Abstract
Background
Cabergoline is a recommended first-line dopamine agonist for prolactinoma treatment, which is withdrawable for some cases. However, the optimal withdrawal strategy and the accurate recurrence rate associated with cabergoline withdrawal remains uncertain.
Objective
To assess the current recurrence rate of hyperprolactinemia and possible favorable factors associated with cabergoline withdrawal in prolactinoma patients.
Method
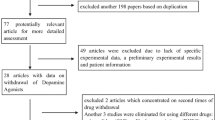
The databases of PubMed, EMBASE, and Web of Science were searched up to May 2014 to identify studies containing data of recurrent hyperprolactinemia in prolactinoma patients after cabergoline withdrawal. Meta-analysis, including sensitivity analysis, meta-regression analysis, and subgroup analysis were performed.
Results
When the patients who received cabergoline withdrawal were pooled, it was found that the hyperprolactinemia recurrence rate was 65 % by a random effects meta-analysis [95 % confidence interval 55–74 %]. In a random effects meta-regression adjusting for optimal withdrawal strategies, CAB dose reduced to the lowest level before withdrawal was associated with treatment success (p = 0.006), whereas CAB treatment longer than 2 years showed no trend of effect (p = 0.587). Patients who received the lowest CAB dose and presented a significant reduction in tumor size before withdrawal were more likely to achieve the best success (p < 0.001).
Conclusions
Our meta-analysis shows that hyperprolactinemia recurs after cabergoline withdrawal in a majority of patients. The probability of success favors patients who have achieved normoprolactinemia and considerable reduction in tumor size by low dose of cabergoline treatment. In addition, our study further suggests that a beneficial strategy is associated with tapering CAB dose before withdrawal but not with CAB treatment duration longer than 2 years.
Similar content being viewed by others
References
Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA, Wass JAH (2011) Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(2):273–288. doi:10.1210/jc.2010-1692
Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, Brue T, Cappabianca P, Colao A, Fahlbusch R, Fideleff H, Hadani M, Kelly P, Kleinberg D, Laws E, Marek J, Scanlon M, Sobrinho LG, Wass JAH, Giustina A (2006) Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol 65(2):265–273. doi:10.1111/j.1365-2265.2006.02562.x
Dekkers OM, Lagro J, Burman P, Jorgensen JO, Romijn JA, Pereira AM (2010) Recurrence of hyperprolactinemia after withdrawal of dopamine agonists: systematic review and meta-analysis. J Clin Endocrinol Metab 95(1):43–51. doi:10.1210/jc.2009-1238
Webster J, Piscitelli G, Polli A, Ferrari CI, Ismail I, Scanlon MF (1994) A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. Cabergoline Comparative Study Group. N Engl J Med 331(14):904–909. doi:10.1056/nejm199410063311403
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327(7414):557–560. doi:10.1136/bmj.327.7414.557
Watanabe S, Takano S, Akutsu H, Sato H, Matsumura A (2011) Prolactinoma treatment status in the cabergoline era. Neurol Surg 39(11):1045–1054
Giusti M, Porcella E, Carraro A, Cuttica M, Valenti S, Giordano G (1994) A cross-over study with the two novel dopaminergic drugs cabergoline and quinagolide in hyperprolactinemic patients. J Endocrinol Invest 17(1):51–57
Di Sarno A, Landi ML, Marzullo P, Di Somma C, Pivonello R, Cerbone G, Lombardi G, Colao A (2000) The effect of quinagolide and cabergoline, two selective dopamine receptor type 2 agonists, in the treatment of prolactinomas. Clin Endocrinol 53(1):53–60. doi:10.1046/j.1365-2265.2000.01016.x
Colao A, Di Sarno A, Cappabianca P, Di Somma C, Pivonello R, Lombardi G (2003) Withdrawal of long-term cabergoline therapy for tumoral and nontumoral hyperprolactinemia. N Engl J Med 349(21):2023–2033. doi:10.1056/NEJMoa022657
Bronstein MD (2006) Potential for long-term remission of microprolactinoma after withdrawal of dopamine-agonist therapy. Nat Clin Pract Endocrinol Metab 2(3):130–131. doi:10.1038/ncpendmet0135
Colao A, Di Sarno A, Guerra E, Pivonello R, Cappabianca P, Caranci F, Elefante A, Cavallo LM, Briganti F, Cirillo S, Lombardi G (2007) Predictors of remission of hyperprolactinaemia after long-term withdrawal of cabergoline therapy. Clin Endocrinol 67(3):426–433. doi:10.1111/j.1365-2265.2007.02905.x
Biswas M, Smith J, Jadon D, McEwan P, Rees DA, Evans LM, Scanlon MF, Davies JS (2005) Long-term remission following withdrawal of dopamine agonist therapy in subjects with microprolactinomas. Clin Endocrinol 63(1):26–31. doi:10.1111/j.1365-2265.2005.02293.x
Kwancharoen R, Auriemma RS, Yenokyan G, Wand GS, Colao A, Salvatori R (2013) Second attempt to withdraw cabergoline in prolactinomas: a pilot study. Pituitary. doi:10.1007/s11102-013-0525-x
Anagnostis P, Adamidou F, Polyzos SA, Efstathiadou Z, Karathanassi E, Kita M (2012) Long term follow-up of patients with prolactinomas and outcome of dopamine agonist withdrawal: a single center experience. Pituitary 15(1):25–29. doi:10.1007/s11102-011-0303-6
Barber TM, Kenkre J, Garnett C, Scott RV, Byrne JV, Wass JAH (2011) Recurrence of hyperprolactinaemia following discontinuation of dopamine agonist therapy in patients with prolactinoma occurs commonly especially in macroprolactinoma. Clin Endocrinol 75(6):819–824. doi:10.1111/j.1365-2265.2011.04136.x
Huda MSB, Athauda NB, Teh MM, Carroll PV, Powrie JK (2010) Factors determining the remission of microprolactinomas after dopamine agonist withdrawal. Clin Endocrinol 72(4):507–511. doi:10.1111/j.1365-2265.2009.03657.x
Buyukbayrak EE, Karsidag AYK, Kars B, Balcik O, Pirimoglu M, Unal O, Turan C (2010) Effectiveness of short-term maintenance treatment with cabergoline in microadenoma-related and idiopathic hyperprolactinemia. Arch Gynecol Obstet 282(5):561–566. doi:10.1007/s00404-010-1562-6
Kharlip J, Salvatori R, Yenokyan G, Wand GS (2009) Recurrence of hyperprolactinemia after withdrawal of long-term cabergoline therapy. J Clin Endocrinol Metab 94(7):2428–2436. doi:10.1210/jc.2008-2103
Cannavo S, Curto L, Squadrito S, Almoto B, Vieni A, Trimarchi F (1999) Cabergoline: a first-choice treatment in patients with previously untreated prolactin-secreting pituitary adenoma. J Endocrinol Invest 22(5):354–359
Muratori M, Arosio M, Gambino G, Romano C, Biella O, Faglia G (1997) Use of cabergoline in the long-term treatment of hyperprolactinemic and acromegalic patients. J Endocrinol Invest 20(9):537–546
Ferrari C, Paracchi A, Mattei AM, de Vincentiis S, D’Alberton A, Crosignani P (1992) Cabergoline in the long-term therapy of hyperprolactinemic disorders. Acta Endocrinol 126(6):489–494
Ben-Jonathan N, Hnasko R (2001) Dopamine as a prolactin (PRL) inhibitor. Endocr Rev 22(6):724–763. doi:10.1210/er.22.6.724
Wang F, Gao H, Li C, Bai J, Lu R, Cao L, Wu Y, Hong L, Wu Y, Lan X, Zhang Y (2014) Low levels of PRB3 mRNA are associated with dopamine-agonist resistance and tumor recurrence in prolactinomas. J Neurooncol 116(1):83–88. doi:10.1007/s11060-013-1276-2
Popescu MN, Ionescu E, Iovanescu LC, Cotoi BV, Popescu AI, Ganescu AE, Glodeanu A, Geormaneanu C, Moraru A, Patrascu A (2013) Clinical aggression of prolactinomas: correlations with invasion and recurrence. Rom J Morphol Embryol 54(4):1075–1080
Acknowledgments
The authors sincerely thank Prof. Rufu Xu (Evidence Based Medicine and Epidemiology Center, Third Military University, Chongqing, China) for helpful comments on the statistical methods.
Conflict of interest
No conflict of interest exits in the submission of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hu, J., Zheng, X., Zhang, W. et al. Current drug withdrawal strategy in prolactinoma patients treated with cabergoline: a systematic review and meta-analysis. Pituitary 18, 745–751 (2015). https://doi.org/10.1007/s11102-014-0617-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-014-0617-2