Abstract
Purpose
Recently, we noticed a considerable development in alleviating problems related to positive airway pressure (PAP) masks. In this study, we report on the initial PAP mask acceptance rates and the effects of mask switching on mask-related symptoms.
Methods
We prospectively collected all cases of mask switching in our sleep unit for a period of 14 months. At the time of the study, we used ResMed™ CPAP devices and masks. Mask switching was defined as replacing a mask used for at least 1 day with another type of mask. Changing to a different size but keeping the same type of mask did not count as mask switching. Switching outcomes were considered failed if the initial problem persisted or reappeared during the year that followed switching.
Results
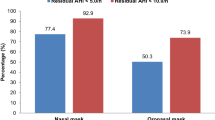
Our patient pool was 2768. We recorded 343 cases of mask switching among 267 patients. Of the 566 patients who began new PAP therapy, 108 (39 women) had switched masks, yielding an initial mask acceptance rate of 81 %.
The reason for switching was poor-fit/uncomfortable mask in 39 %, leak-related in 30 %, outdated model in 25 %, and nasal stuffiness in 6 % of cases; mask switching resolved these problems in 61 %.
Mask switching occurred significantly (p = 0.037) more often in women and in new PAP users. The odds ratio for abandoning PAP therapy within 1 year after mask switching was 7.2 times higher (interval 4.7–11.1) than not switching masks.
Conclusion
The initial PAP mask acceptance rate was high. Patients who switched their masks are at greater risk for abandoning PAP therapy.
Similar content being viewed by others
References
Loube DI, Gay PC, Strohl KP, et al. (1999) Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest1 115:863–866
Kushida CA, Littner MR, Hirshkowitz M, et al. (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29:375–380
Mysliwiec V, Gill J, Matsangas P, Baxter T, Barr T, Roth BJ (2015) IGF-1: a potential biomarker for efficacy of sleep improvement with automatic airway pressure therapy for obstructive sleep apnea? Sleep Breath. doi:10.1007/s11325-015-1142-x
Bachour A, Vitikainen P, Virkkula P, Maasilta P (2013) CPAP interface: satisfaction and side effects. Sleep and Breathing 17:667–672
Massie CA, Hart RW (2003) Clinical outcomes related to interface type in patients with obstructive sleep apnea/hypopnea syndrome who are using continuous positive airway pressure. Chest 123:1112–1118
Kakkar RK, Berry RB (2007) Positive airway pressure treatment for obstructive sleep apnea. Chest 132:1057–1072
Pepin JL, Leger P, Veale D, Langevin B, Robert D, Lévy P (1995) Side effects of nasal continuous positive airway pressure in sleep apnea syndrome: study of 193 patients in two French sleep centers. Chest 107:375–381
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5:173–178
Berry RB (2000) Improving CPAP compliance—man more than machine. Sleep Med 1:175–178
Silva RS, Truksinas V, de Mello-Fujita L, Truksinas E, Zanin LK, Pinto MC, de Paula MS, Skomro RP, Bittencourt LR, Tufik S (2008) An orientation session improves objective sleep quality and mask acceptance during positive airway pressure titration. Sleep Breath 12:85–89
Bachour A, Virkkala J, Maasilta P (2007) AutoCPAP initiation at home: optimal trial duration and cost-effectiveness. Sleep Med 8:704–710
Ryan S, Garvey JF, Swan V, Behan R, McNicholas WT (2011) Nasal pillows as an alternative interface in patients with obstructive sleep apnoea syndrome initiating continuous positive airway pressure therapy. J Sleep Res 20:367–373
Kreivi HR, Virkkula P, Lehto J, Brander P (2010) Frequency of upper airway symptoms before and during continuous positive airway pressure treatment in patients with obstructive sleep apnea syndrome. Respiration 80:488–494
Beecroft J, Zanon S, Lukic D, Hanly P (2003) Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest 124:2200–2208
Acknowledgments
This study took place at the Helsinki University Hospital and was funded by the Helsinki University Special Fund (V1016SK001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Bachour, A., Vitikainen, P. & Maasilta, P. Rates of initial acceptance of PAP masks and outcomes of mask switching. Sleep Breath 20, 733–738 (2016). https://doi.org/10.1007/s11325-015-1292-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1292-x