Abstract
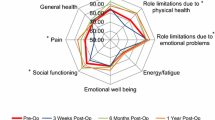
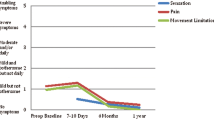
Laparoscopic TAPP inguinal hernia repair is an established alternative to open hernia repair, which offers equivalent outcomes with less postoperative pain and faster recovery. Unfortunately, it remains technically challenging, requiring advanced laparoscopic skills which have limited its popularity among surgeons. The robotic platform has the potential to overcome these challenges. The objective of this study was to examine the long-term quality of life and outcomes following robotic assisted TAPP inguinal hernia repair, since these data have not been reported up to now. From October 2012 to October 2015, 159 inguinal hernias in 82 consecutive patients were repaired with 3D mesh (BARD) using da Vinci Si Surgical System (Intuitive Surgical, Sunnyvale, CA, USA). The patients’ demographics and intraoperative data were documented. Patients were seen 2 and 6 weeks after the surgery and the complications were recorded. Patients were assessed 6 weeks after the surgery by a survey using a universal pain assessment tool to document their post-operative pain, narcotic use and time of return to work and exercise. A modified short form 12 (SF 12) was also sent out to the patients 12–36 months after the surgery to measure their health-related quality of life prior to surgery and at the 12- to 36-month follow-up, and to document any evidence of recurrence. Postoperative health-related quality of life scores were compared to the pre-operative baseline quality of life scores using the unpaired t test. Over the course of 3 years, 159 robotic assisted TAPP inguinal hernia repair were performed in 82 patients, 73 men and 9 women by one surgeon as an outpatient basis. The mean age was 53 and mean body mass index was 26. There were no intraoperative complications or conversions. The average operative time was 99 min. Four patients developed urinary retention post-operatively and one patient developed postoperative bowel obstruction requiring laparoscopic lysis of adhesion with no long-term complications. All patients completed the pain assessment survey and the median pain score, 3 days after the surgery was 3. Narcotics were used for an average of 3.1 days. The modified SF 12 survey assessing for quality of life before and 12–36 months after surgery was completed and returned by 29 patients (response rate of 35.4% and median follow-up of 32 months). Only one recurrence was reported which was repaired with open technique. The analysis of the SF 12 survey that evaluated patient’s quality of life, pain score and the ability to perform activities of daily living before and after surgery revealed a significant improvement in those measures 12–36 months after the surgery compare to their baseline. Hernia recurrence, chronic pain and physical impairment are the major long-term concerns after any type of inguinal hernia repair. Our results demonstrate that robotic assisted TAPP inguinal hernia repair appears to be a technically feasible, reproducible and safe minimally invasive alternative with low recurrence, low chronic pain and high health-related quality of life in the long term.















Similar content being viewed by others
References
Bittner R, Schwarz J (2012) Inguinal hernia repair: current surgical techniques. Langenbecks Arch Surg 397:271–282
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Wellwood J, Sculpher MJ, Stoker D et al (1998) Randomized controlled trial of laparoscopic versus open hernia repair for inguinal hernia: outcome and cost. Br Med J 317:103–110
Wauschkuhn CA, Schwarz J, Boekeler U, Bitter R (2010) Laparoscopic inguinal hernia repair: gold standard in bilateral hernia repair? Result of more than 2800 patients in comparison to literature. Surg Endosc 24:3026–3030
Trevisonno M, Kaneva P, Watanabe Y, Fried GM, Feldman LS, Andalib A, Vassiliou MC (2015) Current practices of laparoscopic inguinal hernia repair: a population-based analysis. Hernia 19(5):725–733. doi:10.1007/s10029-015-1358-5 (Epub 2015 Mar 10)
Kudsi OY, McCarty JC, Paluvoi N, Mabardy AS (2017) Transition from laparoscopic totally extraperitoneal inguinal hernia repair to robotic transabdominal preperitoneal inguinal hernia repair: a retrospective review of a single surgeon’s experience. World J Surg. doi:10.1007/s00268-017-3998-3 (Epub ahead of print)
Arcerito M, Changchien E, Bernal O, Konkoly-Thege A, Moon J (2016) Robotic inguinal hernia repair: technique and early experience. Am Surg 82(10):1014–1017
Escobar Dominguez JE, Ramos MG, Seetharamaiah R, Donkor C, Rabaza J, Gonzalez A (2016) Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endosc 30(9):4042–4048. doi:10.1007/s00464-015-4717-5 (Epub 2015 Dec 30)
Ito F, Jarrard D, Gould JC (2008) Transabdominal preperitoneal robotic inguinal hernia repair. J Laparoendosc Adv Surg Tech A 18(3):397–399
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (international Endohernia Society [IEHS]). Surg Endosc 25:2773–2843
GraphPad QuickCalcs: T Test Calculator Web 1 Jan 2017
Ger R, Monrroe K, Duvivier R (1990) Management of indirect inguinal hernia by laparoscopic closure of the neck of the sac. Am J Surg 159:370–373
Van Den Heuvel B, Beudeker N, Van Den Broek J, Bogte A, Dwars BJ (2013) The incidence and natural course of occult inguinal hernia during TAPP repair: Repair is beneficial. Surg Endoscopy 27:4142–4146
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Andrew Iraniha M.D, FACS, and Author Joshua Peloquin D. O declare they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Iraniha, A., Peloquin, J. Long-term quality of life and outcomes following robotic assisted TAPP inguinal hernia repair. J Robotic Surg 12, 261–269 (2018). https://doi.org/10.1007/s11701-017-0727-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-017-0727-8