Abstract
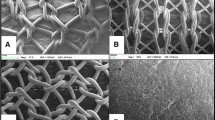
To determine whether the use of multiple layers of acellular bladder matrix (ABM) is more suitable for the treatment of abdominal wall hernia than a single layered ABM. The feasibility, biocompatibility and mechanical properties of both materials were assessed and compared. Biocompatibility testing was performed on 4 and 1 layered ABM. The matrices were used to repair an abdominal hernia model in 24 rabbits. The animals were followed for up to 3 months. Immediately after euthanasia, the implant site was inspected and samples were retrieved for histology, scanning electron microscopy and biomechanical studies. Both acellular biomaterials demonstrated excellent biocompatibility. At the time of retrieval, there was no evidence of infection. The matrices demonstrated biomechanical properties comparable to native tissue. Three hernias (25%) were found in the single layer ABM group and only 1 hernia (8%) was found in the 4 layer ABM group. Histologically, the matrix structure was intact and the cell density within the matrices decreased with time. The dominant cell type present within the matrices shifted from lymphocytes to fibroblasts over time. Both ABMs maintained adequate strength over time when used for hernia repair, and there was an extremely low incidence of adhesion formation. The single layer ABM showed enhanced cellular integration, while the 4 layer ABM reduced hernia formation. Either of these matrices may be useful as an off-the-shelf biomaterial for patients requiring fascial repair.






Similar content being viewed by others
References
Pu LL. Small intestinal submucosa (Surgisis) as a bioactive prosthetic material for repair of abdominal wall fascial defect. Plast Reconstr Surg. 2005;115(7):2127–31.
Amid PK, Shulman AG, Lichtenstein IL, Hakakha M. Biomaterials for abdominal wall hernia surgery and principles of their applications. Langenbecks Arch Chir. 1994;379(3):168–71.
Bellon JM, Contreras LA, Bujan J, Carrera-San Martin A. The use of biomaterials in the repair of abdominal wall defects: a comparative study between polypropylene meshes (Marlex) and a new polytetrafluoroethylene prosthesis (Dual Mesh). J Biomater Appl. 1997;12(2):121–35.
Klinge U, Klosterhalfen B, Muller M, Schumpelick V. Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg. 1999;165(7):665–73.
Majercik S, Tsikitis V, Iannitti DA. Strength of tissue attachment to mesh after ventral hernia repair with synthetic composite mesh in a porcine model. Surg Endosc. 2006;20(11):1671–4.
Menon NG, Rodriguez ED, Byrnes CK, Girotto JA, Goldberg NH, Silverman RP. Revascularization of human acellular dermis in full-thickness abdominal wall reconstruction in the rabbit model. Ann Plast Surg. 2003;50(5):523–7.
Demir U, Mihmanli M, Coskun H, Dilege E, Kalyoncu A, Altinli E, et al. Comparison of prosthetic materials in incisional hernia repair. Surg Today. 2005;35(3):223–7. doi:10.1007/s00595-004-2907-1.
Konstantinovic ML, Pille E, Malinowska M, Verbeken E, De Ridder D, Deprest J. Tensile strength and host response towards different polypropylene implant materials used for augmentation of fascial repair in a rat model. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(6):619–26. doi:10.1007/s00192-006-0202-y.
Krambeck AE, Dora CD, Sebo TJ, Rohlinger AL, DiMarco DS, Elliott DS. Time-dependent variations in inflammation and scar formation of six different pubovaginal sling materials in the rabbit model. Urology. 2006;67(5):1105–10. doi:10.1016/j.urology.2005.11.036.
Engelsman AF, van der Mei HC, Ploeg RJ, Busscher HJ. The phenomenon of infection with abdominal wall reconstruction. Biomaterials. 2007;28(14):2314–27.
Kaufman Z, Engelberg M, Zager M. Fecal fistula: a late complication of Marlex mesh repair. Dis Colon Rectum. 1981;24(7):543–4.
Bauer JJ, Salky BA, Gelernt IM, Kreel I. Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PTFE). Ann Surg. 1987;206(6):765–9.
Tyrell J, Silberman H, Chandrasoma P, Niland J, Shull J. Absorbable versus permanent mesh in abdominal operations. Surg Gynecol Obstet. 1989;168(3):227–32.
Voyles CR, Richardson JD, Bland KI, Tobin GR, Flint LM, Polk HC Jr. Emergency abdominal wall reconstruction with polypropylene mesh: short-term benefits versus long-term complications. Ann Surg. 1981;194(2):219–23.
James NL, Poole-Warren LA, Schindhelm K, Milthorpe BK, Mitchell RM, Mitchell RE, et al. Comparative evaluation of treated bovine pericardium as a xenograft for hernia repair. Biomaterials. 1991;12(9):801–9.
Rodgers BM, Maher JW, Talbert JL. The use of preserved human dura for closure of abdominal wall and diaphragmatic defects. Ann Surg. 1981;193(5):606–11.
Koizumi NJ, Inatomi TJ, Sotozono CJ, Fullwood NJ, Quantock AJ, Kinoshita S. Growth factor mRNA and protein in preserved human amniotic membrane. Curr Eye Res. 2000;20(3):173–7.
Voytik-Harbin SL, Brightman AO, Kraine MR, Waisner B, Badylak SF. Identification of extractable growth factors from small intestinal submucosa. J Cell Biochem. 1997;67(4):478–91. doi:10.1002/(SICI)1097-4644(19971215)67:4<478::AID-JCB6>3.0.CO;2-P.
Meinert M, Eriksen GV, Petersen AC, Helmig RB, Laurent C, Uldbjerg N, et al. Proteoglycans and hyaluronan in human fetal membranes. Am J Obstet Gynecol. 2001;184(4):679–85. doi:10.1067/mob.2001.110294.
Chun SY, Lim GJ, Kwon TG, Kwak EK, Kim BW, Atala A, et al. Identification and characterization of bioactive factors in bladder submucosa matrix. Biomaterials. 2007;28(29):4251–6.
Ram-Liebig G, Meye A, Hakenberg OW, Haase M, Baretton G, Wirth MP. Induction of proliferation and differentiation of cultured urothelial cells on acellular biomaterials. BJU Int. 2004;94(6):922–7. doi:10.1111/j.1464-410X.2004.05061.x.
Singelyn JM, Christman KL. Injectable materials for the treatment of myocardial infarction and heart failure: the promise of decellularized matrices. J Cardiovasc Transl Res. 2010;3(5):478–86. doi:10.1007/s12265-010-9202-x.
Zhang Y, He Y, Bharadwaj S, Hammam N, Carnagey K, Myers R, et al. Tissue-specific extracellular matrix coatings for the promotion of cell proliferation and maintenance of cell phenotype. Biomaterials. 2009;30(23–24):4021–8. doi:10.1016/j.biomaterials.2009.04.005.
Eberli D, Susaeta R, Yoo J, Atala A. Tunica repair with acellular bladder matrix maintains corporal tissue function. Int J Impot Res. 2007;19(6):602–9. doi:10.1038/sj.ijir.3901587.
Pariente JL, Kim BS, Atala A. In vitro biocompatibility assessment of naturally derived and synthetic biomaterials using normal human urothelial cells. J Biomed Mater Res. 2001;55(1):33–9.
Pariente JL, Kim BS, Atala A. In vitro biocompatibility evaluation of naturally derived and synthetic biomaterials using normal human bladder smooth muscle cells. J Urol. 2002;167(4):1867–71.
Ansaloni L, Cambrini P, Catena F, Di Saverio S, Gagliardi S, Gazzotti F, et al. Immune response to small intestinal submucosa (surgisis) implant in humans: preliminary observations. J Invest Surg. 2007;20(4):237–41. doi:10.1080/08941930701481296.
Sarikaya A, Record R, Wu CC, Tullius B, Badylak S, Ladisch M. Antimicrobial activity associated with extracellular matrices. Tissue Eng. 2002;8(1):63–71. doi:10.1089/107632702753503063.
Eberli D, Rodriguez S, Atala A, Yoo JJ. In vivo evaluation of acellular human dermis for abdominal wall repair. J Biomed Mater Res A. 2010;93(4):1527–38. doi:10.1002/jbm.a.32636.
Abraham GA, Murray J, Billiar K, Sullivan SJ. Evaluation of the porcine intestinal collagen layer as a biomaterial. J Biomed Mater Res. 2000;51(3):442–52.
el-Kassaby A, AbouShwareb T, Atala A. Randomized comparative study between buccal mucosal and acellular bladder matrix grafts in complex anterior urethral strictures. J Urol. 2008;179(4):1432–6.
Chen F, Yoo JJ, Atala A. Acellular collagen matrix as a possible “off the shelf” biomaterial for urethral repair. Urology. 1999;54(3):407–10.
Yoo JJ, Meng J, Oberpenning F, Atala A. Bladder augmentation using allogenic bladder submucosa seeded with cells. Urology. 1998;51(2):221–5.
Kwon TG, Yoo JJ, Atala A. Autologous penile corpora cavernosa replacement using tissue engineering techniques. J Urol. 2002;168(4 Pt 2):1754–8. doi:10.1097/01.ju.0000030103.53181.7d.
Hiles MC, Badylak SF, Geddes LA, Kokini K, Morff RJ. Porosity of porcine small-intestinal submucosa for use as a vascular graft. J Biomed Mater Res. 1993;27(2):139–44.
Klinge U, Conze J, Klosterhalfen B, Limberg W, Obolenski B, Ottinger AP, et al. Changes in abdominal wall mechanics after mesh implantation. Experimental changes in mesh stability. Langenbecks Arch Chir. 1996;381(6):323–32.
Han JG, Ma SZ, Song JK, Wang ZJ. Operative treatment of ventral hernia using prosthetic materials. Hernia. 2007;11(5):419–23.
Farhat WA, Chen J, Haig J, Antoon R, Litman J, Sherman C, et al. Porcine bladder acellular matrix (ACM): protein expression, mechanical properties. Biomed Mater. 2008;3(2):25015. doi:10.1088/1748-6041/3/2/025015.
Freytes DO, Badylak SF, Webster TJ, Geddes LA, Rundell AE. Biaxial strength of multilaminated extracellular matrix scaffolds. Biomaterials. 2004;25(12):2353–61.
Freytes DO, Stoner RM, Badylak SF. Uniaxial and biaxial properties of terminally sterilized porcine urinary bladder matrix scaffolds. J Biomed Mater Res B Appl Biomater. 2008;84(2):408–14. doi:10.1002/jbm.b.30885.
Freytes DO, Tullius RS, Badylak SF. Effect of storage upon material properties of lyophilized porcine extracellular matrix derived from the urinary bladder. J Biomed Mater Res B Appl Biomater. 2006;78(2):327–33. doi:10.1002/jbm.b.30491.
Ko R, Kazacos EA, Snyder S, Ernst DM, Lantz GC. Tensile strength comparison of small intestinal submucosa body wall repair. J Surg Res. 2006;135(1):9–17. doi:10.1016/j.jss.2006.02.007.
Soergel TM, Cain MP, Kaefer M, Gitlin J, Casale AJ, Davis MM, et al. Complications of small intestinal submucosa for corporal body grafting for proximal hypospadias. J Urol. 2003;170(4 Pt 2):1577–8; 8–9.
Hafez AT, El-Assmy A, El-Hamid MA. 4 layer versus 1 layer small intestinal submucosa for correction of penile chordee: experimental study in a rabbit model. J Urol. 2004;171(6 Pt 1):2489–91.
Alimoglu O, Akcakaya A, Sahin M, Unlu Y, Ozkan OV, Sanli E, et al. Prevention of adhesion formations following repair of abdominal wall defects with prosthetic materials (an experimental study). Hepatogastroenterology. 2003;50(51):725–8.
Butler CE, Prieto VG. Reduction of adhesions with composite AlloDerm/polypropylene mesh implants for abdominal wall reconstruction. Plast Reconstr Surg. 2004;114(2):464–73.
Dinsmore RC, Calton WC Jr, Harvey SB, Blaney MW. Prevention of adhesions to polypropylene mesh in a traumatized bowel model. J Am Coll Surg. 2000;191(2):131–6.
Judge TW, Parker DM, Dinsmore RC. Abdominal wall hernia repair: a comparison of sepramesh and parietex composite mesh in a rabbit hernia model. J Am Coll Surg. 2007;204(2):276–81. doi:10.1016/j.jamcollsurg.2006.11.003.
Clarke KM, Lantz GC, Salisbury SK, Badylak SF, Hiles MC, Voytik SL. Intestine submucosa and polypropylene mesh for abdominal wall repair in dogs. J Surg Res. 1996;60(1):107–14.
Acknowledgments
The authors wish to thank Jennifer Olson, Ph.D. for editorial assistance with this manuscript. This research was supported, in part, by Acell Inc., the Swiss National Research Foundation and Swiss Urological Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eberli, D., Atala, A. & Yoo, J.J. One and four layer acellular bladder matrix for fascial tissue reconstruction. J Mater Sci: Mater Med 22, 741–751 (2011). https://doi.org/10.1007/s10856-011-4242-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-011-4242-6