Abstract
Purpose
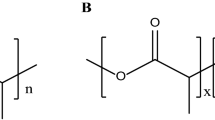
This study reports the incorporation of the antibiotics rifampin, doxycycline and clarithromycin in poly(styrene-co-methyl methacrylate films and their effect on biofilm prevention.
Background
Invasive procedures in patients such as surgical device, or intravenous or urinary catheter implantation, often results in complicated hospital-acquired nosocomial infections. Biofilm formation is essential to establish these infections on these devices and novel antibiotic delivery approaches are needed for more effective management.
Methods
The films were evaluated in vitro for drug release and for their ability to prevent biofilm formation by methicillin susceptible and methicillin resistant Staphylococcus aureus. Surface tension components, obtained from contact angle measurements, and the morphology of the films evaluated by scanning electron microscopy were also investigated.
Results
In this study, antibiotic-loaded methacrylic copolymer films that effectively released rifampin, clarithromycin and doxycycline for up to 21 days prevented biofilm formation when tested in an in vitro bioreactor model. These drug loaded copolymer films provided the advantage by coating materials with a novel surface that was unsuitable for resettling of biofilms once the antibiotic was dissolved from the polymer surface. A combination of rifampin and clarithromycin released from the polymer film provided >99.9% kill of an MRSA inoculate for up to 72 h.
Conclusion
Results showed that combining multiple drugs in copolymer films with unique surface properties, initial hydrophilicity and increase in roughness, can be an effective way to prevent biofilm formation.









Similar content being viewed by others
Abbreviations
- CLR:
-
Clarithromycin
- DIM:
-
Diiodomethane
- DOX:
-
Doxycycline
- EG:
-
Ethylene glycol
- GPC-MALLS-RI:
-
Gel permeation chromatography coupled to multi-angle laser light scattering and refractive index double detection
- HQ:
-
Hydroquinone
- KPS:
-
Potassium persulphate
- MMA:
-
Methyl methacrylate
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MSSA:
-
Methicillin-susceptible Staphylococcus aureus
- Poly(S-co-MMA):
-
Poly(styrene-co-methyl methacrylate)
- RIF:
-
Rifampicin
- S:
-
Styrene
- SDS:
-
Sodium dodecyl sulphate
- W A :
-
Work of adhesion
References
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284(5418):1318–22.
Veesenmeyer JL, Hauser AR, Lisboa T, Rello J. Pseudomonas aeruginosa virulence and therapy: evolving translational strategies. Crit Care Med. 2009;37(5):1777–86.
Donlan RM. Role of biofilms in antimicrobial resistance. ASAIO J. 2001;46(6):S47–52.
Gordon CA, Hodges NA, Marriott C. Antibiotic interaction and diffusion through alginate and exopolysaccharide of cystic fibrosis-derived Pseudomonas aeruginosa with piperacillin and tobramycin. J Antimicrob Chemother. 1988;22(5):667–74.
Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15(2):167–93.
Prabhakara R, Harro JM, Leid JG, Keegan AD, Prior ML, Shirtliff ME. Suppression of the inflammatory immune response prevents the development of chronic biofilm infection due to methicillin-resistant Staphylococcus aureus. Infect Immun. 2011;79(12):5010–8.
Darouiche R. Device-associated infections: a macroproblem that starts with microadherence. Clin Infect Dis. 2001;33(9):1567–72.
Raad I, Costerton JW, Sabharwal U, Sacilowski M, Anaissie E, Bodey GP. Ultrastructural analysis of indwelling vascular catheters: a quantitative relationship between luminal colonization and duration of placement. J Infect Dis. 1993;168(2):400–7.
Stoodley P, Ehrlich GD, Sedghizadeh PP, Hall-Stoodley L, Baratz ME, Altman DT, et al. Orthopaedic biofilm infections. Curr Orthop Pract. 2011;22(6):558–63.
Esfandiari N, Simchi A, Bagheri R. Size tuning of Ag-decorated TiO2 nanotube arrays for improved bactericidal capacity of orthopedic implants. J Biomed Mater Res A. (2013):In press.
Strydom SJ, Rose WE, Otto DP, Liebenberg W, de Villiers MM. Poly(amidoamine) dendrimer-mediated synthesis and stabilization of silver sulfonamide nanoparticles with increased antibacterial activity. Nanomedicine Nanotechnol Biol Med. 2013;9(1):85–93.
Tan H, Ma R, Lin C, Liu Z, Tang T. Quaternized chitosan as an antimicrobial agent: antimicrobial activity, mechanism of action and biomedical applications in orthopedics. Int J Mol Sci. 2013;14(1):1854–69.
Janjaroen D, Ling F, Monroy G, Derlon N, Mogenroth E, Boppart SA, et al. Roles of ionic strength and biofilm roughness on adhesion kinetics of Escherichia coli onto groundwater biofilm grown on PVC surfaces. Water Res. 2013;47(7):2531–42.
Lichter JA, Thompson MT, Delgadillo M, Nishikawa T, Rubner MF, van Vliet KJ. Substrata mechanical stiffness can regulate adhesion of viable bacteria. Biomacromolecules. 2008;9(6):1571–8.
Otto DP, Vosloo HCM, Liebenberg W, de Villiers MM. Effects of the cosurfactant 1-butanol and feed composition on nanoparticle properties produced by microemulsion copolymerization of styrene and methyl methacrylate. J Appl Polym Sci. 2008;107(6):3950–62.
Otto DP, Vosloo HCM, Liebenberg W, de Villiers MM. Development of microporous drug-releasing films cast from artificial nanosized latexes of poly(styrene-co-methyl methacrylate) or poly(styrene-co-ethyl methacrylate). Eur J Pharm Biopharm. 2008;69(3):1121–34.
USP. United States Pharmacopeia (USP-36-NF 31). The United States Pharmacopeial Convention, Rockville; 2014.
De Villiers MM. Anti-tuberculosis drugs. In: Cazes J, editor. Encyclopedia of chromatography, vol. 1. 3rd ed. Boca Raton: CRC Press; 2010. p. 118–23.
Balkende AR, van de Boogaard HJAP, Scholten M, Willard NP. Evaluation of different approaches to assess the surface tension of low-energy solids by means of contact angle measurements. Langmuir. 1998;14(20):5907–12.
Van Oss CJ, Good RJ, Chaudhury MK. Additive and nonadditive surface tension components and the interpretation of contact angles. Langmuir. 1988;4(4):884–91.
Van Oss CJ. Use of the combined Lifshitz-van der Waals and Lewis acid–base approaches in determining the apolar and polar contributions to surface and interfacial tensions and free energies. J Adhes Sci Technol. 2002;16(6):669–77.
Van Oss CJ, Good RJ. Prediction of the solubility of polar polymers by means of interfacial tension combining rules. Langmuir. 1992;8(12):2877–9.
Lam CNC, Lu JJ, Neumann AW. Measuring contact angle. In: Holmberg K, editor. Handbook of applied surface and colloid chemistry, vol. 2. Chichester: John Wiley & Sons; 2002. p. 251–80.
Agostinho AM, Hartman A, Lipp C, Parker AE, Stewart PS, James GA. An in vitro model for the growth and analysis of chronic wound MRSA biofilms. J Appl Microbiol. 2011;111(5):1275–82.
Briandet R, Herry JM, Bellon-Fontaine MN. etermination of the van der Waals, electron donor and electron acceptor surface tension components of static Gram-positive microbial biofilms. Coll Surf B. 2001;21(4):299–310.
Desrousseaux C, Sautou V, Descamps S, Traoré O. Modification of the surfaces of medical devices to prevent microbial adhesion and biofilm formation. J Hosp Infect. 2013;85(2):87–93.
Fan CW, Lee SC. Surface free energy effects in sputter-deposited WNx films. Mater Trans. 2007;48(9):2449–53.
Van Oss CJ. Hydrophobicity of biosurfaces – origin, quantitative determination and interaction energies. Coll Surf B. 1995;5(3–4):91–110.
Van Oss CJ. Interfacial forces in aqueous media. FL:CRC Press; 2006.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 34 kb)
Rights and permissions
About this article
Cite this article
Rose, W.E., Otto, D.P., Aucamp, M.E. et al. Prevention of Biofilm Formation by Methacrylate-Based Copolymer Films Loaded With Rifampin, Clarithromycin, Doxycycline Alone or in Combination. Pharm Res 32, 61–73 (2015). https://doi.org/10.1007/s11095-014-1444-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1444-x