Abstract
There are indications that in persons of older age, systolic blood pressure (SBP) is no longer associated with mortality. This raises the question whether the predictive value of SBP changes from younger to older age groups. Analysis in the Rotterdam Study, a population-based prospective cohort study among 4,612 participants aged ≥55 years without previous cardiovascular disease and with a median follow-up of 14.9 (interquartile range, 11.1–15.8) years. Within four age groups (55–64, 65–74, 75–84, ≥85 years), the predictive value of baseline SBP for mortality was studied. From age 55 to ≥85 years, risk of all-cause mortality associated with SBP ≥160 mmHg decreased from HR 1.7 (95%CI 1.2–2.2) to HR 0.7 (95%CI 0.4–1.1), p for trend <0.001. For participants with SBP 140–159 mmHg, the risk decreased from HR 1.2 (95%CI 0.9–1.5) to HR 0.7 (95%CI 0.5–1.1), p for trend <0.001. Analyses in the 5-year age groups showed an increased risk with higher SBPs up to age 75 years. After 75 years, a trend towards SBP no longer being associated with an increased mortality risk was seen in our study. These findings need to be considered with recently reported beneficial effects of antihypertensive treatment in this age group.
Similar content being viewed by others
Introduction
High systolic blood pressure (SBP) is recognized as an important risk factor for cardiovascular disease (CVD), irrespective of age (Lewington et al. 2002). However, observational cohort studies in older populations report that high SBP does not predict mortality from age 75 years onwards (Alli et al. 1999; Van Bemmel et al. 2006a, b; Boshuizen et al. 1998; Bulpitt and Fletcher 1992; Guo et al. 1997; Hakala et al. 1997; Heikinheimo et al. 1990; Kagiyama et al. 2008; Lernfelt and Svanborg 2002; Molander et al. 2008; Oates et al. 2007; Okayama et al. 2006; Rajala et al. 1983; Rastas et al. 2006; Satish et al. 2001a, b; Trenkwalder et al. 1999). Therefore, the value of SBP to predict mortality may change from younger to older age groups. As previous studies were performed in cohorts of exclusively older people, the age at which the association between SBP and mortality starts to fade remains unknown and needs to be studied in a large cohort with a wider age range.
The present study aims to determine the risk prediction of all-cause and (non)cardiovascular mortality with SBP in persons without a history of CVD across increasing age categories from age 55 years onwards. As diastolic blood pressure (DBP) loses its predictive abilities for mortality in adults aged over 50 years (Taylor et al. 2011), only SBP is investigated in this study.
Methods
Study population
Data for this study were derived from the Rotterdam Study, a population-based prospective cohort study including 7,983 participants (4,878 women and 3,105 men) aged 55 years and over, living in Ommoord (an urban district of Rotterdam, the Netherlands). The study has been described in detail elsewhere (Hofman et al. 2009). The Medical Ethics Committee of the Erasmus University Medical Center approved the study and written informed consent was obtained from all participants.
For the present study, we excluded all participants with a history of CVD, defined as myocardial infarction, coronary interventions (percutaneous coronary interventions or coronary artery bypass grafts), ischemic and hemorrhagic stroke, atrial fibrillation and peripheral arterial disease (n = 2,294); an additional 308 participants were excluded because data on cardiovascular history were missing. The prevalence of prior CVD (overall 2,294/7,983; 29%), increased with increasing age: 18% in age group 55–64 years, 29% in age group 65–74 years, 49% in age group 75–84 years, and 71% in patients aged ≥85 years. Of the 5,381 participants available for the present study blood pressure data were available for 4,612 (85.7%) persons, which was the final sample size.
Measurements
Between 1990 and 1993 participants visited the research center for the baseline examination, at which blood pressure measurements were obtained. Blood samples were taken for measurement of total cholesterol and high-density cholesterol, body mass index was assessed, as well as participants’ history of smoking and diabetes mellitus. Blood pressure measurements were carried out by research assistants using a standardized protocol. SBP (Korotkoff phase I) was measured in duplicate on the right arm using a random-zero sphygmomanometer (with a 14 × 38 cm cuff), after the participant had been seated for at least 5 min. The mean of the two blood pressures values was used in the analyses. For SBP, three categories for blood pressure were used according to the European guidelines on CVD prevention in clinical practice (Mancia et al. 2007), namely “normal” (SBP <140 mmHg), “grade 1 hypertension” (SBP 140–159 mmHg) or “grade 2 hypertension or higher” (SBP ≥160 mmHg) were used.
Data on the use of antihypertensive medication (ATC codes: C02, C03, C07) were collected through interviews. Medication containers were checked during the interview. A SBP ≥160 mmHg was reported to the participant’s general practitioner (GP), unless the GP was already informed about the participant’s hypertension.
Follow-up
In the Rotterdam Study, data on all-cause mortality are obtained in two ways. Participants living independently in the area of Ommoord are followed by continuous monitoring of the municipal address files and are considered to have complete follow-up with respect to vital status (i.e., they are still alive at the reference date). Participants living outside Ommoord and/or in a nursing home were at least alive at the last date of manual data collection; these subjects have partial follow-up. The completeness of follow-up is the ratio of the total number of observed person-years and the total number of potential person-years (Clark et al. 2002). Mean intervals from baseline measurements until death varied with age at baseline and were 14.4, 13.2, 10.1 and 5.6 years for the age groups 55–64, 65–74, 75–84 and ≥85 years, respectively.
Endpoints
A detailed description of the procedure to classify events has been published earlier (Mattace-Raso et al. 2004). All information on possible events was obtained from the participant’s GP and subsequently classified independently by two research physicians. In case of disagreement, consensus was reached in a plenary session. A medical expert in the field of CVD verified all these events. This verification was considered definite. Classification of events was based on the International Classification of Diseases, 10th revision (ICD-10). Events followed by death within 28 days were classified as fatal. Cardiovascular mortality was defined as mortality from coronary heart disease (ICD-10 codes I20–I25, I46, I49, I50, I60–I67, I70–I74, and R96) or stroke (ICD-10 codes I60–I67). Noncardiovascular mortality was defined as all other mortality, other than cardiovascular mortality.
Data analysis
Differences in characteristics between participants in the lowest, middle, and highest SBP groups were tested with the chi-square test for categorical variables and the Jonkheere–Terpstra tests for continuous variables. Within strata by age group (at baseline 55–64 years, 65–74, 75–84 and >85 years), risk estimates (hazard ratios) were calculated for the relation between SBP at baseline, and all-cause and (non)cardiovascular mortality, using a Cox proportional hazards model. Since the aim was to determine the predictive value of SBP (as opposed to exploring etiological pathways), results were not adjusted for potential confounders, but for age (per age category, as a continuous variable) and sex only. For all participants, including those using antihypertensive medication, the actual blood pressure is used in the analysis. Analyses were repeated in strata according to baseline use of antihypertensive medication.
Because of suggestions in the literature to use 150 mmHg as a treatment target in older people (Beckett et al. 2008), as sensitivity analysis we used categories of blood pressure with a corresponding reference group: “reference” (SBP <150 mmHg), SBP 150–159 mmHg or SBP ≥160 mmHg. Additionally, to evaluate the influence of the arbitrarily chosen age groups, all analyses were repeated in 5-year interval age groups (at baseline 55–59 years, 60–64, 65–69, 70–74, 75–79, 80–84, and >85 years), as well as in 10-year interval age groups (at baseline 55–59 years, 60–69, 70–79, and ≥80 years). Analyses were performed using SPSS 16.0 for Windows (SPSS, Chicago, IL, USA).
Results
Table 1 shows the baseline characteristics of the participants, including other cardiovascular risk factors. Mean age at baseline was 67.4 (range, 55.0–106.2) years. The prevalence of increased SBP increased with age.
Follow-up was completed until 1 January 2008 for all-cause mortality and until 1 January 2005 for cause-specific mortality (both complete for 99.0%). The median duration of follow-up was 14.9 (interquartile range (IQR) 11.1–15.8) years for all-cause mortality and 12.1 (IQR 10.8–13.0) years for cause-specific mortality. During follow-up, overall mortality increased from 12.1/1,000 person-years (1.1% in the first year of follow-up) in those aged 55–64 years to 168.1/1,000 person-years (13.0% in the first year of follow-up) in those aged 85 years and over.
Risk of all-cause mortality
Relative risks adjusted for age and sex associated with SBP ≥160 mmHg, compared to the reference group SBP <140 mmHg, decreases with age from HR≥160 1.7 (95% CI: 1.2, 2.2) in the age group 55–64 years, to HR≥160 0.7 (95% CI: 0.4, 1.1) in the age group ≥85 years (p for trend <0.001; Table 2). For SBP ≥140–159 mmHg the same trend could be seen: HR140–159 1.2 (95% CI: 0.9, 1.5) in the age group 55–64 years, to HR140–159 0.7 (95% CI: 0.5, 1.1) in the age group ≥85 years (p for trend <0.001).
When participants were categorized into 5-year age groups, the increased risk with higher SBPs was present up to age 75 years: in the age group 70–74 years, the HR140–159 is 1.4 (95% CI: 1.1, 1.7) and in the age group 75–79 years and over the HR reaches unity (HR140–159 1.1, 95% CI: 0.9, 1.4). For the group with the highest SBPs, in the age group 70–74 years, the HR≥160 is 1.3 (95% CI: 1.0, 1.7). Relative risks in the age group 75–79 and 80–84 years are similar, whereas in the age group ≥85 years HR≥160 is 0.7 (95% CI: 0.4, 1.1). Using a reference group with SBP <150 mmHg shows similar results with HR150–159 0.8 (95% CI: 0.5, 1.3) and HR≥160 0.8 (95% CI: 0.5, 1.2) at age ≥85 years (data not shown).
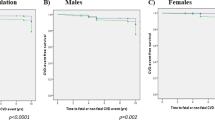
Figure 1 shows absolute mortality, presented as all-cause mortality rate (per 1,000 person-years) depending on two levels of SBP: <140 and ≥160 mmHg. Between age 75 and 85 years, the absolute mortality risk reverses, with SBP <140 mmHg being related to higher mortality than SBP ≥160 mmHg.
Risk of cardiovascular mortality
In the age group 55–64 years, the risk of cardiovascular mortality was increased for participants with SBP ≥160 mmHg (HR≥160 2.9, 95% CI: 1.4, 5.9) compared to those with SBP <140 mmHg. In the higher age groups, this risk decreases (at age ≥85 years: HR≥160 0.9, 95% CI: 0.3, 2.1). The same applies to the relative risks associated with SBP 140–159 mmHg: HR140–159 2.1, 95% CI: 1.1, 3.9 for age 55–64 and HR140–159 1.3, 95% CI: 0.6, 2.8 for age ≥85 (p for trend <0.001; Table 2).
Risk of noncardiovascular mortality
Noncardiovascular mortality is increased with a higher SBP in the younger age groups, but in those aged 75–84 years the relative risk reaches unity. For participants aged ≥85 years, the risk for noncardiovascular mortality was decreased (HR140–159 0.6, 95% CI: 0.3, 1.0, and HR≥160 0.7, 95% CI: 0.4, 1.2) compared to participants aged 55–64 years (HR140–159 1.0, 95% CI: 0.7, 1.4, and HR≥160 1.3, 95% CI: 0.9, 2.0), p for trend = 0.001 (Table 2).
Additional analyses (data not shown)
When participants were stratified according to the use of antihypertensive medication at baseline, results in both strata were roughly similar. Excluding the participants who died in the first year of follow-up (n = 54) yielded similar results.
Discussion
This analysis in the Rotterdam Study shows that the predictive value of SBP for mortality differs with age in people aged 55 years and over without a history of CVD. Between age 55 and 75 years, high SBP predicts higher mortality risk. From age 75 years onwards, we observed a significant trend indicating that SBP no longer predicts increased mortality, although due to lower numbers in the higher age-groups the hazard ratios in each age group were not significant. From age 85 years onwards, high SBP even predicts lower mortality risk, confirming earlier observations in the oldest old (Van Bemmel et al. 2006a)
In 1992 a review of observational population studies relating blood pressure to mortality in older persons, a weaker association between SBP and mortality from age 75 years onwards was reported (Bulpitt and Fletcher 1992). Since then, several individual studies have reported on the fading association between SBP and mortality and cardiovascular morbidity in older persons (Alli et al. 1999; Van Bemmel et al. 2006a, b; Boshuizen et al. 1998; Heikinheimo et al. 1990; Molander et al. 2008; Nelson et al. 2011; Okayama et al. 2006; Satish et al. 2001b; Trenkwalder et al. 1999). However, most of these studies had a relatively heterogeneous population (age, previous CVD or use of antihypertensive medication, high-risk populations) and methodologies (measurement of blood pressure, length of follow-up, and measurement of outcomes). We are the first to show the changing predictive value of SBP across the age span within a single population-based cohort.
Our results only partly agree with a landmark meta-analysis published in 2002, which included data from one million adults without a history of CVD from 61 prospective studies, with age-specific relevance of blood pressure as primary focus of attention (Lewington et al. 2002). This meta-analysis demonstrated a progressive slowing down with age of the rate of increase of cardiovascular mortality and morbidity risks with increasing SBPs, but did not show a reversal of risks in their highest age group (80 years and over). Whether inclusion of all recently published studies that used cohorts of older people would alter these estimations remains to be seen.
Our population-based study has several strengths. The population studied is highly representative for those without a history of CVD in the general population, and therefore reflects the population that would be addressed by systematic screening as a means of primary prevention of CVD. A high response rate, almost complete follow-up, and uniformity in methodology and data collection in all participants reinforce internal validity and generalizability. In addition, our study employs various strata of age groups, allowing determination of the specific age at which the association between SBP and mortality disappears and subsequently reverses. It may be seen as a weakness that GPs were notified about previously unrecognized hypertension, potentially causing misclassification. Since in the younger age groups (≤75 years) robust correlations of high SBP and increased mortality risk were observed, and since it is likely that participants in these age groups were treated more strictly than those in older age groups, this almost certainly did not influence our results (Di Bari et al. 1999). All our prognostic analyses were based on a (twice repeated) blood pressure measurement at one point in time, and not on a series of blood pressure measurements over time. Although the latter would have been interesting from an etiological point of view, a single blood pressure estimation is in keeping with current practice with regard to cardiovascular risk prediction and the use of various risk functions, such as the Framingham Risk Score and SCORE (D’Agostino et al. 2001; Ezzati et al. 2002).
In view of the observational design of the data collection, analyses with regard to the effect of antihypertensive medication are bound to be confounded by prescription bias. Therefore, we did not perform analyses to study effect of medication. To understand the possible clinical consequences of our findings, it is important to combine our results with the recently reported beneficial effects of antihypertensive treatment of (relatively healthy) persons aged 80 years and over (Beckett et al. 2008; Bejan-Angoulvant et al. 2010). Thus, although high SBP does not predict mortality above age 75 years, antihypertensive treatment still has a beneficial outcome in these age groups. Reductions in total mortality, incidence of stroke, heart failure, and all cardiovascular events have been shown (Beckett et al. 2008). This is not a unique concept in the very old, since in this age group it has also been shown that high total cholesterol levels are associated with better survival than low cholesterol levels (Weverling-Rijnsburger et al. 1997), while at the same time statin treatment in older populations has been proven beneficial (Shepherd et al. 2002). To understand the apparent contradiction regarding SBP, it is important to elucidate the etiology of the change in prediction of negative clinical outcomes by SBP in higher age groups. The population of people of old age includes relatively many subjects with decreasing blood pressure, since SBP is known to decrease in the last years before dying (Satish et al. 2001a). Decreases in SBP as a sign of imminent heart failure, could underlie the observed worse prognosis in these individuals (van Bemmel et al. 2009). Participants with formerly higher blood pressures, but now a decreasing blood pressure due to (imminent) heart failure, cause the increased absolute risk of mortality in the low blood pressure group. Nonetheless, antihypertensive medication for those with high blood pressure reduces this incidence of heart failure (Beckett et al. 2008). Another explanation for our findings could be that age becomes such a strong risk factor with increasing age that it is difficult for other risk factors to have an additional prognostic effect. Some have therefore agued to confine cardiovascular risk prediction to age-based prediction alone (Wald et al. 2011). However, this still does not explain the reversal of risk in those participants aged 85 and over.
Other important questions raised by this study are: Is antihypertensive treatment beneficial for all older subjects with high SBP, or should those with falling blood pressure be identified? Who will not benefit from antihypertensive treatment? Should antihypertensive medication be lowered or discontinued in specific subgroups of older patients?
In conclusion, the predictive value of SBP for mortality differs with age in people aged 55 years and over without a history of CVD. Between age 55 and 75 years, high SBP predicts higher mortality risk, but from age 75 years onwards a significant trend shows that SBP levels no longer predict mortality risk (although hazard ratios per age group do not reach significance). From age 85 years onwards, high SBP even predicts lower mortality risk. The discrepancy of these predictive findings together with recently shown beneficial effects of antihypertensive treatment also in high age groups fuels the necessary discussion about possible clinical consequences. Future studies should use a longitudinal approach to explore how changing blood pressure is linked to mortality risk.
References
Alli C, Avanzini F, Bettelli G, Colombo F, Torri V, Tognoni G (1999) The long-term prognostic significance of repeated blood pressure measurements in the elderly: SPAA (Studio sulla Pressione Arteriosa nell’Anziano) 10-year follow-up. Arch Intern Med 159:1205–1212
Beckett NS, Peters R, Fletcher AE, Staessen JA et al (2008) Treatment of hypertension in patients 80 years of age or older. N Engl J Med 358:1887–1898
Bejan-Angoulvant T, Saadatian-Elahi M, Wright JM, Schron EB et al (2010) Treatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trials. J Hypertens 28:1366–1372
Boshuizen HC, Izaks GJ, van Buuren S, Ligthart GJ (1998) Blood pressure and mortality in elderly people aged 85 and older: community based study. BMJ 316:1780–1784
Bulpitt CJ, Fletcher AE (1992) Aging, blood pressure and mortality. J Hypertens Suppl 10:S45–S49
Clark TG, Altman DG, De Stavola BL (2002) Quantification of the completeness of follow-up. Lancet 359:1309–1310
D’Agostino RBS, Grundy S, Sullivan LM, Wilson P (2001) Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 286:180–187
Di Bari M, Salti F, Nardi M, Pahor M et al (1999) Undertreatment of hypertension in community-dwelling older adults: a drug-utilization study in Dicomano, Italy. J Hypertens 17:1633–1640
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ (2002) Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 360:1347–1360
Guo Z, Viitanen M, Winblad B (1997) Low blood pressure and five-year mortality in a Stockholm cohort of the very old: possible confounding by cognitive impairment and other factors. Am J Public Health 87:623–628
Hakala SM, Tilvis RS, Strandberg TE (1997) Blood pressure and mortality in an older population. A 5-year follow-up of the Helsinki Ageing Study. Eur Heart J 18:1019–1023
Heikinheimo RJ, Haavisto MV, Kaarela RH, Kanto AJ, Koivunen MJ, Rajala SA (1990) Blood pressure in the very old. J Hypertens 8:361–367
Hofman A, Breteler MM, van Duijn CM, Janssen HL et al (2009) The Rotterdam Study: 2010 objectives and design update. Eur J Epidemiol 24:553–572
Kagiyama S, Fukuhara M, Ansai T, Matsumura K et al (2008) Association between blood pressure and mortality in 80-year-old subjects from a population-based prospective study in Japan. Hypertens Res 31:265–270
Lernfelt B, Svanborg A (2002) Change in blood pressure in the age interval 70–90. Late blood pressure peak related to longer survival. Blood Press 11:206–212
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Collaboration PS (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360:1903–1913
Mancia G, De Backer G, Dominiczak A, Cifkova R et al (2007) 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28:1462–1536
Mattace-Raso FU, van der Cammen TJ, van Popele NM, van der Kuip DA et al (2004) Blood pressure components and cardiovascular events in older adults: the Rotterdam Study. J Am Geriatr Soc 52:1538–1542
Molander L, Lovheim H, Norman T, Nordström P, Gustafson Y (2008) Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc 56:1853–1859
Nelson MR, Ryan P, Ramsay E, Willson K, Tonkin AM, Wing LMH, Simon L, Reid CM (2011) A score for the prediction of cardiovascular events in the hypertensive aged. Am J Hypert. doi:10.1038/ajh.2011.192
Oates DJ, Berlowitz DR, Glickman ME, Silliman RA, Borzecki AM (2007) Blood pressure and survival in the oldest old. J Am Geriatr Soc 55:383–388
Okayama A, Kadowaki T, Okamura T, Hayakawa T, Ueshima H (2006) Age-specific effects of systolic and diastolic blood pressures on mortality due to cardiovascular diseases among Japanese men (NIPPON DATA80). J Hypertens 24:459–462
Rajala S, Haavisto M, Heikinheimo R, Mattila K (1983) Blood pressure and mortality in the very old. Lancet 2:520–521
Rastas S, Pirttila T, Viramo P, Verkkoniemi A et al (2006) Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc 54:912–918
Satish S, Zhang DD, Goodwin JS (2001a) Clinical significance of falling blood pressure among older adults. J Clin Epidemiol 54(9):961–967
Satish S, Freeman DH Jr, Ray L, Goodwin JS (2001b) The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc 49:367–374
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG, PROSPER study group (2002) PROspective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 360:1623–1630
Taylor BC, Wilt TJ, Welch HG (2011) Impact of diastolic and systolic blood pressure on mortality: implications for the definition of “normal”. J Gen Intern Med Jul 26:685–690
Trenkwalder P, Hendricks P, Schoniger R, Rossberg J, Lydtin H, Hense HW (1999) Hypertension as a risk factor for cardiovascular morbidity and mortality in an elderly German population; the prospective STEPHY II study. Starnberg Study on Epidemiology of Parkinsonism and Hypertension in the Elderly. Eur Heart J 20:1752–1756
Van Bemmel T, Gussekloo J, Westendorp RG, Blauw GJ (2006a) In a population-based prospective study, no association between high blood pressure and mortality after age 85 years. J Hypertens 24:287–292
Van Bemmel T, Woittiez K, Blauw GJ, van der Sman-de BF, Dekker FW, Westendorp RG, Gussekloo J (2006b) Prospective study of the effect of blood pressure on renal function in old age: the Leiden 85-Plus Study. J Am Soc Nephrol 17:2561–2566
Van Bemmel T, Holman ER, Gussekloo J, Blauw GJ, Bax JJ, Westendorp RG (2009) Low blood pressure in the very old, a consequence of imminent heart failure: the Leiden 85-plus Study. J Hum Hypertens 23:27–32
Wald NJ, Simmonds M, Morris JK (2011) Screening for future cardiovascular disease using age alone compared with multiple risk factors and age. PLoS One 6:e18742
Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG (1997) Total cholesterol and risk of mortality in the oldest old. Lancet 350:1119–11123
Acknowledgements
The contribution of inhabitants, general practitioners, and pharmacists of the Ommoord district to the Rotterdam Study is gratefully acknowledged. The authors also gratefully acknowledge the contributions of previous principal investigators of the Rotterdam Study, including Frank van den Ouweland (endocrine diseases), Diederick Grobbee (cardiovascular diseases), Paulus de Jong (ophthalmic diseases), and Huibert Pols (endocrine diseases). The contribution of Guy Brusselle to the study of respiratory diseases is also gratefully acknowledged. The authors thank Prof. RGJ Westendorp PhD MD of the Department of Geriatrics and Gerontology, Leiden University Medical Center and the Netherlands Consortium for Healthy Aging, Leiden, for his advice during the production of this article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Blom, J.W., de Ruijter, W., Witteman, J.C.M. et al. Changing prediction of mortality by systolic blood pressure with increasing age: the Rotterdam study. AGE 35, 431–438 (2013). https://doi.org/10.1007/s11357-011-9349-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-011-9349-7