Abstract
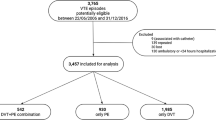
Venous thromboembolism (VTE) is the third most common cardiovascular disease. Real-life data on the clinical presentation, risk factors, diagnosis, and treatment of VTE in Italy and Europe are required to optimize the management of this disease. The PREFER in VTE registry, a prospective non-interventional real-life study, was designed to assess clinical characteristics and management of patients with VTE, use of health care resources, and on-treatment patient quality of life. Eligible consecutive patients with objectively diagnosed VTE were enrolled in the registry and followed up for 12 months. Between January and December 2013, 816 Italian and 1027 patients from 6 European countries other than Italy (European patients) were enrolled in the registry, and followed up until December 2014. Italian patients were the oldest (mean age 65.7 years) among the European patients. The Italian patients with a history of cancer were 24.6 % of whom 63.2 % had an active cancer (18.2 and 57.0 %, respectively, in Europe). Parenteral heparin was given, as initial treatment, in 73.8 % of Italian patients (66.4 % in Europe); VKA in combination with other treatments in 45.8 % (34.7 % in Europe); and VKA as the only anticoagulant treatment in 24.4 % (17.2 % in Europe). Of the Italian patients, 43.2 and 90.6 % of patients were hospitalized for deep vein thrombosis and pulmonary embolism, respectively; 65.4 % were admitted to the hospital through the emergency department. Following a real world approach, PREFER in VTE shows that the Italian patients, among and compared to the European patients, are the oldest, have a history of cancer more commonly, receive an initial treatment with heparin more commonly, and are more commonly hospitalized, particularly if affected by PE.





Similar content being viewed by others
References
Piazza G, Goldhaber SZ (2010) Venous thromboembolism and atherothrombosis: an integrated approach. Circulation 121(19):2146–2150
Cohen AT, Agnelli G, Anderson FA, VTE Impact Assessment Group in Europe (VITAE) et al (2007) Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost 98:756–764
Kahn SR, Ginsberg JS (2004) Relationship between deep venous thrombosis and the post-thrombotic syndrome. Arch Intern Med 164(1):17–26
Kahn SR, Comerota AJ, Cushman M, American Heart Association Council on Peripheral Vascular Disease, Council on Clinical Cardiology, and Council on Cardiovascular and Stroke Nursing et al (2014) The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation 130:1636–1661
Pengo V, Lensing AW, Prins MH, Thromboembolic Pulmonary Hypertension Study Group et al (2004) Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med 350(22):2257–2264
Kearon C, Akl EA, Comerota AJ, American College of Chest Physicians et al (2012) Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of Thrombosis. 9th ed: American College of Chest Physicians Evidence-based clinical practise Guidelines. Chest 141:e419S–e494S
Nieto JA, Solano R, Ruiz-Ribó MD, Riete Investigators et al (2010) Fatal bleeding in patients receiving anticoagulant therapy for venous thromboembolism: findings from the RIETE registry. J Thromb Haemost 8(6):1216–1222
Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ (2008) Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 133(6Suppl):454S–545S (8 Edition)
Ansell J, Hirsh J, Hylek E, Jacobseon A, Crowther M, Palareti G (2008) Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 133(6Suppl):160S–198S (8th Edition)
Büller HR, Décousus H, Grosso MA et al (2013) Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 369(15):1406–1415
Schulman S, Kearon C, Kakkar AK et al (2009) Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 361(24):2342–2352
Agnelli G, Buller HR, Cohen A et al (2013) Apixaban for extended treatment of venous thromboembolism. N Engl J Med 368(8):699–708
Büller HR, Prins MH, Lensin AW et al (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366(14):1287–1297
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors: Giuseppe De Bartolomeo, Francesco Guercini, Davide Imberti, Valeria Mommi and Chiara Tonello declare that they have no conflict of interest regarding this article. Giuseppe Camporese has been a member of Daiichi-Sankyo Italy Advisory Board. Raffaella Benedetti has received research grants from Portola, Astrazeneca, Boehringer Ingelheim; and has received speaker honorarium from Bayer, Boehringer Ingelheim, Sanofi. Giancarlo Agnelli reports receiving personal fees from Boehringer Ingelheim, Sanofi, Daiichi-Sankyo, Bayer, Pfizer and Bristol-Myers Squibb.
Funding
This study was funded by Daiichi Sankyo Europe GmbH.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Appendix 1
Appendix 1
International Steering Committee—PREFER in VTE
Giancarlo Agnelli, Alexander T. Cohen, Anselm K. Gitt, Rupert Bauersachs, Eva-Maria Fronk, Petra Laeis, Patrick Mismetti, Manuel Monreal, Stefan N. Willich, Wolf-Peter. The list of the Italian centers and principal local investigators of the study are shown in Table 2.
Rights and permissions
About this article
Cite this article
Guercini, F., Mommi, V., Camporese, G. et al. The management of patients with venous thromboembolism in Italy: insights from the PREFER in VTE registry. Intern Emerg Med 11, 1095–1102 (2016). https://doi.org/10.1007/s11739-016-1507-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1507-6