Abstract
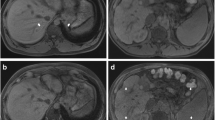
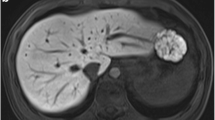
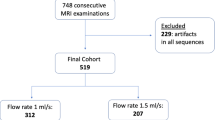
This study aimed to compare the uniformity of fat suppression and image quality between liver acquisition with volume acceleration flex (LAVA-Flex) and LAVA on 60-cm conventional-bore and 70-cm wide-bore 3.0-T magnetic resonance imaging (MRI). The uniformity of fat suppression by LAVA-Flex and LAVA was assessed as the efficiency of suppression of superficial fat at the levels of the liver dome, porta, and renal hilum. Percentage standard deviation (%SD) was calculated using the following equation: %SD (%) = 100 × SD of the regions of interest (ROIs)/mean value of the signal intensity (SI) in the ROIs. Signal-to-noise ratio (SNR) and contrast ratio (CR) were calculated. In the LAVA sequence, the %SD in all slices on wide-bore 3.0-T MRI was significantly higher than that on conventional-bore 3.0-T MRI (P < 0.01). However, there was no significant difference in fat signal uniformity between the conventional and wide-bore scanners when LAVA-Flex was used. In the liver, there were no significant differences in SNR between the two sequences. However, the SNR in the pancreas was lower for the wide-bore scanner than for the conventional-bore scanner for both sequences (P < 0.05). There were no significant differences in CR for the liver and fat between LAVA-Flex and LAVA in both scanners. The CR in the LAVA-Flex images obtained by wide-bore MRI was significantly higher than that in the LAVA-Flex images recorded by conventional-bore MRI (P < 0.001). LAVA-Flex offers more homogenous fat suppression in the upper abdomen than LAVA for both conventional and wide-bore 3.0-T MRI.




Similar content being viewed by others
References
Lu DS, Saini S, Hahn PF, Goldberg M, Lee MJ, Weissleder R, et al. T2-weighted MR imaging of the upper part of the abdomen: should fat suppression be used routinely? AJR Am J Roentgenol. 1994;162:1095–100. doi:10.2214/ajr.162.5.8165989.
Semelka RC, Chew W, Hricak H, Tomei E, Higgins CB. Fat-saturation MR imaging of the upper abdomen. AJR Am J Roentgenol. 1990;155:1111–6. doi:10.2214/ajr.155.5.2120945.
Beddy P, Rangarajan RD, Kataoka M, Moyle P, Graves MJ, Sala E. T1-weighted fat-suppressed imaging of the pelvis with a dual-echo Dixon technique: initial clinical experience. Radiology. 2011;258:583–9. doi:10.1148/radiol.10100912.
Kier R, Smith RC, McCarthy SM. Value of lipid- and water-suppression MR images in distinguishing between blood and lipid within ovarian masses. AJR Am J Roentgenol. 1992;158:321–5. doi:10.2214/ajr.158.2.1729791.
Kaldoudi E, Williams SC, Barker GJ, Tofts PS. A chemical shift selective inversion recovery sequence for fat-suppressed MRI: theory and experimental validation. Magn Reson Imaging. 1993;11:341–55.
Foo TK, Sawyer AM, Faulkner WH, Mills DG. Inversion in the steady state: contrast optimization and reduced imaging time with fast three-dimensional inversion-recovery-prepared GRE pulse sequences. Radiology. 1994;191:85–90. doi:10.1148/radiology.191.1.8134602.
Del Grande F, Santini F, Herzka DA, Aro MR, Dean CW, Gold GE, et al. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics. 2014;34:217–33. doi:10.1148/rg.341135130.
Bley TA, Wieben O, Francois CJ, Brittain JH, Reeder SB. Fat and water magnetic resonance imaging. J Magn Reson Imaging. 2010;31:4–18. doi:10.1002/jmri.21895.
Dixon WT. Simple proton spectroscopic imaging. Radiology. 1984;153:189–94. doi:10.1148/radiology.153.1.6089263.
Mito S, Ishizaka K, Nakanishi M, Sugimori H, Hamaguchi H. Tsuzuki T [Comparison of fat suppression techniques of bilateral breast dynamic sequence at 3.0 T: utility of three-point DIXON technique]. Nihon Hoshasen Gijutsu Gakkai zasshi. 2011;67:654–60.
Ishizaka K, Oyama N, Mito S, Sugimori H, Nakanishi M, Okuaki T, et al. Comparison of 1H MR spectroscopy, 3-point DIXON, and multi-echo gradient echo for measuring hepatic fat fraction. Magn Reson Med Sci MRMS Off J Japan Soc Magn Reson Med. 2011;10:41–8.
Ma J, Wehrli FW, Song HK, Hwang SN. A single-scan imaging technique for measurement of the relative concentrations of fat and water protons and their transverse relaxation times. J Magn Reson. 1997;125:92–101. doi:10.1006/jmre.1996.1086.
Ma J. Breath-hold water and fat imaging using a dual-echo two-point Dixon technique with an efficient and robust phase-correction algorithm. Magn Reson Med Off J Soc Magn Reson Med/Soc Magn Reson Med. 2004;52:415–9. doi:10.1002/mrm.20146.
Li XH, Zhu J, Zhang XM, Ji YF, Chen TW, Huang XH, et al. Abdominal MRI at 3.0 T: LAVA-Flex compared with conventional fat suppression T1-weighted images. J Magn Reson Imaging. 2014;40:58–66. doi:10.1002/jmri.24329.
Harris LM, Robinson J, Menzies RG. Evidence for fear of restriction and fear of suffocation as components of claustrophobia. Behav Res Ther. 1999;37:155–9.
Bangard C, Paszek J, Berg F, Eyl G, Kessler J, Lackner K, et al. MR imaging of claustrophobic patients in an open 1.0T scanner: motion artifacts and patient acceptability compared with closed bore magnets. Eur J Radiol. 2007;64:152–7. doi:10.1016/j.ejrad.2007.02.012.
Arepally A, Karmarkar PV, Qian D, Barnett B, Atalar E. Evaluation of MR/fluoroscopy-guided portosystemic shunt creation in a swine model. J Vasc Interv Radiol JVIR. 2006;17:1165–73. doi:10.1097/01.RVI.0000228493.07075.FC.
Stattaus J, Maderwald S, Forsting M, Barkhausen J, Ladd ME. MR-guided core biopsy with MR fluoroscopy using a short, wide-bore 1.5-Tesla scanner: feasibility and initial results. J Magn Reson Imaging. 2008;27:1181–7. doi:10.1002/jmri.21075.
Nakazawa H, Komori M, Shibamoto Y, Takikawa Y, Mori Y, Tsugawa T. Geometric accuracy in three-dimensional coordinates of Leksell stereotactic skull frame with wide-bore 1.5-T MRI compared with conventional 1.5-T MRI. J Med Imaging Radiat Oncol. 2014;58:595–600. doi:10.1111/1754-9485.12225.
Kandpal H, Sharma R, Madhusudhan KS, Kapoor KS. Respiratory-triggered versus breath-hold diffusion-weighted MRI of liver lesions: comparison of image quality and apparent diffusion coefficient values. AJR Am J Roentgenol. 2009;192:915–22. doi:10.2214/AJR.08.1260.
Takayama Y, Nishie A, Asayama Y, Ishigami K, Kakihara D, Ushijima Y, et al. Optimization and clinical feasibility of free-breathing diffusion-weighted imaging of the liver: comparison with respiratory-triggered diffusion-weighted imaging. Magn Reson Med Sci. 2015;. doi:10.2463/mrms.2014-0032.
Ragan DK, Bankson JA. Two-point Dixon technique provides robust fat suppression for multi-mouse imaging. J Magn Reson Imaging. 2010;31:510–4. doi:10.1002/jmri.22060.
Cornfeld DM, Israel G, McCarthy SM, Weinreb JC. Pelvic imaging using a T1 W fat-suppressed three-dimensional dual echo Dixon technique at 3T. J Magn Reson Imaging. 2008;28:121–7. doi:10.1002/jmri.21402.
Ream JM, Rosenkrantz AB. Advances in T1-Weighted and T2-Weighted Imaging in the Abdomen and Pelvis. Radiol Clin North Am. 2015;53:583–98. doi:10.1016/j.rcl.2015.01.003.
Ding Y, Rao SX, Chen CZ, Li RC, Zeng MS. Usefulness of two-point Dixon fat-water separation technique in gadoxetic acid-enhanced liver magnetic resonance imaging. World J Gastroenterol. 2015;21:5017–22. doi:10.3748/wjg.v21.i16.5017.
Costelloe CM, Madewell JE, Kundra V, Harrell RK, Bassett RL Jr, Ma J. Conspicuity of bone metastases on fast Dixon-based multisequence whole-body MRI: clinical utility per sequence. Magn Reson Imaging. 2013;31:669–75. doi:10.1016/j.mri.2012.10.017.
Acknowledgments
This work was supported by Grants-in-Aid for Scientific Research (Kakenhi, No. 24300167 and No. 26870339) from the Japan Society for the Promotion of Science (JSPS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no financial or commercial conflicts of interest.
About this article
Cite this article
Saito, S., Tanaka, K. & Hashido, T. Liver acquisition with volume acceleration flex on 70-cm wide-bore and 60-cm conventional-bore 3.0-T MRI. Radiol Phys Technol 9, 154–160 (2016). https://doi.org/10.1007/s12194-015-0344-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-015-0344-z