Abstract
This paper uses a mixed effects model to examine the temporal variation of cost efficiency in Switzerland’s general hospitals. The variations in total costs, the number of empty beds and the length of hospital stays are analyzed using financial data from a sample of 168 hospitals operating from 1998 to 2003, as well as hospitalization records disaggregated to Diagnosis Related Groups. Individual intercepts and random coefficients are used to account for the unobserved time-invariant heterogeneity and the differences in temporal patterns across hospitals and DRG categories. The analysis illustrates the usefulness of mixed models to account for unobserved factors such as quality, with a relatively weak assumption that their temporal variations, rather than their initial levels, be uncorrelated with efficiency changes. The results indicate that hospitals have adopted measures to curtail hospitalizations and reduce empty beds. The extent and effectiveness of these measures vary significantly across individual hospitals. However, there is no evidence in favor of a particular ownership type or subsidization regime. While the link between reduction rates of empty beds and gains in cost-efficiency is statistically significant, the expected association between shortening hospital stays and cost-efficiency cannot be clearly established in the data.



Similar content being viewed by others
Notes
DRG is a system of classification based on the required hospital resources. DRG codes are assigned by patented computer programs using information on diagnoses, complications/comorbidities and procedures as well as patient’s age and gender. DRGs have been first used by Medicare (the US health insurance program for the elderly) in its case-based reimbursement rules, known as Prospective Payment System. Hospitalization costs of each DRG are usually estimated by statistical analysis of large samples of similar cases. In Switzerland, this information is provided by ‘APDRG Suisse,’ a non-profit association comprising of DRG users throughout the country.
The overall inefficiency is usually over-stated should the fixed effects be interpreted as inefficiency as in Schmidt and Sickles (1984), and understated if they are considered as external factors unrelated to cost-efficiency as in Polachek and Yoon (1996) and Greene (2005). Farsi and Filippini (2004) show how the efficiency differences could reach implausible levels in the former case. As for the latter cases, where inefficiency is identified as an additional skewed stochastic term, this author’s experience suggests that the available algorithms have a high risk of producing unreliable estimates of the fixed effects. Farsi et al. (2005) propose a solution around the incidental parameters problem by combining Mundlak’s (1978) specification to Greene’s (2005) random effects model.
Sickles’ (2005) general framework can be applied with fixed effects for temporal changes as well, however at a considerable loss of the model’s degrees of freedom. For instance in a quadratic form for temporal variations would require 3 fixed parameters for each hospital, which might create a plausibility problem for short and medium panels.
The adopted cost function is similar to the specification used in Farsi and Filippini (2008), with the difference that here because of the presence of individual fixed effects, a number of variables that are time-invariant or practically stable over time are excluded. Similarly, the choice of Cobb–Douglas from as opposed to flexible forms such as translog is motivated by the trade-off between flexibility and the model’s degrees of freedom, especially restricted here because of fixed effects. Moreover, we do not impose the restriction of linear homogeneity in input prices, because as we see later in the data section, the included input prices do not cover all the input factors.
These omitted characteristics could include hospital’s specialization level, quality of service, and also case mix severity to the extent that these factors depend on hospital location and long-term factors such as medical staff and reputation. Concerning the case mix it should be noted that the DRG adjustment (used in the specification) is only an imperfect measure of severity, thus the within-DRG variations across hospitals remain unobserved.
In line with the Rogowski and Newhouse, we assume that this effect is a result of ‘indirect’ costs of training medical students rather than hospital’s inefficiency suggested by Simmer et al. (1991).
I use the word excess in a narrow sense, to denote the temporal changes that cannot be explained by the changes in variables included in the model.
Kruskal–Wallis test is a non-parametric test that has been often used in frontier analysis (Singh and Coelli 2001; Grosskopf et al. 2001). An alternative approach would be to include type indicators as interaction terms in the regression models and test their significance. I preferred the non-parametric test because of its robustness to distribution assumptions.
Specialized clinics, rehabilitation centers and other long-term facilities are excluded.
The original data base includes about a million records by DRG and admission categories.
Such an assumption might bias the estimated differences across different ownership types. Assuming a sudden structural change in parameters after the conversion year is also unrealistic, because the ownership changes are usually long processes and the converting hospitals might undergo gradual changes prior to conversion. See Farsi (2004) for some evidence on this issue.
A series of probit analyses and t-tests indicated that the excluded observations are not related to an obvious selection of hospitals regarding size (number of beds) or ownership/subsidy types. In any case, given the presence of fixed effects in the model sample selection is not expected to affect the results.
The DRGs described by ‘other’ or ‘non-specified’ were not considered.
About 1,600 severe outliers with average LOS greater than 36.4 days (three times the inter-quartile range) were excluded.
The average cost weight for any given hospital-year is calculated form the medical data, by dividing the weighted sum of the number of admissions (with weights being the DRG cost weights according to Swiss AP-DRG version 4.0), by the total number of cases. This provides a single measure of inpatient services in contrast with Brown’s (2003) approach with multiple groups with similar DRG weights.
In any case the focus of this study is on efficiency estimates and the endogeneity bias in the price coefficients is of secondary importance. The possible impact of endogeneity on efficiency estimates is an open question that depends on whether a company’s intentions in changing their inputs are interpreted as a quality-neutral effort to improve efficiency or as an intentional change in the quality of inputs. In the latter case, by including the input prices we can provide more realistic values of efficiency adjusted for quality differences, even though the price coefficients are obviously biased.
The presence of fixed effects can also explain the lack of statistical significance for some of the variables. Compare for instance with the estimation results reported in Farsi and Filippini (2008).
This can also be explained by the mechanical negative relationship between admissions and the number of empty beds. Such a relationship might create endogeneity bias in the hospital-specific estimates of growth in excess capacity. However, a preliminary analysis showed that excluding the number of admissions from the model does not cause much difference.
An additional analysis of LOS aggregated at the hospital level (available upon request), indicates an average decrease of about 3.3% per year in the length of hospitalizations, suggesting an upward aggregation bias. All other coefficients are very similar to those reported in Table 3.
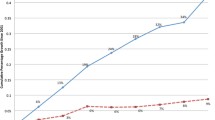
Interpreting the average trends without statistical correlations, could be misleading. For instance, as we see later the excess costs and excess LOS show a positive correlation in the hospital group with efficiency loss, which might seem contradictory to the opposing trends in costs and LOS in Fig. 3. However, a positive correlation does not necessarily imply similar average trends. Rather, it implies that the hospitals that are located above the LOS curve are likely to be above the excess capacity curve as well. Another interesting point is the close coincidence of LOS and cost curves in Fig. 2, but the lack of statistically significant correlation between the two measures in that group (as we see later).
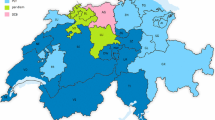
In addition to ownership types, we studied the differences among five typologies based on size and specialization (SFSO 2001), and five geographical regions (details available upon request). Virtually in all cases, the differences across groups were statistically insignificant. The only exception was canton Ticino (southern region) with greater gains in cost efficiency compared to four other regions. Nevertheless, further tests suggested no significant difference between Ticino and six other cantons (BS, BL, FR, GE, NE and VS), out of 26 Swiss cantons.
This result was also confirmed by a series of correlation analyses within various types of hospitals by ownership/subsidy. Excepting a few cases with significant correlations in levels, the rank correlation remained statistically insignificant across all sub-samples.
References
Aigner D, Lovell CAK, Schmidt P (1977) Formulation and estimation of stochastic frontier production function models. J Econom 6:21–37. doi:10.1016/0304-4076(77)90052-5
Alvarez AM, Schmidt P (2006) Is skill more important than luck in explaining fish catches? J Prod Anal 26(1):15–25. doi:10.1007/s11123-006-0002-x
APDRG Suisse (2003) Cost Weights version 4.1. Institut de Santé et d’Economie Prilly, Switzerland, available at: www.apdrgsuisse.ch
Battese GE, Coelli T (1992) Frontier production functions, technical efficiency and panel data: with application to paddy farmers in India. J Prod Anal 3:153–169. doi:10.1007/BF00158774
Bradford WD et al (2001) Stochastic frontier estimation of cost models within the hospital. Rev Econ Stat 83(2):302–309. doi:10.1162/00346530151143833
Breyer F (1987) The specification of a hospital cost function: a comment on the recent literature. J Health Econ 6:147–157. doi:10.1016/0167-6296(87)90004-X
Brown HS (2003) Managed care and technical efficiency. Health Econ 12(2):149–158. doi:10.1002/hec.712
Carey K (1997) A panel data design for estimation of hospital cost functions. Rev Econ Stat 79(2):443–453. doi:10.1162/003465300556850
Carey K (2000) Hospital cost containment and length of stay: an econometric analysis. Southern Econ J 67(2):363–380. doi:10.2307/1061475
Cornwell Ch, Schmidt P, Sickles RC (1990) Production frontiers with cross-sectional and time-series variation in efficiency levels. J Econom 46:185–200. doi:10.1016/0304-4076(90)90054-W
Deily ME, McKay NL (2006) Cost inefficiency and mortality rates in Florida hospitals. Health Econ 15(4):419–431. doi:10.1002/hec.1078
Farsi M (2004) Changes in hospital quality after conversion in ownership status. Int J Health Care Finance Econ 4(3):211–230. doi:10.1023/B:IHFE.0000036047.66483.46
Farsi M, Filippini M (2004) Regulation and measuring cost efficiency with panel data models application to electricity distribution utilities. Rev Ind Organ 25(1):1–19. doi:10.1023/B:REIO.0000040474.83556.54
Farsi M, Filippini M (2006) An analysis of efficiency and productivity in Swiss hospitals. Schweiz Z Volkswirtsch Stat 142(1):1–37
Farsi M, Filippini M (2008) Effects of Subsidization and Teaching Activities on Hospital Costs in Switzerland. Health Econ 17(3):335–350
Farsi M, Filippini M, Kuenzle M (2005) Unobserved heterogeneity in stochastic cost frontier models: an application to Swiss nursing homes. Appl Econ 37:2127–2141. doi:10.1080/00036840500293201
Folland ST, Hofler RA (2001) How reliable are hospital efficiency estimates? Exploiting the dual to homothetic production. Health Econ 10:683–698. doi:10.1002/hec.600
Gaynor M, Anderson GF (1995) Uncertain demand, the structure of hospital costs, and the cost of empty hospital beds. J Health Econ 14:291–317. doi:10.1016/0167-6296(95)00004-2
Greene W (2005) Fixed and random effects in stochastic frontier models. J Prod Anal 23(1):7–32. doi:10.1007/s11123-004-8545-1
Grosskopf S, Margaritis D, Valdmanis V (2001) Comparing teaching and non-teaching hospitals: a frontier approach (teaching vs. non-teaching hospitals). Health Care Manage Sci 4:83–90. doi:10.1023/A:1011449425940
Heshmati A (2002) Productivity measurement in Swedish departments of gynecology and obstetrics. Struct Change Dynam 13:315–336. doi:10.1016/S0954-349X(01)00040-6
Hollingsworth B, Street A (2006) The market for efficiency analysis of health care organisations (editorial). Health Econ 15(11):1055–1059. doi:10.1002/hec.1169
Jacobs R, Dawson D (2003) Hospital efficiency targets. Health Econ 12(8):669–684. doi:10.1002/hec.758
Jacobs R, Smith PC, Street A (2006) Measuring efficiency in health care: analytic techniques and health policy. Cambridge University Press
Kneip A, Sickles RC, Song WH (2003) On estimating a mixed effects model with applications to the US banking industry. Rice University, Mimeo
Kruskal WH, Wallis WA (1952) Use of ranks in one-criterion variance analysis. J Am Stat Assoc 47:583–621. doi:10.2307/2280779
Kumbhakar SC (1990) Production frontiers and panel data, and time varying technical inefficiency. J Econom 46:201–211. doi:10.1016/0304-4076(90)90055-X
Kumbhakar SC (1991) Estimation of technical inefficiency in panel data models with firm- and time-specific effects. Econ Lett 36:43–48. doi:10.1016/0165-1765(91)90053-N
Lee Y, Schmidt P (1993) A production frontier model; with flexible temporal variation in technical efficiency. In: Fried H, Lovell K, Schmidt S (eds) The measurement of productive efficiency. Oxford University Press, New York
Linna M (1998) Measuring hospital cost efficiency with panel data models. Health Econ 7:415–427. doi :10.1002/(SICI)1099-1050(199808)7:5<415::AID-HEC357>3.0.CO;2-9
Liu C, Laporte A, Ferguson B (2007) The Quantile Regression Approach to Efficiency Measurement: Insights from Monte Carlo Simulations, HEDG Working Paper 07/14, Department of Economics, University of York
Martin S, Smith P (1996) Explaining variations in inpatient length of stay in the National Health Service. J Health Econ 15:279–304. doi:10.1016/0167-6296(96)00003-3
Meeusen W, van den Broeck J (1977) Efficiency estimation from Cobb–Douglas production functions with composed error. Int Econ Rev 18(2):435–444. doi:10.2307/2525757
Mundlak Y (1978) On the pooling of time series and cross section data. Econometrica 64(1):69–85. doi:10.2307/1913646
Newhouse JP (1994) Frontier estimation: how useful a tool for health economics. J Health Econ 13:317–322. doi:10.1016/0167-6296(94)90030-2
Polachek S, Yoon B (1996) Panel estimates of a two-tiered earnings frontier. J Appl Econom 11:169–178. doi :10.1002/(SICI)1099-1255(199603)11:2<169::AID-JAE373>3.0.CO;2-#
Rosko MD (2001) Cost efficiency of US hospitals: a stochastic frontier approach. Health Econ 10:539–551. doi:10.1002/hec.607
Rogowski JA, Newhouse JP (1992) Estimating the indirect costs of teaching. J Health Econ 11:153–171. doi:10.1016/0167-6296(92)90032-V
Schmidt P, Sickles RC (1984) Production frontiers and panel data. J Bus Econ Stat 2:367–374. doi:10.2307/1391278
Scuffham PA, Devlin NJ, Jaforullah M (1996) The structure of costs and production in New Zealand public hospitals: an application of the transcendental logarithmic variable cost function. Appl Econ 28:75–85. doi:10.1080/00036849600000010
SFSO (1997a) Statistiques des établissements de santé (soins intra-muros), Statistique des hôpitaux, Conception détaillée, Déc. 1997 (in French). Swiss Federal Statistical Office, Neuchâtel, Switzerland, www.statistik.admin.ch
SFSO (1997b) Statistiques des établissements de santé (soins intra-muros), Statistique médicale des hôpitaux, Conception détaillée 1997 (in French). Swiss Federal Statistical Office, Neuchâtel, Switzerland, www.statistik.admin.ch
SFSO (2001) Statistiques des établissements de santé (soins intra-muros), Typologie des hôpitaux (in French). Swiss Federal Statistical Office, Neuchâtel, Switzerland, www.statistik.admin.ch
Sickles RC (2005) Panel estimators and the identification of firm-specific efficiency levels in parametric, semiparametric and nonparametric settings. J Econom 126(2):305–334. doi:10.1016/j.jeconom.2004.05.004
Simmer T, Nerenz D, Rutt W, Newcomb C, Benfer C (1991) A randomized, controlled trial of an attending staff service in general internal medicine. Medical Care 29(7):31–40
Singh S, Coelli T (2001) Performance of dairy plants in the cooperative and private sectors in India. Ann Public Coop Econ 72(4):453–479. doi:10.1111/1467-8292.00178
Skinner J (1994) What do stochastic frontier cost functions tell us about inefficiency? J Health Econ 13:323–328. doi:10.1016/0167-6296(94)90031-0
Steinmann L, Zweifel P (2003) On the (in)efficiency of Swiss hospitals. Appl Econ 35:361–370. doi:10.1080/00036840210167183
Street A (2003) How much confidence should we place in efficiency estimates? Health Econ 12:895–907. doi:10.1002/hec.773
Vita MG (1990) Exploring hospital production relationships with flexible functional forms. J Health Econ 9:1–21. doi:10.1016/0167-6296(90)90038-5
Vitaliano D, Toren M (1996) Hospital cost and efficiency in a regime of stringent regulation. East Econ J 22:161–184
Wagstaff A, Lopez G (1995) Hospital costs in Catalonia: a stochastic frontier analysis. Appl Econ Lett 3:471–474. doi:10.1080/758540809
Worthington AC (2004) Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Med Care Res Rev 61(2):135–170. doi:10.1177/1077558704263796
Zuckerman S, Hadley J, Iezzoni L (1994) Measuring hospital efficiency with frontier cost functions. J Health Econ 13:255–280. doi:10.1016/0167-6296(94)90027-2
Acknowledgements
This research has been partly financed by the Swiss National Science Foundation through research grant 100012-108288, which is gratefully acknowledged. I am also grateful to the Swiss Federal Statistical Office for providing the data and to Massimo Filippini, William Greene, Martin Jakob and André Meister for their support and many helpful comments. I benefited from helpful suggestions of two anonymous reviewers and this journal’s editor which is greatly appreciated. I am solely responsible for the expressed views as well as any remaining errors and omissions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farsi, M. The temporal variation of cost-efficiency in Switzerland’s hospitals: an application of mixed models. J Prod Anal 30, 155–168 (2008). https://doi.org/10.1007/s11123-008-0105-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11123-008-0105-7