Abstract
A recently proposed mechanism-based disease systems model for osteoporosis (Schmidt et al., J Pharmacokinet Pharmacodyn 38:873–900, 2011) was applied to clinical data from post-menopausal women (n = 767) receiving various doses of the selective estrogen receptor modulator tibolone. Plasma bone-specific alkaline phosphatase activity and urinary N-telopeptide were used as biomarkers reflecting the activity of osteoblasts (bone forming cells) and osteoclasts (bone removing cells), respectively. These data were analyzed in conjunction with data on osteocalcin and on bone mineral density (BMD) (both lumbar spine and total hip), which reflect the activity of both cell types. While the dynamics of bone turnover markers changes rapidly, closely following changes in the activity of bone cells, changes in BMD are slower and have their own dynamics. Application of the mechanism-based disease systems model to the clinical data allowed for an adequate description of the data and yielded parameter estimates that are consistent with physiological values reported in the literature (Lemaire et al., J Theor Biol 229:293–309, 2004). The fitted model enabled characterization of (i) the critical time scales involved in disease progression, (ii) the dynamics of the system during onset and offset of the therapeutic intervention, and (iii) the distinction between responders and low-responders to tibolone treatment.





Similar content being viewed by others
References
Chan PL, Holford NH (2001) Drug treatment effects on disease progression. Annu Rev Pharmacol Toxicol 41:625–659
Post TM, Freijer JI, DeJongh J, Danhof M (2005) Disease system analysis: basic disease progression models in degenerative disease. Pharm Res 22:1038–49
Danhof M, de Jongh J, De Lange EC, Della Pasqua O, Ploeger BA, Voskuyl RA (2007) Mechanism-based pharmacokinetic-pharmacodynamic modeling: biophase distribution, receptor theory, and dynamical systems analysis. Annu Rev Pharmacol Toxicol 47:357–400
Schmidt S, Post TM, Peletier LA, Boroujerdi MA, Danhof M (2011) Coping with time scales in disease systems analysis: application to bone remodeling. J Pharmacokinet Pharmacodyn 38:873–900
Lemaire V, Tobin FL, Greller LD, Cho CR, Suva LJ (2004) Modeling the interactions between osteoblast and osteoclast activities in bone remodeling. J Theor Biol 229:293–309
Gallagher JC, Baylink DJ, Freeman R, McClung M (2001) Prevention of bone loss with tibolone in postmenopausal women: results of two randomized, double-blind, placebo-controlled, dose-finding studies. J Clin Endocrinol Metab 86:4717–4726
Post TM, Cremers SC, Kerbusch T, Danhof M (2010) Bone physiology, disease and treatment: towards disease system analysis in osteoporosis. Clin Pharmacokinet 49:89–118
Berning B, Bennink HJ, Fauser BC (2001) Tibolone and its effects on bone: a review. Climactic 4:120–136
Pilla Reddy V, Kozielska M, Johnson M, Vermeulen A, de Greef R, Liu J, Groothuis GM, Danhof M, Proost JH (2011) Structural models describing placebo treatment effects in schizophrenia and other neuropsychiatric disorders. Clin Pharmacokinet 50:429–50
Dayneka NL, Garg V, Jusko WJ (1993) Comparison of four basic models of indirect pharmacodynamic responses. J Pharmacokinet Biopharm 21:457–478
Earp JC, DuBois DC, Molano DS, Pyszczynski NA, Keller CE, Almon RR, Jusko WJ (2008) Modeling corticosteroid effects in a rat model of rheumatoid arthritis I: mechanistic disease progression model for the time course of collagen-induced arthritis in Lewis rats. J Pharmacol Exp Ther 326:532–545
Marathe DD, Marathe A, Mager DE (2011) Integrated model for denosumab and ibandronate pharmacodynamics in postmenopausal women. Biopharm Drug Dispos 32:471–481
Riggs MM, Peterson MC, Gastonguay MR (2012) Multiscale physiology-based modeling of mineral bone disorder in patients with impaired kidney function. J Clin Pharmacol 52:45S–53S
Greenspan SL, Emkey RD, Bone HG, Welss SR, Bell NH, Downs RW Jr, McKeever C, Miller SS, Davidson M, Bolognese MA, Mulloy AL, Heyden N, Wu M, Kaur A, Lombardi A (2002) Significant differential effects of alendronate, estrogen, or combination therapy on the rate of bone loss after discontinuation of treatment of postmenopausal osteoporosis. Ann Intern Med 137:875–883
Schmidt S, Post TM, Boroujerdi MA, van Kesteren C, Ploeger BA, Della Pasqua OE, Danhof M (2010) Disease progression analysis: towards mechanism-based models. In: Kimko HC, Peck CC (eds) Clinical trial simulations, 1st edn. Springer, New York, pp 437–459
de Winter W, DeJongh J, Post T, Ploeger B, Urquhart R, Moules I, Eckland D, Danhof M (2006) A mechanism-based disease progression model for comparison of long-term effects of pioglitazone, metformin and gliclazide on disease processes underlying type 2 diabetes mellitus. J Pharmacokinet Pharmacodyn 33:313–43
Titus L, Jackson E, Nanes MS, Rubin JE, Catherwood BD (1991) 1,25-Dihydroxy vitamin D reduces parathyroid hormone receptor number in ROS 17/2.8 cells and prevents the glucocorticoid-induced increase in these receptors: relationship to adenylate cyclase activation. J Bone Miner Res 6:631–637
Xie LY, Leung A, Segre GV, Yamamoto I, Abou-Samra AB (1996) Downregulation of the PTH/ PTHrP receptor by vitamin D3 in the osteoblast-like ROS 17/2.8 cells. Am J Physiol 270:E654–E660
Alliston T, Choy L, Ducy P, Karsenty G, Derynck R (2001) TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J 20:2254–2272
Ducy P, Schinke T, Karsenty G (2000) The osteoblast: a sophisticated fibroblast under central surveillance. Sci Agric 289:1501–1504
Komori T, Yagi H, Nomura S, Yamaguchi A, Sasaki K, Deguchi K, Shimizu Y, Bronson RT, Gao YH, Inada M, Sato M, Okamoto R, Kitamura Y, Yoshiki S, Kishimoto T (1997) Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell 89:755–764
Bone HG, Bolognese MA, Yuen CK, Kendler DL, Wang H, Liu Y, San Martin J (2008) Effects of denosumab on bone mineral density and bone turnover in postmenopausal women. J Clin Endocrinol Metab 93:2149–57
Rachner TD, Hadji P, Hofbauer LC (2012) Novel therapies in benign and malignant bone diseases. Pharmacol Ther 134:338–344
Ploeger BA, Holford NH (2009) Washout and delayed start designs for identifying disease modifying effect in slowly progressive diseases using disease progression analysis. Pharm Stat 8:225–38
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Derivation of the system (12)
In this appendix we briefly sketch how the model (9), (10) can be transformed into the system (12) for the dimensionless variables y = B/B 0 and z = C/C 0:
and
Derivation of the first equation of (12): We divide the equation for dB/dt in the system (9) by B 0 and so obtain
At baseline y = 1, and therefore
so that (24) can be written as
where we have used the definition of π C (C):
In light of the definition of σ(z) in (12), Eq. (26) has the required form. This completes the transformation of the first equation of the system (12).
The second equation of (12): Proceeding as with the first equation, we divide the equation for dC/dt in the system (9) by C 0 to obtain
By definition, the baseline values B 0 and C 0 are related through the equation
or, after some rearrangement,
Using (28) in (27) we eliminate many constants and arrive at the expression
which still contains the variable x.
In order to eliminate x we use the expression (10)
and conclude that
Therefore,
so that Eq. (29) can be written as
This completes the transformation of the Eqs. (9) and (10) into the system (12) for the dimensionless variables y and z.
Appendix 2: Dynamical systems behaviour
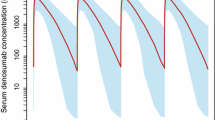
An important feature of the reduced disease system model is that it enables an analysis of the dynamical systems behaviour. This can be of value for optimizing the design of clinical trial protocols, particularly if the objective is to make a distinction between a symptomatic versus a disease-modifying effect [24]. A phase-plane analysis (cf. Fig. 6) was introduced as a novel tool to evaluate the dynamic behaviour of the system aiming at the prediction of the effect of a therapeutic intervention.
Within the context of the Reduced Model (cf. (4)) the state of the RANK–RANKL–OPG system is given by the osteoblast and osteoclast activities B and C. Their relative values with respect to their baseline values are denoted by y = B/B 0 and z = C/C 0. This pair of quantities y and z, which we refer to as the state of the system, can be represented geometrically by a point in the (z, y)-plane, often referred to as the State Space. As time progresses and the state changes, the point (z, y) moves through state space and traces out an Orbit.
In Fig. 6 we show four orbits, which separate after 100 days when calcium and tibolone treatment starts. The green orbit follows the disease progression, the blue orbit follows the system when it is affected by calcium treatment, the Placebo Orbit, and two red orbits demonstrate the impact of tibolone treatment, one for infinite treatment (solid) and one for treatment terminating after 1,000 days (dashed).
Orbits of solutions of the system (19) in red in the (z, y)-plane. The green curve is the orbit in the absence of any treatment, the blue curve is the orbit in the presence of calcium treatment alone and the red curves are orbits caused by calcium and tibolone treatment combined. The solid red curve is the orbit during continuous tibolone treatment, the dashed curve the continuation after termination and washout at t = 1,000 days. Note that three of the four orbits start at the baseline point (z, y) = (1, 1) and end at a point for which z = 2, as demonstrated analytically in (33). The fourth orbit, associated with continuous tibolone treatment, ends at a different point for which z = 2E(Ti*), where \(Ti^{*}= \lim_{t \to\infty}Ti(t)\) (cf. (34)). The functions E(Ti) and Ti(t) and P Ca in the system (12) are given by Eqs. (6), (7) and (8), respectively, and parameter values are given by Table 1 for responders
In all four scenarios, after leaving the baseline point (z, y) = (1, 1) the orbit first moves to the right and up as the baseline changes due to disease progression. Then, at t start = 100 days, when the calcium and tibolone interventions kick in, the blue and the red orbit bifurcate from the disease progression orbit, the blue curve because of the calcium treatment and the red curve because of combined calcium and tibolone treatment. The latter moves sharply to the left, towards lower osteoclast-values and subsequently also down towards lower osteoblast-values. The green curve is the continuation of the disease progression orbit.
Because disease progression, as modelled by the function β(t) = β0 f(t), where \(f(t)=e^{-k_{{\rm estrogen}}t}\) (cf. Eqs. (5) and (14)), and calcium treatment modelled by the function P Ca(t) (cf. Eq. (13)), eventually come to a halt, the states of both scenarios (z, y) tend to a final limiting state \((z_\infty,y_\infty).\) Thus,
Equating the right-hand terms of the equations in the system (20) to zero and observing that by Eq. (14), f(t) → 0 as \(t \to \infty,\) we find that the final terminal point \((z_\infty,y_\infty)\) is given by
When tibolone treatment is terminated at t = 1,000 days, the corresponding red dashed orbit converges to the same terminal state, which suggests a symptomatic treatment effect in the bone cell level.
We conclude from Fig. 6 that \(S_\infty=z_\infty/y_\infty>1.\) Therefore, by Eq. (16) the BMD will keep decreasing over time.
On the other hand when tibolone treatment is continued indefinitely, the corresponding red solid orbit converges to a new terminal state \((z_\infty^{*},y_\infty^{*}).\) If Ti(t) → Ti* as \(t \to \infty,\) then we obtain for this state:
Thus, upon continued treatment, both z and y settle on lower homeostases. It is clear from Fig. 6 that now \(S_\infty^{*}=z_\infty^{*}/y_\infty^{*}<1, \) so that by Eq. (16) the BMD will steadily increase.
It is interesting to observe the difference in dynamics between onset and washout of effect. The onset proceeds in two stages. In the first stage (100–150 days) z drops rapidly while changes in y are relatively slow; in the second stage (150–1,000 days) both quantities decrease, but now it is y that drops faster. In contrast, washout consists of a gradual and comparable increase of z and y.
In order to capture these differences in cell dynamics through the use of corresponding biomarkers and to characterize the nature of the therapeutic intervention it is important to select an appropriate study design, i.e. washout design versus delayed-start design [24]. A washout design is better suited to evaluate these aspects for the current study as it allows to evaluate dynamics and the final state \((z_\infty,y_\infty)\) of the system following treatment cessation.
For the model we fitted in this paper, the elimination half-life of the active osteoblasts (y) is given by \(\ln(2)/k_B,\) which amounts to about 2 months. Note that it is independent of y or z. On the other hand, the elimination half-life of osteoclasts activity (z) is given by \(\ln(2)/\{D_A \pi_z(z)\},\) and thus depends on z. Specifically, as z increases, then so does π z (z) and hence the half-life shortens. In this study, the half-life for osteoclast activity in healthy individuals was estimated at 1 day. We conclude that washout of z or C proceeds much faster than that of y or B, as was seen in Fig. 6.
Rights and permissions
About this article
Cite this article
Post, T.M., Schmidt, S., Peletier, L.A. et al. Application of a mechanism-based disease systems model for osteoporosis to clinical data. J Pharmacokinet Pharmacodyn 40, 143–156 (2013). https://doi.org/10.1007/s10928-012-9294-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-012-9294-9