Abstract
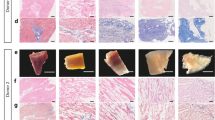
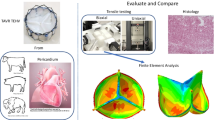
To achieve natural scaffolds for tissue engineering applications we decellularized bovine pericardial (BP) tissues according to two different protocols: a novel treatment based on Triton® X-100 (12 h, 4 °C) (BP1) and a trypsin/EDTA treatment (37 °C, 48 h) (BP2). Results were compared with commercially available acellular xenogeneic biomaterials, Veritas® and Collamed®. Biomechanical characteristics, high (Eh) and low (El) modulus of elasticity, of the fresh untreated tissue varied with the anatomical direction (apex to base (T) to transverse (L)) (mean ± SDEV): (41.63 ± 14.65–48.12 ± 10.19 MPa and 0.27 ± 0.05–0.30 ± 0.12 MPa respectively). BP1 had no mechanical effect (44.65 ± 19.73–52.67 ± 7.59 MPa and 0.37 ± 0.14–0.37 ± 0.11 MPa, respectively) but BP2 resulted in significant decrease in Eh and El (20.96 ± 8.17–36.82 ± 3.23 MPa and 0.20 ± 0.06–0.23 ± 0.06 MPa). Hysteresis ratio (h) varied (19–26 % of the loading energy) independently of anatomical direction. Glycosaminoglycans content was unaffected by BP1, while 22 % of chondroitin/dermatan sulphate and 60 % of hyaluronan were removed after BP2 treatment. Endothelial cell adhesion was achieved after 24 h and 3 days cell culture.







Similar content being viewed by others
References
Steinhoff G, et al. Tissue engineering of pulmonary heart valves on allogenic acellular matrix conduits-in vivo restoration of valve tissue. Circulation. 2000;102:I50–5.
Stock UA, et al. Tissue engineered valved conduits in the pulmonary circulation. J Thorac Cardiovasc Surg. 2000;119:732–40.
Sodian R, Hoerstrup SP, Sperling JS, Martin DP, Daebritz S, Mayer JE Jr, Vacanti JP. Evaluation of biodegradable, three-dimensional matrices for tissue engineering of heart valves. ASAIO J. 2000;46:107–10.
Shinoka T. Tissue engineered heart valves: autologous cell seeding on biodegradable polymer scaffold. Artif Organs. 2002;26:402–6.
Jockenhoevel S, et al. Fibrin gel—advantages of a new scaffold in cardiovascular tissue engineering. Eur J Cardiothorac Surg. 2001;19:424–30.
Flanagan TC. In vivo remodeling and structural characterization of fibrin-based tissue-engineered heart valves in the adult sheep model. Tissue Eng A. 2009;15:2965–76.
Ravi S, Chaikof EL. Biomaterials for vascular tissue engineering. Regen Med. 2010;5:107–20.
Badylak SF. Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol. 2004;12:367–77.
Gilbert TW, Sellaro TL, Badylak SF. Decellularization of tissues and organs. Biomaterials. 2006;27:3675–83.
Limpert JN, Desai AR, Kumpf AL, Fallucco MA, Aridge DL. Repair of abdominal wall defects with bovine pericardium. Am J Surg. 2009;198:e60–5.
Canda AE, Karaca A. Incisional hernia in action: the use of vacuum-assisted closure and porcine dermal collagen implant. Hernia. 2009;13:651–5.
Badylak SF. The extracellular matrix as a biologic scaffold material. Biomaterials. 2007;28:3587–93.
Mendoza-Novelo B, Avila EE, Cauich-Rodríguez JV, Jorge-Herrero E, Rojo FJ, Guinea GV, Mata-Mata JL. Decellularization of pericardial tissue and its impact on tensile viscoelasticity and glycosaminoglycan content. Acta Biomater. 2011;7:1241–8.
Rieder E, et al. Tissue engineering of heart valves: decellularized porcine and human valve scaffolds differ importantly in residual potential to attract monocytic cells. Circulation. 2005;111:2792–7.
Schmidt CE, Baier JM. Acellular vascular tissues: natural biomaterials for tissue repair and tissue engineering. Biomaterials. 2000;21:2215–31.
Doss M, Moid R, Wood JP, Miskovic A, Martens S, Moritz A. Pericardial patch augmentation for reconstruction of incompetent bicuspid aortic valves. Ann Thorac Surg. 2005;80:304–7.
Mavrilas D, Sinouris EA, Vynios DH, Papageorgakopoulou N. Dynamic mechanical characteristics of intact and structurally modified bovine pericardial tissues. J Biomech. 2005;38:761–8.
Iozzo RV, Murdoch AD. Proteoglycans of the extracellular environment: clues from the gene and protein side offer novel perspectives in molecular diversity and function. FASEB J. 1996;10:598–614.
Wilson GJ, Courtman DW, Klement P, Lee JM, Yeger H. Acellular matrix: a biomaterials approach for coronary artery bypass and heart valve replacement. Ann Thorac Surg. 1995;60:S353–8.
Bader A, Schilling T, Teebken OE, Brandes G, Herden T, Steinhoff G, Haverich A. Tissue engineering of heart valves—human endothelial cell seeding of detergent acellularized porcine valves. Eur J Cardiothorac Surg. 1998;14:279–84.
Bertipaglia B, et al. Cell characterization of porcine aortic valve and decellularized leaflets repopulated with aortic valve interstitial cells. Ann Thorac Surg. 2003;75:1274–82.
Korossis SA, Booth C, Wilcox HE, Watterson KG, Kearney JN, Fisher J, Ingham E. Tissue engineering of cardiac valve prostheses II: biomechanical characterization of decellularized porcine aortic heart valves. J Heart Valve Dis. 2002;11:463–71.
Liao J, Joyce EM, Sacks MS. Effects of decellularization on the mechanical and structural properties of the porcine aortic valve leaflet. Biomaterials. 2008;29:1065–74.
Cebotari S, et al. Construction of autologous human heart valves based on an acellular allograft matrix. Circulation. 2002;106:I63–8.
Patton JH Jr, Berry S, Kralovich KA. Use of human acellular dermal matrix in complex and contaminated abdominal wall reconstructions. Am J Surg. 2007;193:360–3.
Catena F, Ansaloni L, Gazzotti F, Gagliardi S, Di Saverio S, D’Alessandro L, Pinna AD. Use of porcine dermal collagen graft for hernia repair in contaminated fields. Hernia. 2007;11:57–60.
Kim H, Bruen K, Vargo D. Acellular dermal matrix in the management of high-risk abdominal wall defects. Am J Surg. 2006;192:705–9.
Papadas TA. Alterations in the content and composition of glycosaminoglycans in human laryngeal carcinoma. Acta Otolaryngol. 2002;122:330–7.
Reddy GK, Enwemeka CS. A simplified method for the analysis of hydroxyproline in biological tissues. Clin Biochem. 1996;29:225–9.
Fung YC. Elasticity of soft tissues in simple elongation. Am J Physiol. 1967;213:1532–44.
Anssari-Benam A, Bader DL, Screen HR. A combined experimental and modelling approach to aortic valve viscoelasticity in tensile deformation. J Mater Sci Mater Med. 2011;22:253–62.
Shah SR, Vyavahare NR. The effect of glycosaminoglycan stabilization on tissue buckling in bioprosthetic heart valves. Biomaterials. 2008;29:1645–53.
Sacks MS. Biaxial mechanical evaluation of planar biological materials. J Elast. 2000;61:199–246.
Braga-Vilela AS, Pimentel ER, Marangoni S, Toyama MH, de Campos Vidal B. Extracellular matrix of porcine pericardium: biochemistry and collagen architecture. J Membr Biol. 2008;221:15–25.
Simionescu D, Iozzo RV, Kefalides NA. Bovine pericardial proteoglycan: biochemical, immunochemical and ultrastructural studies. Matrix. 1989;9:301–10.
Danielson KG, Baribault H, Holmes DF, Graham H, Kadler KE, Iozzo RV. Targeted disruption of decorin leads to abnormal collagen fibril morphology and skin fragility. J Cell Biol. 1997;136:729–43.
Winnemöller M, Schmidt G, Kresse H. Influence of decorin on fibroblast adhesion to fibronectin. Eur J Cell Biol. 1991;54:10–7.
Coleman PJ. Evidence for a role of hyaluronan in the spacing of fibrils within collagen bundles in rabbit synovium. Biochim Biophys Acta. 2002;1571:173–82.
Bos KJ, Holmes DF, Meadows RS, Kadler KE, McLeod D, Bishop PN. Collagen fibril organisation in mammalian vitreous by freeze etch/rotary shadowing electron microscopy. Micron. 2001;32:301–6.
Acknowledgments
This work was partly supported by University of Patras research committee grand “K. Karatheodoris” #B711. We thank Synovis Surgical Innovations S.A., USA and Diophar S.A., GR for supplying Veritas® biomaterial for testing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pagoulatou, E., Triantaphyllidou, IE., Vynios, D.H. et al. Biomechanical and structural changes following the decellularization of bovine pericardial tissues for use as a tissue engineering scaffold. J Mater Sci: Mater Med 23, 1387–1396 (2012). https://doi.org/10.1007/s10856-012-4620-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4620-8