Summary
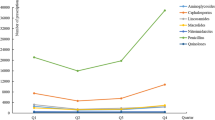
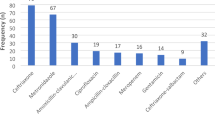
With dwindling number of new antibiotics and inappropriate use of antibiotics, the emergence and spread of antibiotics resistance occurs commonly in healthcare institutions worldwide. In China, antibiotics are commonly overprescribed and misused. This study is to assess the effect of the nationwide special campaign on antibiotic stewardship program (ASP) at specialized hospitals in China by investigating prescription information from 2011 to 2012. Data on the hospital consumption and prescription of systemic antibiotics were obtained from four specialized hospitals, including maternity, children’s, stomatological and cancer hospitals. Systematic random sampling was used to select outpatient prescriptions and inpatient cases. A total of 105 specialized hospitals in 2011 and 121 specialized hospitals in 2012 were analysed. The defined daily doses (DDDs) per 100 inpatient days, the percentage of antibiotic use in outpatient prescriptions, and the percentage of antibiotic use in inpatient cases were used as measurements of antibiotic use. The overall antibiotic use density in the selected hospitals decreased between 2011 and 2012 from 39.37 to 26.54 DDD/100 inpatient days (P<0.001). The percentage of antibiotic use in outpatient prescriptions (range: 24.12%–18.71%, P=0.109) and inpatient cases (64.85%–60.10%, P=0.006) also decreased within the two years. Significant changes were observed among regions and different hospitals within the two years. And antibiotic consumption was correlated with the type and size of specialized hospital in 2012, but not with the regions. This analysis of antibiotic consumption of specialized hospitals allows relevant comparisons for benchmarking and shows that national ASP has improved antibiotic rational use in China. The data will assist policymakers in formulating effective strategies to decrease antibiotic overuse and identify areas that require further work.
Similar content being viewed by others
References
Klugman KP, Koornhof HJ. Worldwide increase in pneumococcal antibiotic resistance. Lancet, 1989,2(8660): 444
Hawkey PM. Action against antibiotic resistance: no time to lose. Lancet, 1998,351(9112):1298–1299
Dong L, Yan H, Wang D. Antibiotic prescribing patterns in village health clinics across 10 provinces of Western China. J Antimicrob Chemother, 2008, 62(2):410–415
Ferber D. Antibiotic resistance. Superbugs on the hoof? Science, 2000, 288(5467):792–794
Kmietowicz Z. WHO warns of threat of “superbugs”. BMJ, 2000, 320(7250):1624
le Grand A, Hogerzeil HV, Haaijer-Ruskamp FM. Intervention research in rational use of drugs: a review. Health Policy Plan, 1999, 14(2):89–102
Phelps CE. Bug/drug resistance. Sometimes less is more. Med Care, 1989, 27(2):194–203
Zhang R, Eggleston K, Rotimi V, et al. Antibiotic resistance as a global threat: evidence from China, Kuwait and the United States. Global Health, 2006, 2:6
World Health Organization. The evolving threat of antimicrobial resistance: Options for action. World Health Organization, 2012
Tang S, Meng Q, Chen L, et al. Tackling the challenges to health equity in China. Lancet, 2008, 372(9648): 1493–1501
Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet, 2012, 379(9818):805–814
Kondro W. Canadian scientists urge government to develop antibiotic plan. Lancet, 2002, 360(9341):1230
de Man P, Verhoeven BA, Verbrugh HA, et al. An antibiotic policy to prevent emergence of resistant bacilli. Lancet, 2000, 355(9208):973–978
Schito GC, Debbia EA, Marchese A. The evolving threat of antibiotic resistance in Europe: new data from the Alexander Project. J Antimicrob Chemother, 2000, 46(Suppl T1):3–9
WHO, Ministry of Health in China. China-WHO Country Cooperation Strategy 2013-2015. World Health Organization, 2013
Chen W, Tang S, Sun J, et al. Availability and use of essential medicines in China: manufacturing, supply, and prescribing in Shandong and Gansu provinces. BMC Health Serv Res, 2010, 10:211
Xiang X, Yang C, Wang D, et al. Effects of China’s national essential medicines policy on the use of injection in primary health facilities. J Huazhong Univ Sci Technolog Med Sci, 2012, 32(4):626–629
Heddini A, Cars O, Qiang S, et al. Antibiotic resistance in China—a major future challenge. Lancet, 2009, 373(9657):30
Jing L. China faces great risk due to overuse of antibiotics. 2013. http://www.nationmultimedia.com/opinion/China-faces-great-risk-due-to-overuse-of-antibioti-30207488.html
Reynolds L, McKee M. Factors influencing antibiotic prescribing in China: an exploratory analysis. Health Policy, 2009, 90(1):32–36
Bi P, Tong S, Parton KA. Family self-medication and antibiotics abuse for children and juveniles in a Chinese city. Soc Sci Med, 2000, 50(10):1445–1450
Ramanan Laxminarayan AMDH. Extending the cure: policy responses to the growing threat of antibiotic resistance. Washington, DC 20036-1400 USA: 2007
Ministry of Health in China. Interim provisions on the administration of hospital pharmacy. 2002. http://www.moh.gov.cn/mohyzs/s3577/200804/18787.shtml (Chinese)
Xiao Y, Li L. Legislation of clinical antibiotic use in China. Lancet Infect Dis, 2013, 13(3):189–191
Yang L, Liu C, Ferrier JA, et al. The impact of the National Essential Medicines Policy on prescribing behaviours in primary care facilities in Hubei province of China. Health Policy Plan, 2012
Ministry of Health in China. Notification for the special campaign of antibiotics rational use in hospitals. 2012. http://www.moh.gov.cn/mohyzs/s3586/201203/54251.shtml (Chinese)
Regev-Yochay G, Raz M, Dagan R, et al. Reduction in antibiotic use following a cluster randomized controlled multifaceted intervention: the Israeli judicious antibiotic prescription study. Clin Infect Dis, 2011, 53(1):33–41
Kern WV, de With K, Nink K, et al. Regional variation in outpatient antibiotic prescribing in Germany. Infection, 2006, 34(5):269–273
Filippini M, Masiero G, Moschetti K. Socioeconomic determinants of regional differences in outpatient antibiotic consumption: evidence from Switzerland. Health Policy, 2006, 78(1):77–92
National Bureau of Statistics in China. The Divide of Regions According to Economic Development in China. 2012. http://www.stats.gov.cn/tjzs/t20110613_402731597.htm. (Chinese)
National Bureau of Statistics in China. Division Method of Regions. 2011. http://www.stats.gov.cn/tjzs/t20110613_402731597.htm. (Chinese)
Antachopoulos C, Dotis J, Pentsioglou V. Development of a paediatric daily defined dose system for the measurement of antibiotic consumption in paediatric units. 14th European Congress of Clinical Microbiology and Infectious Diseases. Prague, Czech Republic: 2004
Kern WV, de With K, Steib-Bauert M, et al. Antibiotic use in non-university regional acute care general hospitals in southwestern Germany, 2001–2002. Infection, 2005, 33(5–6):333–339
De WK, Steib-Bauert M, Straach P, et al. Is there significant regional variation in hospital antibiotic consumption in Germany? Infection, 2006, 34(5):274–277
Piovani D, Clavenna A, Cartabia M, et al. The regional profile of antibiotic prescriptions in Italian outpatient children. Eur J Clin Pharmacol, 2012, 68(6):997–1005
Zhang W, Shen X, Bergman U, et al. Drug utilisation 90% (DU90%) profiles of antibiotics in five Chinese children’s hospitals (2002–2006). Int J Antimicrob Agents, 2008, 32(3):250–255
Ceyhan M, Yildirim I, Ecevit C, et al. Inappropriate antimicrobial use in Turkish pediatric hospitals: a multicenter point prevalence survey. Int J Infect Dis, 2010, 14(1): e55–e61
Ashiru-Oredope D, Sharland M, Charani E, et al. Improving the quality of antibiotic prescribing in the NHS by developing a new Antimicrobial Stewardship Programme: Start Smart—Then Focus. J Antimicrob Chemother, 2012, 67(Suppl 1):i51–i63
Low M, Nitzan O, Bitterman H, et al. Trends in outpatient antibiotic use in Israel during the years 2000–2010: setting targets for an intervention. Infection, 2013, 41(2): 401–407
Cairns KA, Jenney AW, Abbott IJ, et al. Prescribing trends before and after implementation of an antimicrobial stewardship program. Med J Aust, 2013, 198(5): 262–266
Dumartin C, Rogues AM, Amadeo B, et al. Antibiotic stewardship programmes: legal framework and structure and process indicator in Southwestern French hospitals, 2005–2008. J Hosp Infect, 2011, 77(2):123–128
Hadi U, Keuter M, van Asten H, et al. Optimizing antibiotic usage in adults admitted with fever by a multifaceted intervention in an Indonesian governmental hospital. Trop Med Int Health, 2008, 13(7):888–899
Wilf-Miron R, Ron N, Ishai S, et al. Reducing the volume of antibiotic prescriptions: a peer group intervention among physicians serving a community with special ethnic characteristics. J Manag Care Pharm, 2012, 18(4): 324–328
Elseviers MM, Ferech M, Vander SR, et al. Antibiotic use in ambulatory care in Europe (ESAC data 1997–2002): trends, regional differences and seasonal fluctuations. Pharmacoepidemiol Drug Saf, 2007, 16(1):115–123
Dumartin C, L’Heriteau F, Pefau M, et al. Antibiotic use in 530 French hospitals: results from a surveillance network at hospital and ward levels in 2007. J Antimicrob Chemother, 2010, 65(9):2028–2036
Grau S, Fondevilla E, Mojal S, et al. Antibiotic consumption at 46 VINCat hospitals from 2007 to 2009, stratified by hospital size and clinical services. Enferm Infecc Microbiol Clin, 2012, 30(Suppl 3):43–51
D’Alerte R. Surveillance de la consommation des antibiotiques. Institut de veille sanitaire, 2010
Sumpradit N, Chongtrakul P, Anuwong K, et al. Antibiotics Smart Use: a workable model for promoting the rational use of medicines in Thailand. Bull World Health Organ, 2012, 90(12):905–913
Stockley JM. European Antibiotic Awareness Day 2012: getting smart about antibiotics, a public-professional partnership. J Infect, 2012, 65(5):377–379
Currie J, Lin W, Zhang W. Patient knowledge and antibiotic abuse: Evidence from an audit study in China. J Health Econ, 2011, 30(5):933–949
Goossens H, Ferech M, Vander SR, et al. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet, 2005, 365(9459): 579–587
Kuster SP, Ruef C, Bollinger AK, et al. Correlation between case mix index and antibiotic use in hospitals. J Antimicrob Chemother, 2008, 62(4):837–842
Sabath LD, Notto DA. Analysis of factors influencing antibiotic usage in hospitals. Prog Clin Biol Res, 1979, 35:65–74
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by grants from the General Program of National Natural Science Foundation of China (No. 71073062) and Major Project in Philosophy and Social Science of Ministry of Education in China (No. 10JZD0027).
Rights and permissions
About this article
Cite this article
Zou, Xx., Fang, Z., Min, R. et al. Is nationwide special campaign on antibiotic stewardship program effective on ameliorating irrational antibiotic use in China? Study on the antibiotic use of specialized hospitals in China in 2011–2012. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 34, 456–463 (2014). https://doi.org/10.1007/s11596-014-1300-6
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-014-1300-6