Abstract
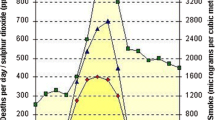
Few researches have been investigated on the effects of ambient air pollutants from coal combustion on acute exacerbation of chronic obstructive pulmonary disease (AECOPD) hospitalizations. The whole time series was split into heating season and non-heating season. We used a quasi-Poisson generalized linear regression model combined with distributed lag non-linear models (DLNMs) to estimate the relative cumulative risk and calculate the air pollutant hospitalization burden of AECOPD for lag 0–7 days in heating season and non-heating season. There were higher PM2.5, PM10, NO2, SO2, and CO concentrations in heating seasons than non-heating season in Shijiazhuang; however, O3 was higher in non-heating season than heating season. The AECOPD-associated relative cumulative risks for PM2.5, PM10, NO2, and SO2 for lag 0–7 days were significantly positively associated with hospitalization in heating and non-heating season; we found that the cumulative relative risk of NO2 was the greatest in every 1 unit of air pollutants during the heating season and the cumulative relative risk of SO2 was the greatest during the non-heating season. The results showed that 17.8%, 12.9%, 1.7%, 16.7%, and 10.5% of AECOPD hospitalizations could be attributable to PM2.5, PM10, SO2, NO2, and CO exposure in heating season, respectively. However, the results showed that 19.5%, 22.4%, 15%, 8.3%, and 10.4% of AECOPD hospitalizations could be attributable to PM2.5, PM10, SO2, NO2, and O3 exposure in non-heating season, respectively. The attributable burden of AECOPD hospitalization in heating season and non-heating season are different. PM2.5, PM10, NO2, and CO are the main factors of heating season, while PM10, PM2.5, SO2, and O3 are the main factors of non-heating season. In conclusions, the centralized heating can change the influence of attributable risk. When government departments formulate interventions to reduce the risk of acute hospitalization of chronic obstructive pulmonary disease (COPD), the influence of heating on disease burden should be considered.


Similar content being viewed by others
References
Almagro P, Calbo E, Ochoa de Echaguen A, Barreiro B, Quintana S, Heredia JL, Garau J (2002) Mortality after hospitalization for COPD. Chest 121:1441–1448
Anderson HR, Spix C, Medina S, Schouten JP, Castellsague J, Rossi G, Zmirou D, Touloumi G, Wojtyniak B, Ponka A, Bacharova L, Schwartz J, Katsouyanni K (1997) Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur Respir J 10:1064–1071
Anonymous (2017) Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med 5:691–706
Bayram H, Sapsford RJ, Abdelaziz MM, Khair OA (2001) Effect of ozone and nitrogen dioxide on the release of proinflammatory mediators from bronchial epithelial cells of nonatopic nonasthmatic subjects and atopic asthmatic patients in vitro. J Allergy Clin Immunol 107:287–294
Burnett RT, Brook JR, Yung WT, Dales RE, Krewski D (1997) Association between ozone and hospitalization for respiratory diseases in 16 Canadian cities. Environ Res 72:24–31
Chen KS, Ho YT, Lai CH, Tsai YA, Chen SJ (2004) Trends in concentration of ground-level ozone and meteorological conditions during high ozone episodes in the Kao-Ping Airshed, Taiwan. J Air Waste Manage Assoc 54:36–48
Cheng MH, Chiu HF, Yang CY (2015) Coarse particulate air pollution associated with increased risk of hospital admissions for respiratory diseases in a tropical city, Kaohsiung, Taiwan. Int J Environ Res Public Health 12:13053–13068
Di Q, Dai L, Wang Y, Zanobetti A, Choirat C, Schwartz JD, Dominici F (2017) Association of short-term exposure to air pollution with mortality in older adults. JAMA 318:2446–2456
Ding PH, Wang GS, Guo YL, Chang SC, Wan GH (2017) Urban air pollution and meteorological factors affect emergency department visits of elderly patients with chronic obstructive pulmonary disease in Taiwan. Environ Pollut 224:751–758
Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA (2002) Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 57:847–852
Ferrari U, Exner T, Wanka ER, Bergemann C, Meyer-Arnek J, Hildenbrand B, Tufman A, Heumann C, Huber RM, Bittner M, Fischer R (2012) Influence of air pressure, humidity, solar radiation, temperature, and wind speed on ambulatory visits due to chronic obstructive pulmonary disease in Bavaria, Germany. Int J Biometeorol 56:137–143
Gao N, Li C, Ji J, Yang Y, Wang S, Tian X, Xu KF (2019) Short-term effects of ambient air pollution on chronic obstructive pulmonary disease admissions in Beijing, China (2013-2017). Int J Chron Obstruct Pulmon Dis 14:297–309
Gasparrini A, Leone M (2014) Attributable risk from distributed lag models. BMC Med Res Methodol 14:55
Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, Zanobetti A, Schwartz JD, Tobias A, Leone M, Tong S, Honda Y, Kim H, Armstrong BG (2015) Temporal variation in heat-mortality associations: a multicountry study. Environ Health Perspect 123:1200–1207
Gasparrini A, Scheipl F, Armstrong B, Kenward MG (2017) A penalized framework for distributed lag non-linear models. Biometrics 73:938–948
Gharehchahi E, Mahvi AH, Amini H, Nabizadeh R, Akhlaghi AA, Shamsipour M, Yunesian M (2013) Health impact assessment of air pollution in Shiraz, Iran: a two-part study. J Environ Health Sci Eng 11:11
Ghio AJ, Carraway MS, Madden MC (2012) Composition of air pollution particles and oxidative stress in cells, tissues, and living systems. J Toxicol Environ Health B Crit Rev 15:1–21
Kan H, Chen B, Zhao N, London SJ, Song G, Chen G, Zhang Y, Jiang L, Committee HEIHR (2010) Part 1. A time-series study of ambient air pollution and daily mortality in Shanghai, China. Res Rep Health Eff Inst, 17-78
Lam HC, Li AM, Chan EY, Goggins WB 3rd (2016) The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: a time-series study. Thorax 71:1097–1109
Li MH, Fan LC, Mao B, Yang JW, Choi AMK, Cao WJ, Xu JF (2016) Short-term exposure to ambient fine particulate matter increases hospitalizations and mortality in COPD: a systematic review and meta-analysis. Chest 149:447–458
Lin G, Fu J, Jiang D, Wang J, Wang Q, Dong D (2015) Spatial variation of the relationship between PM 2.5 concentrations and meteorological parameters in China. Biomed Res Int 2015:684618
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, AlMazroa MA, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Abdulhak AB, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, de Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FGR, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Memish ZA, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KMV, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA III, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, de León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJL (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2095–2128
Meng K, Xu X, Cheng X, Xu X, Qu X, Zhu W, Ma C, Yang Y, Zhao Y (2018) Spatio-temporal variations in SO2 and NO2 emissions caused by heating over the Beijing-Tianjin-Hebei Region constrained by an adaptive nudging method with OMI data. Sci Total Environ 642:543–552
Morrow PE, Utell MJ, Bauer MA, Smeglin AM, Frampton MW, Cox C, Speers DM, Gibb FR (1992) Pulmonary performance of elderly normal subjects and subjects with chronic obstructive pulmonary disease exposed to 0.3 ppm nitrogen dioxide. Am Rev Respir Dis 145:291–300
Nhung NTT, Amini H, Schindler C, Kutlar Joss M, Dien TM, Probst-Hensch N, Perez L, Kunzli N (2017) Short-term association between ambient air pollution and pneumonia in children: a systematic review and meta-analysis of time-series and case-crossover studies. Environ Pollut 230:1000–1008
Qiu H, Pun VC, Tian L (2018) Short-term effects of fine and coarse particles on deaths in Hong Kong elderly population: an analysis of mortality displacement. Environ Pollut 241:148–154
Schwartz J (2001) Is there harvesting in the association of airborne particles with daily deaths and hospital admissions? Epidemiology 12:55–61
Tian L, Ho KF, Wang T, Qiu H, Pun VC, Chan CS, Louie PK, Yu IT (2014a) Ambient carbon monoxide and the risk of hospitalization due to chronic obstructive pulmonary disease. Am J Epidemiol 180:1159–1167
Tian S, Pan Y, Liu Z, Wen T, Wang Y (2014b) Size-resolved aerosol chemical analysis of extreme haze pollution events during early 2013 in urban Beijing, China. J Hazard Mater 279:452–460
Tsai SS, Chang CC, Yang CY (2013) Fine particulate air pollution and hospital admissions for chronic obstructive pulmonary disease: a case-crossover study in Taipei. Int J Environ Res Public Health 10:6015–6026
van Eeden SF, Hogg JC (2002) Systemic inflammatory response induced by particulate matter air pollution: the importance of bone-marrow stimulation. J Toxic Environ Health A 65:1597–1613
White AJ, Gompertz S, Stockley RA (2003) Chronic obstructive pulmonary disease . 6: the aetiology of exacerbations of chronic obstructive pulmonary disease. Thorax 58:73–80
Yang Q, Chen Y, Krewski D, Burnett RT, Shi Y, McGrail KM (2005) Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ Res 99:99–105
Yang J, Zhou M, Ou CQ, Yin P, Li M, Tong S, Gasparrini A, Liu X, Li J, Cao L, Wu H, Liu Q (2017) Seasonal variations of temperature-related mortality burden from cardiovascular disease and myocardial infarction in China. Environ Pollut 224:400–406
Zeka A, Zanobetti A, Schwartz J (2006) Individual-level modifiers of the effects of particulate matter on daily mortality. Am J Epidemiol 163:849–859
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, Liu J, Zhang M, Qi J, Yu S, Afshin A, Gakidou E, Glenn S, Krish VS, Miller-Petrie MK, Mountjoy-Venning WC, Mullany EC, Redford SB, Liu H, Naghavi M, Hay SI, Wang L, Murray CJL, Liang X (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet
Acknowledgments
The authors thank the database of the Health Insurance Center of Shijiazhuang City providing population support; we appreciate the Shijiazhuang Environmental Protection Department providing for air pollution monitoring data and Shijiazhuang Meteorological Bureau providing for meteorological data.
Funding
This work is supported by the National Natural Science Foundation of China (81770020 to XY) and Haze Special Project of Hebei Province Finance Department (2014-1257).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Patient consent
Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Additional information
Responsible editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qu, F., Liu, F., Zhang, H. et al. Comparison of air pollutant-related hospitalization burden from AECOPD in Shijiazhuang, China, between heating and non-heating season. Environ Sci Pollut Res 26, 31225–31233 (2019). https://doi.org/10.1007/s11356-019-06242-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-019-06242-3