Abstract
Background
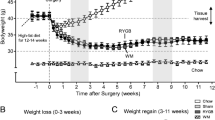
Weight regain and type-2 diabetes relapse has been reported in a significant proportion of vertical sleeve gastrectomy (VSG) patients in some studies, but definitive conclusions regarding the long-term comparative effectiveness of VSG and Roux-en-Y gastric bypass (RYGB) surgery are lacking both in humans and rodent models. This study’s objective was to compare the effects of murine models of VSG and RYGB surgery on body weight, body composition, food intake, energy expenditure, and glycemic control.
Methods
VSG, RYGB, and sham surgery was performed in high-fat diet-induced obese mice, and the effects on body weight and glycemic control were observed for a period of 12 weeks.
Results
After the initial weight loss, VSG mice regained significant amounts of body weight and fat mass that were only marginally lower than in sham-operated mice. In contrast, RYGB produced sustained loss of body weight and fat mass up to 12 weeks and drastically improved fasting insulin and HOMA-IR compared with sham-operated mice. Using weight-matched control groups, we also found that the adaptive hypometabolic response to weight loss was blunted by both VSG and RYGB, and that despite large weight/fat regain, fasting insulin and HOMA-IR were markedly improved, but not reversed, in VSG mice.
Conclusions
VSG is less effective to lastingly suppress body weight and improve glycemic control compared with RYGB in mice. Given similar observations in many human studies, the run towards replacing RYGB with VSG is premature and should await carefully controlled randomized long-term trials with VSG and RYGB.






Similar content being viewed by others
References
Busetto L. Timing of bariatric surgery in people with obesity and diabetes. Ann Transl Med. 2015;3(7):94.
Cohen RV, Neto MG, Correa JL, et al. A pilot study of the duodenal-jejunal bypass liner in low body mass index type 2 diabetes. J Clin Endocrinol Metab. 2013;98(2):E279–82.
Rubino F, Cummings DE. Surgery: the coming of age of metabolic surgery. Nat Rev Endocrinol. 2012;8(12):702–4.
Haruta H, Kasama K, Ohta M, et al. long-term outcomes of bariatric and metabolic surgery in Japan: results of a multi-institutional survey. Obes Surg. 2017;27(3)754–62.
Debs T, Petrucciani N, Kassir R, et al. Gugenheim J. Trends of bariatric surgery in France during the last 10 years: analysis of 267,466 procedures from 2005–2014. Surg Obes Relat Dis. 2016;12(8):1602–09.
Beaulac J, Sandre D. Critical review of bariatric surgery, medically supervised diets, and behavioural interventions for weight management in adults. Perspect. Public Health. 2016. doi:10.1177/1757913916653425.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes--3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Froylich D, Corcelles R, Daigle C, et al. Effect of Roux-en-Y gastric bypass and sleeve gastrectomy on nonalcoholic fatty liver disease: a comparative study. Surg Obes Relat Dis. 2016;12(1):127–31.
Praveenraj P, Gomes RM, Kumar S, et al. Comparison of weight loss outcomes 1 year after sleeve gastrectomy and Roux-en-Y gastric bypass in patients aged above 50 years. J Minim Access Surg. 2016;12(3):220–5.
Celio AC, Wu Q, Kasten KR, et al.Comparative effectiveness of Roux-en-Y gastric bypass and sleeve gastrectomy in super obese patients. Surg Endosc. 2017;31(1):317–23.
Lager CJ, Esfandiari NH, Subauste AR, et al. Roux-En-Y gastric bypass vs. sleeve gastrectomy: balancing the risks of surgery with the benefits of weight loss. Obes Surg. 2017;27(1):154–61.
Kansou G, Lechaux D, Delarue J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass: one year outcomes. Int J Surg. 2016;33(Pt A):18–22.
Maffazioli GD, Stanford FC, Campoverde Reyes KJ, et al. Comparing outcomes of two types of bariatric surgery in an adolescent obese population: Roux-en-Y gastric bypass vs. Sleeve Gastrectomy Front Pediatr. 2016;4:78.
Lee WJ, Chong K, Aung L, et al. Metabolic surgery for diabetes treatment: sleeve gastrectomy or gastric bypass? World J Surg. 2017;41(1):216–23.
Osland E, Yunus RM, Khan S, et al. Diabetes improvement and resolution following laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a systematic review of randomized controlled trials. Surg Endosc. 2017;31(4):1952–63.
Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–55.
Felsenreich DM, Langer FB, Kefurt R, et al. Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(9):1655–62.
Kalarchian M, Turk M, Elliott J, et al. Lifestyle management for enhancing outcomes after bariatric surgery. Curr Diab Rep. 2014;14(10):540.
Hao Z, Mumphrey MB, Townsend RL, et al. Body composition, food intake, and energy expenditure in a murine model of Roux-en-y gastric bypass surgery. Obes Surg. 2016;26(9):2173–82.
Mokadem M, Zechner JF, Margolskee RF, et al. Effects of Roux-en-Y gastric bypass on energy and glucose homeostasis are preserved in two mouse models of functional glucagon-like peptide-1 deficiency. Mol Metab. 2014;3(2):191–201.
Liou AP, Paziuk M, Luevano Jr JM, et al. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5(178):178ra41.
Flynn CR, Albaugh VL, Cai S, et al. Bile diversion to the distal small intestine has comparable metabolic benefits to bariatric surgery. Nat Commun. 2015;6:7715.
Chambers AP, Kirchner H, Wilson-Perez HE, et al. The effects of vertical sleeve gastrectomy in rodents are ghrelin independent. Gastroenterology 2013;144(1):50-52.
Arble DM, Sandoval DA, Turek FW, et al. Metabolic effects of bariatric surgery in mouse models of circadian disruption. Int J Obes. 2015;39(8):1310–8.
Ryan KK, Tremaroli V, Clemmensen C, et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014;509(7499):183–8.
Hao Z, Zhao Z, Berthoud HR, et al. Development and verification of a mouse model for roux-en-Y gastric bypass surgery with a small gastric pouch. PLoS One. 2013;8(1):e52922.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Ding L, Sousa KM, Jin L, et al. Vertical sleeve gastrectomy activates GPBAR-1/TGR5 to sustain weight loss, improve fatty liver, and remit insulin resistance in mice. Hepatology. 2016;64(3):760–73.
McGavigan AK, Garibay D, Henseler ZM, et al. TGR5 contributes to glucoregulatory improvements after vertical sleeve gastrectomy in mice. Gut 2017;66(2):226–34.
Myronovych A, Kirby M, Ryan KK, et al. Vertical sleeve gastrectomy reduces hepatic steatosis while increasing serum bile acids in a weight-loss-independent manner. Obesity (Silver Spring). 2014;22(2):390–400.
Aminian A, Brethauer SA, Andalib A, et al. Can sleeve gastrectomy "cure" diabetes? Long-term metabolic effects of sleeve gastrectomy in patients with type 2 diabetes. Ann Surg. 2016;264(4):674–81.
Figura A, Rose M, Ordemann J, et al. Changes in self-reported eating patterns after laparoscopic sleeve gastrectomy: a pre-post analysis and comparison with conservatively treated patients with obesity. Surg Obes Relat Dis. 2017;13(2):129–37.
Disse E, Pasquer A, Pelascini E, et al. Dilatation of sleeve gastrectomy: myth or reality? Obes Surg. 2017;27(1):30–37.
Ferrer-Marquez M, Garcia-Diaz JJ, Moreno-Serrano A, et al. Changes in gastric volume and their implications for weight loss after laparoscopic sleeve gastrectomy. Obes. Surg. 2017;27(2):303–9.
Das SK, Roberts SB, McCrory MA, et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr. 2003;78(1):22–30.
Dirksen C, Jorgensen NB, Bojsen-Moller KN, et al. Gut hormones, early dumping and resting energy expenditure in patients with good and poor weight loss response after Roux-en-Y gastric bypass. Int J Obes. 2013;37(11):1452–9.
Tam CS, Redman LM, Greenway F, et al. Energy metabolic adaptation and cardiometabolic improvements one year after gastric bypass, sleeve gastrectomy, and gastric band. J Clin Endocrinol Metab. 2016;101(10):3755–64.
Butte NF, Brandt ML, Wong WW, et al. Energetic adaptations persist after bariatric surgery in severely obese adolescents. Obesity (Silver Spring). 2015;23(3):591–601.
Sista F, Abruzzese V, Clementi M, et al. The effect of sleeve gastrectomy on GLP-1 secretion and gastric emptying: a prospective study. Surg Obes Relat Dis. 2017;13(1):7–14.
Aminian A, Jamal M, Augustin T, et al. Failed surgical weight loss does not necessarily mean failed metabolic effects. Diabetes Technol Ther. 2015;17(10):682–4.
Sjoholm K, Sjostrom E, Carlsson LM, et al. Weight change-adjusted effects of gastric bypass surgery on glucose metabolism: 2- and 10-year results from the Swedish obese subjects (SOS) study. Diabetes Care. 2016;39(4):625–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Animal Rights
Animal care and experimentation was approved by the Pennington Biomedical Research Center Institutional Animal Care and Use Committee and strictly followed rules and guidelines provided by the American Physiological Society and NIH.
Funding
This work was supported by National Institutes of Health grant DK047348 (HRB) and P20-RR021945 (COBRE Phenotyping Core). CDM was supported by National Institutes of health grant DK081563. HM was supported by National Institutes of Health grant DK092587.
Electronic supplementary material
ESM 1
(DOCX 612 kb)
Rights and permissions
About this article
Cite this article
Hao, Z., Townsend, R., Mumphrey, M.B. et al. RYGB Produces more Sustained Body Weight Loss and Improvement of Glycemic Control Compared with VSG in the Diet-Induced Obese Mouse Model. OBES SURG 27, 2424–2433 (2017). https://doi.org/10.1007/s11695-017-2660-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2660-3