Abstract
Background
Sleep disorders are very common in migrants and refugees, often as a comorbid disorder to different somatic or psychiatric diagnoses and psychological disturbances such as metabolic syndrome, post-traumatic stress disorder, depression, and anxiety disorders.
Objectives
To review published prevalence rates as well as possible predictors for sleep disturbances in these vulnerable groups, including pre-migration stress, acculturation, and trauma before, during, and after migration, integration, and lifestyle in the host country with implications for predictive, preventive, and personalized medical approach (3PM).
Data sources
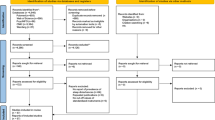
Electronic databases PubMed, PsycInfo, and Web of Knowledge were searched using (combined) search terms “migrant,” “asylum seeker,” “refugee,” “sleep disturbances,” “sleep disorder,” “insomnia,” and “sleep wake disorder.”
Study eligibility criteria
Peer-reviewed studies from 2000 to 2018 reporting data on prevalence and/or predictors of any measure of sleep disturbance were included.
Participants
Studies on international migrants and refugees, as well as internally displaced populations, were included.
Methods
We conducted a systematic review on the topic of sleep disorders in migrant and refugee populations. Only published articles and reviews in peer-reviewed journals were included.
Results
We analyzed five studies on sleep disorders in migrants, five studies on adult refugees, and three on refugee children and adolescents. Prevalence of sleep disorders in migrants and refugees ranges between 39 and 99%. In migrant workers, stress related to integration and adaptation to the host society is connected to higher risks of snoring, metabolic diseases, and insomnia. Sleep disturbances in refugees are predicted by past war experience. Sleep difficulties in adult and child refugees are strongly correlated to trauma. Torture of parents and grandparents can predict sleep disorders in refugee children, while being accompanied by parents to the host country has a protective effect on children’s sleep.
Conclusions and implications
Considering the differences in risk factors, vulnerability, and traumatic life events for different migrant populations, origins of sleep difficulties vary, depending on the migrant populations. Effects on sleep disturbances and sleep quality may be a result of integration in the host country, including changes of lifestyle, such as diet and working hours with implication for OSAS (obstructive sleep apnea) and insomnia. Compared with migrant populations, sleep disturbances in refugee populations are more correlated with mental health symptoms and disorders, especially PTSD (post-traumatic stress disorder), than with psychosocial problems. In juvenile refugee populations, psychological problems and disturbed sleep are associated with traumatic experiences during their journey to the host country. Findings highlight the need for expert recommendations for development of 3P approach stratified in the following: (1) prediction, including structured exploration of predisposing and precipitating factors that may trigger acute insomnia, screening of the according sleep disorders by validated translated questionnaires and sleep diaries, and a face-to-face or virtual setting and screening of OSAS; (2) target prevention by sleep health education for female and male refugees and migrant workers, including shift workers; and (3) personalized medical approach, including translated cognitive behavioral treatment for insomnia (CBT-I) and imagery rehearsal therapy for refugees and telehealth programs for improved CPAP adherence in migrants, with the goal to enable better sleep health quality and improved health economy.

Similar content being viewed by others
References
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79.
Spielman AJ, Glovinsky P. The varied nature of insomnia. In: Hauri PJ, editor. Case studies in insomnia. New York: Plenum Press; 1991.
Richter K, Peter L, Lehfeld H, Zäske H, Brar-Reissinger S, Niklewski G. Prevalence of psychiatric diagnoses in asylum seekers with follow-up. BMC Psychiatry. 2018;18(1):206.
Depner CM, Stothard ER, Wright KP. Metabolic consequences of sleep and circadian disorders. Curr Diab Rep. 2014;14:507. https://doi.org/10.1007/s11892-014-0507-z.
Knauert M, Sreelatha N, Boyd Gillespie M, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg. 2015;1(1):17–27. https://doi.org/10.1016/j.wjorl.2015.08.001.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23 eCollection 2016. Review.
Basishvili T, Eliozishvili M, Maisuradze L, Lortkipanidze N, Nachkebia N, Oniani T, et al. Insomnia in a displaced population is related to war-associated remembered stress. Stress Health. 2012. https://doi.org/10.1002/smi.1421.
Modesti PA, Calabrese M, Perruolo E, Bussotti A, Malandrino D, Bamoshmoosh M, et al. Sleep history and hypertension burden in first-generation Chinese migrants settled in Italy. The Chinese In Prato Cross-Sectional Survey. Medicine. 2016. https://doi.org/10.1097/MD.0000000000003229.
Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic Paradox. Sleep. 2011. https://doi.org/10.5665/SLEEP.1154.
Sandberg JC, Nguyen HT, Quandt SA, Chen H, Summers P, Walker FO, et al. Sleep quality among Latino farmworkers in North Carolina. Examination of the Job Control-Demand-Support Model. J Immigr Minor Health. 2016;18:532–41. https://doi.org/10.1007/s10903-015-0248-3.
Voss U, Tuin I. Integration of immigrants into a new culture is related to poor sleep quality. Health Qual Life Outcomes. 2008;6:1–6. https://doi.org/10.1186/1477-7525-6-61.
Hinton DE, Pich V, Chhean D, Pollack MH. The ghost pushes you down'. Sleep paralysis-type panic attacks in a Khmer refugee population. Transcult Psychiatry. 2005. https://doi.org/10.1177/1363461505050710.
Molsa M, Punamäki RL, Saarni SI, Tiilikainen M, Kuittinen S, Honkasalo ML. Mental and somatic health and pre- and post-migration factors among older Somali refugees in Finland. Transcult Psychiatry. 2014. https://doi.org/10.1177/1363461514526630.
Lies J, Drummond S. Prevalence study of sleep disturbance, mental health, and psychosocial concerns among asylum seekers and refugees. J Sleep Res. 2017. https://doi.org/10.1111/jsr.34_12619.
Sandahl H, Vindbjerg E, Carlsson J. Treatment of sleep disturbances in refugees suffering from post-traumatic stress disorder. Transcult Psychiatry. 2017. https://doi.org/10.1177/1363461517746314.
Thabet AAM, Abed Y, Vostanis P. Comorbidity of PTSD and depression among refugee children during war conflict. J Child Psychol Psychiatry. 2004. https://doi.org/10.1111/j.1469-7610.2004.00243.x.
Montgomery E, Foldspang A. Traumatic experience and sleep disturbance in refugee children from the Middle East. Eur J Pub Health. 2001;11(1):18–22.
Sandahl H, Jennum P, Baandrup L, Poschmann IS, Carlsson J. Treatment of sleep disturbances in trauma-affected refugees. Study protocol for a randomised controlled trial. Trials. 2017;18:1–13. https://doi.org/10.1186/s13063-017-2260-5.
Montgomery E. Trauma, exile and mental health in young refugees. Acta Psychiatr Scand Suppl. 2011. https://doi.org/10.1111/j.1600-0447.2011.01740.
Golubnitschaja O, Costigliola V. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European association for predictive, preventive and personalised medicine. EPMA J. 2012;3:14. https://doi.org/10.1186/1878-5085-3-14.
Golubnitschaja O, Costigliola V, Grech G. EPMA world congress: traditional forum in predictive, preventive and personalised medicine for multi-professional consideration and consolidation. EPMA J. 2017;8(Suppl):1–54. https://doi.org/10.1007/s13167-017-0108-4.
Razum O. Migration, Mortalitat und der healthy-migrant-Effekt. In: Richter M, Hurrelmann K, editors. Gesundheitliche Ungleichheit: VS Verlag für Sozialwissenschaften; 2006.
Wallace DM, Williams NJ, Sawyer AM, Jean-Louis G, Aloia MS, Vieira DL, et al. Adherence to positive airway pressure treatment among minority populations in the US: a scoping review. Sleep Med Rev. 2018;38:56–69. https://doi.org/10.1016/j.smrv.2017.04.002.
Golubnitschaja O, Kinkorova J, Costigliola V. EPMA summit 2014 under the auspices of the presidency of Italy in the EU: professional statements. EPMA J. 2015;6(1):4. https://doi.org/10.1186/s13167-015-0026-2.
Chiarenza A, Dauvrin M, Chiesa V, Baatout S, Verrept H. Supporting access to healthcare for refugees and migrants in European countries under particular migratory pressure. BMC Health Serv Res. 2019;19:513. https://doi.org/10.1186/s12913-019-4353-1.
Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006;20(7):567–90.
Polivka J Jr, Polivka J, Pesta M, et al. Risks associated with the stroke predisposition at young age: facts and hypotheses in light of individualized predictive and preventive approach. EPMA J. 2019;10(1):81–99. Published 2019 Feb 20. https://doi.org/10.1007/s13167-019-00162-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics statement
The study involves only review of literature without involving of human and/or animals. The authors have no ethical conflicts to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Richter, K., Baumgärtner, L., Niklewski, G. et al. Sleep disorders in migrants and refugees: a systematic review with implications for personalized medical approach. EPMA Journal 11, 251–260 (2020). https://doi.org/10.1007/s13167-020-00205-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-020-00205-2