Abstract
Purpose
This single-blinded, randomized, controlled pilot study aimed to investigate whether there is a difference between nasal and oronasal masks in therapeutic continuous positive airway pressure (CPAP) requirement, residual disease, or leak when treating obstructive sleep apnea (OSA) and if differences were related to measures of upper airway size.
Methods
Patients with severe OSA currently using CPAP at ≥4 h/night with a nasal mask were examined (including Mallampati scale, incisal relationship, and mandibular protrusion) and then randomized to receive auto-positive airway pressure (PAP) or fixed CPAP at a manually titrated pressure for 1 week each at home, with immediate crossover. Within each week, a nasal mask and two oronasal masks were to be used for two or three nights each in random order. Data were downloaded from the device.
Results
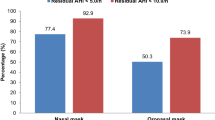
Twelve patients completed the trial (mean ± SD AHI 59.8 ± 28.6 events/h; CPAP 11.1 ± 3.2 cmH2O; BMI 37.7 ± 5.0 kg/m2). During auto-PAP, the median 95th percentile pressure delivered with all masks was within 0.5 cmH2O (p > 0.05). During CPAP, median residual AHI was 0.61 (IQR = 1.18) for the nasal mask, 1.70 (IQR = 4.04) for oronasal mask 1, and 2.48 (IQR = 3.74) for oronasal mask 2 (p = 0.03). The 95th percentile leak was lowest with the nasal mask during both CPAP and auto-PAP (both p < 0.01). Differences in pressure or residual disease were not related to measures of upper airway shape or body habitus.
Conclusions
In obese OSA patients changing from a nasal to oronasal mask increased leak and residual AHI but did not affect the therapeutic pressure requirement. The findings of the current study highlight mask leak as the major difficulty in the use of oronasal masks.



Similar content being viewed by others
References
Mulgrew AT, Ryan CF, Fleetham JA, Cheema R, Fox N, Koehoorn M, Fitzgerald JM, Marra C, Ayas NT (2007) The impact of obstructive sleep apnea and daytime sleepiness on work limitation. Sleep Med 9(1):42–53
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
Nowak M, Kornhuber J, Meyrer R (2006) Daytime impairment and neurodegeneration in OSAS. Sleep 29(12):1521–1530
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol 52(8):686–717
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6(8):e1000132
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(8):1079–1085
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Svensson M, Holmstrom M, Broman JE, Lindberg E (2006) Can anatomical and functional features in the upper airways predict sleep apnea? A population-based study in females. Acta Otolaryngol 126(6):613–620
Vos W, De Backer J, Devolder A, Vanderveken O, Verhulst S, Salgado R, Germonpre P, Partoens B, Wuyts F, Parizel P, De Backer W (2007) Correlation between severity of sleep apnea and upper airway morphology based on advanced anatomical and functional imaging. J Biomech 40(10):2207–2213
Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, Nishino T (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol 82(4):1319–1326
Akashiba T, Kosaka N, Yamamoto H, Ito D, Saito O, Horie T (2001) Optimal continuous positive airway pressure in patients with obstructive sleep apnoea: role of craniofacial structure. Respir Med 95(5):393–397
Chai CL, Pathinathan A, Smith B (2006) Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev (4):CD005308
Mortimore IL, Whittle AT, Douglas NJ (1998) Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax 53(4):290–292
Prosise GL, Berry RB (1994) Oral–nasal continuous positive airway pressure as a treatment for obstructive sleep apnea. Chest 106(1):180–186
Beecroft J, Zanon S, Lukic D, Hanly P (2003) Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest 124(6):2200–2208
Teo M, Amis T, Lee S, Falland K, Lambert S, Wheatley J (2011) Equivalence of nasal and oronasal masks during initial CPAP titration for obstructive sleep apnea syndrome. Sleep 34(7):951–955
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Dimsdale JE, Loredo JS, Profant J (2000) Effect of continuous positive airway pressure on blood pressure: a placebo trial. Hypertension 35(1 Pt 1):144–147
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques, and scoring systems for sleep stages of human subjects. UCLA Brain Information Service/Brain Research Institute, Los Angeles
American Sleep Disorders Association (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force. Sleep 15(2):173–184
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Nuckton TJ, Glidden DV, Browner WS, Claman DM (2006) Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep 29(7):903–908
Schulz KF, Grimes DA (2002) Generation of allocation sequences in randomised trials: chance, not choice. Lancet 359(9305):515–519
Coller D, Stanley D, Parthasarathy S (2005) Effect of air leak on the performance of auto-PAP devices: a bench study. Sleep Breath 9(4):167–175
Valentin A, Subramanian S, Quan SF, Berry RB, Parthasarathy S (2011) Air leak is associated with poor adherence to autoPAP therapy. Sleep 34(6):801–806
Baltzan MA, Dabrusin R, Garcia-Asensi A, Sully JL, Parenteau M, Tansimat G, Kassissia I, Wolkove N (2011) Leak profile inspection during nasal continuous positive airway pressure. Respir Care 56(5):591–595
Oksenberg A, Silverberg DS, Arons E, Radwan H (1999) The sleep supine position has a major effect on optimal nasal continuous positive airway pressure: relationship with rapid eye movements and non-rapid eye movements sleep, body mass index, respiratory disturbance index, and age. Chest 116(4):1000–1006
Acknowledgements
We wish to thank all participants who consented to the study and we are grateful to Dr. Hugh Trengrove for his insight into the measures of upper airway shape.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bakker, J.P., Neill, A.M. & Campbell, A.J. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath 16, 709–716 (2012). https://doi.org/10.1007/s11325-011-0564-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0564-3