarian cancer cases.
Endometrial cancer
We found a higher risk of endometrial cancer among infertile compared to fertile women. The risk was also higher among women diagnosed with ovulatory disturbances, especially in combination with infertility. This risk appeared to be higher among nulliparous women and only evident before menopause. Our results are in agreement with those from a pooled analysis by Yang et al. [13], as well as several previous studies comparing risks among infertile women and women with PCOS to the general population [17, 23, 26, 29, 37, 38]. The study by Jensen et al. [14] did not find a higher risk of endometrial cancer among infertile women. Similar to a recent report from a prospective cohort in the US [27], women with endometriosis did not have a higher risk of endometrial cancer in our study. A Danish cohort reported a higher SIR of endometrial cancer in women with endometriosis, adjusted only for age and calendar year [30]. Overall, our results do not suggest an independent effect of infertility on endometrial cancer risk, but rather that the risk among women with infertility is associated with ovulatory disturbances. It is likely that PCOS is underlying the association, since the main problem with PCOS is a hormonal imbalance with a high ovarian estrogen production without progesterone counteraction, which in turn is a known risk factor for endometrial cancer. These features typically lead to menstrual irregularities due to a chronic and prolonged endometrial stimulation and a later age of menopause onset [39].
Strengths and limitations
To our knowledge, this is one of the largest cohort studies to date on infertility and gynecological cancers. By utilizing Swedish population-based registers with essentially complete follow-up, we were able to accurately identify incident cancers as well as control for many important confounding variables while eliminating the risk of recall bias. The estimated completeness of the SCR for solid tumors is over 95% [40]. Diagnoses of infertility ascertained by physicians were recorded in the NPR for the duration of study follow-up.
Some limitations need to be considered when interpreting our findings. The NPR does not cover primary health care, and specialist out-patient care has only been included since 2001, meaning that some women with infertility-related problems were likely classified as non-infertile. This could bias the results towards the null, although any such effect is likely small given the large comparison group of non-infertile women. Diagnoses of infertility from in-patient care may differ from those recorded in out-patient care, and may reflect different subsets of women prior to and after 2001. However, infertility was more commonly treated in in-patient care during the beginning of the study period. Diagnoses of ovulatory disturbances were mainly captured in out-patient care records, resulting in shorter follow-up and fewer cancer cases among women with these diagnoses. It is also likely that many women with infertility due to ovulatory disturbances were categorized as having only a diagnosis of infertility. Since the cause of infertility was not specified for most women, the reasons for the associations with infertility alone could not be investigated further. The categories of infertility combined with endometriosis or ovulatory disturbances could also include women with infertility due to other causes, potentially diluting the associations.
A woman’s age at menarche and menopause is not recorded in population registers. Early menarche has been associated with a higher risk of ovarian, endometrial and breast cancer [4,5,6]. Since infertility seems to be more common in women with late menarche [41], this could bias the results towards the null. Age at menopause should not confound associations between infertility and cancer as it occurs after the reproductive period. In order to investigate potential effect modification by menopausal status, we used the 50th birthday as a cut-off.
For this large cohort of women, we used information collected on infertility and cancer diagnoses. However, in the group of women with a diagnosis of infertility, information on received hormonal treatments was not available. Therefore, we were unable to investigate whether the associations were mediated by any treatment. It is reassuring that most recent studies and meta-analyses have not found increased cancer risks in women who have undergone hormonal fertility treatments [42]. In a recent British study, ovarian cancer risk was higher than expected among women treated with assisted reproductive technology [9]. Because the higher risk was limited to women with endometriosis or low parity, the authors suggested that the risk was likely due to these characteristics and not the treatment itself.
Finally, we did not have information on additional hormonal treatments such as oral contraceptives or hormonal replacement after menopause, nor on the women’s weight. Oral contraceptives are associated with a lower risk of ovarian and endometrial cancer, and could potentially influence the studied associations if infertile women use them less than other women. On the other hand, oral contraceptives are also currently being prescribed for the treatment of endometriosis and PCOS. It is unlikely that differential use of these drugs could explain the results of this study. Obesity is associated with both PCOS and with an increased risk of endometrial cancer. However, we were unable to investigate whether this association was mediated by weight in our study.
Conclusions
The results from this large population-based study suggest that infertile women may have a higher risk of certain cancers, such as gynecological cancers, but not of breast cancer. Our data confirm findings of previous studies on the increased risk of ovarian cancer in women with infertility and endometriosis, and support that ovulatory disturbances, probably due to underlying PCOS, increased the risk of endometrial cancer in infertile women. Additionally, we found an increased risk of ovarian cancer among nulliparous women with ovulatory disturbances. Women with endometriosis did not have a higher risk of endometrial cancer. Other large-scale studies are needed to confirm these findings.
While the treatment of infertility rightly focuses on helping the couple conceive, the long-term consequences of female infertility and related disorders also merit the attention of physicians and public health workers.
References
Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility–a systematic review of prevalence studies. Hum Reprod Update. 2011;17:575–88.
Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988–1989). Hum Reprod. 1991;6:811–6.
Farhi J, Ben-Haroush A. Distribution of causes of infertility in patients attending primary fertility clinics in Israel. Isr Med Assoc J. 2011;13:51–4.
Rojas K, Stuckey A. Breast cancer epidemiology and risk factors. Clin Obstet Gynecol. 2016;59:651–72.
Hunn J, Rodriguez GC. Ovarian cancer: etiology, risk factors and epidemiology. Clin Obstet Gynecol. 2012;55:3–23.
Ali AT. Reproductive factors and the risk of endometrial cancer. Int J Gynecol Cancer. 2014;24:384–93.
Practice Committee of the American Society for Reproductive Medicine. Fertility drugs and cancer: a guideline. Fertil Steril. 2016;106:1617–26.
Lundberg FE, Iliadou AN, Rodriguez-Wallberg K, Bergh C, Gemzell-Danielsson K, Johansson ALV. Ovarian stimulation and risk of breast cancer in Swedish women. Fertil Steril. 2017;108:137–44.
Williams CL, Jones ME, Swerdlow AJ, Botting BJ, Davies MC, Jacobs I, et al. Risks of ovarian, breast, and corpus uteri cancer in women treated with assisted reproductive technology in Great Britain, 1991–2010: data linkage study including 2.2 million person years of observation. BMJ. 2018;362:k2644.
Zafrakas M, Grimbizis G, Timologou A, Tarlatzis BC, Dubuisson J-B, Cantonal HF, et al. Endometriosis and ovarian cancer risk: a systematic review of epidemiological studies. Front Surg. 2014;1:14.
Harris HR, Terry KL. Polycystic ovary syndrome and risk of endometrial, ovarian, and breast cancer: a systematic review. Fertil Res Pract. 2016;2:14.
Kobayashi H. Potential scenarios leading to ovarian cancer arising from endometriosis. Redox Rep. 2016;21:119–26.
Yang HP, Cook LS, Weiderpass E, Adami H-O, Anderson KE, Cai H, et al. Infertility and incident endometrial cancer risk: a pooled analysis from the epidemiology of endometrial cancer consortium (E2C2). Br J Cancer. 2015;112:925–33.
Jensen A, Sharif H, Olsen JH, Kjaer SK. Risk of breast cancer and gynecologic cancers in a large population of nearly 50,000 infertile Danish women. Am J Epidemiol. 2008;168:49–57.
Brinton LA, Westhoff CL, Scoccia B, Lamb EJ, Althuis MD, Mabie JE, et al. Causes of infertility as predictors of subsequent cancer risk. Epidemiology. 2005;16:500–7.
Tworoger SS, Fairfield KM, Colditz GA, Rosner BA, Hankinson SE. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol. 2007;166:894–901.
Lerner-Geva L, Rabinovici J, Olmer L, Blumstein T, Mashiach S, Lunenfeld B. Are infertility treatments a potential risk factor for cancer development? Perspective of 30 years of follow-up. Gynecol Endocrinol. 2012;28:809–14.
Hanson B, Johnstone E, Dorais J, Silver B, Peterson CM, Hotaling J. Female infertility, infertility-associated diagnoses, and comorbidities: a review. J Assist Reprod Genet. 2017;34:167–77.
Cetin I, Cozzi V, Antonazzo P. Infertility as a cancer risk factor—a review. Placenta. 2008;29(Suppl B):169–77.
Gabriele V, Gapp-Born E, Ohl J, Akladios C, Mathelin C. Infertility and breast cancer: is there a link? Updated review of the literature and meta-analysis. Gynécologie Obs Fertil. 2016;44:113–20.
Statistics Sweden. Multi-generation register 2012. A description of contents and quality. Backgr Facts Popul Welf Stat. 2012;2013(1):2013.
Socialstyrelsen. Kvalitet och innehåll i patientregistret. Utskrivningar från slutenvården 1964–2007 och besök i specialiserad öppenvård (exklusive primärvårdsbesök) 1997–2007. The National Board of Health and Welfare; 2009.
dos Santos Silva I, Wark PA, McCormack VA, Mayer D, Overton C, Little V, et al. Ovulation-stimulation drugs and cancer risks: a long-term follow-up of a British cohort. Br J Cancer. 2009;100:1824–31.
Lerner-Geva L, Keinan-Boker L, Blumstein T, Boyko V, Olmar L, Mashiach S, et al. Infertility, ovulation induction treatments and the incidence of breast cancer—a historical prospective cohort of Israeli women. Breast Cancer Res Treat. 2006;100:201–12.
Terry KL, Willett WC, Rich-Edwards JW, Michels KB. A prospective study of infertility due to ovulatory disorders, ovulation induction, and incidence of breast cancer. Arch Intern Med. 2006;166:2484–9.
Gottschau M, Kjaer SK, Jensen A, Munk C, Mellemkjaer L. Risk of cancer among women with polycystic ovary syndrome: a Danish cohort study. Gynecol Oncol. 2015;136:99–103.
Poole EM, Lin WT, Kvaskoff M, De Vivo I, Terry KL, Missmer SA. Endometriosis and risk of ovarian and endometrial cancers in a large prospective cohort of U.S. nurses. Cancer Causes Control. 2017;28:437–45.
Kim J, Mersereau JE, Khankari N, Bradshaw PT, McCullough LE, Cleveland R, et al. Polycystic ovarian syndrome (PCOS), related symptoms/sequelae, and breast cancer risk in a population-based case–control study. Cancer Causes Control. 2016;27:403–14.
Brinton LA, Moghissi KS, Westhoff CL, Lamb EJ, Scoccia B. Cancer risk among infertile women with androgen excess or menstrual disorders (including polycystic ovary syndrome). Fertil Steril. 2010;94:1787–92.
Brøchner Mogensen J, Kjaer SK, Mellemkjaer L, Jensen A. Endometriosis and risks for ovarian, endometrial and breast cancers: a nationwide cohort study. Gynecol Oncol. 2016;143:87–92.
Asante A, Leonard PH, Weaver AL, Goode EL, Jensen JR, Stewart EA, et al. Fertility drug use and the risk of ovarian tumors in infertile women: a case-control study. Fertil Steril. 2013;99:2031–6.
Kurta ML, Moysich KB, Weissfeld JL, Youk AO, Bunker CH, Edwards RP, et al. Use of fertility drugs and risk of ovarian cancer: results from a U.S.-based case-control study. Cancer Epidemiol Biomarkers Prev. 2012;21:1282–92.
Koushik A, Grundy A, Abrahamowicz M, Arseneau J, Gilbert L, Gotlieb WH, et al. Hormonal and reproductive factors and the risk of ovarian cancer. Cancer Causes Control. 2017;28:393–403.
Stewart LM, Holman CD, Aboagye-Sarfo P, Finn JC, Preen DB, Hart R. In vitro fertilization, endometriosis, nulliparity and ovarian cancer risk. Gynecol Oncol. 2013;128:260–4.
Buis CC, van Leeuwen FE, Mooij TM, Burger CW, Group OP. Increased risk for ovarian cancer and borderline ovarian tumours in subfertile women with endometriosis. Hum Reprod. 2013;28:3358–69.
Bertelsen L, Mellemkjaer L, Frederiksen K, Kjaer SK, Brinton LA, Sakoda LC, et al. Risk for breast cancer among women with endometriosis. Int J Cancer. 2007;120:1372–5.
Shen CC, Yang AC, Hung JH, Hu LY, Tsai SJ. A nationwide population-based retrospective cohort study of the risk of uterine, ovarian and breast cancer in women with polycystic ovary syndrome. Oncologist. 2015;20:45–9.
Brinton L. Long-term effects of ovulation-stimulating drugs on cancer risk. Reprod Biomed. 2007;15:38–44.
Li J, Eriksson M, Czene K, Hall P, Rodriguez-Wallberg KA. Common diseases as determinants of menopausal age. Hum Reprod. 2016;31:2856–64.
Barlow L, Westergren K, Holmberg L, Talbäck M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48:27–33.
Guldbrandsen K, Håkonsen LB, Ernst A, Toft G, Lyngsø J, Olsen J, et al. Age of menarche and time to pregnancy. Hum Reprod. 2014;29:2058–64.
Kroener L, Dumesic D, Al-Safi Z. Use of fertility medications and cancer risk: a review and update. Curr Opin Obstet Gynecol. 2017;29:195–201.
Acknowledgements
This study was funded by the European Union Framework Program 7 (EU-FP7 259679), the Swedish Research Council (K2011-69X-21871-01-6; SIMSAM 340-2013-5867), and the Strategic Research Program in Epidemiology Young Scholar Awards, Karolinska Institutet.
Funding
This study was funded by the EU-FP7 Health program (Agreement 259679), the Swedish Research Council (K2011-69X-21871-01-6; SIMSAM 340-2013-5867), and the Strategic Research Program in Epidemiology Young Scholar Awards, Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lundberg, F.E., Iliadou, A.N., Rodriguez-Wallberg, K. et al. The risk of breast and gynecological cancer in women with a diagnosis of infertility: a nationwide population-based study. Eur J Epidemiol 34, 499–507 (2019). https://doi.org/10.1007/s10654-018-0474-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-018-0474-9