Abstract
Poisoning is the second leading cause of injury-related fatality in the USA and the leading cause of cardiac arrest in victims under 40 years of age. The study objective was to define the electrocardiographic (ECG) predictors of adverse cardiovascular events (ACVE) complicating suspected acute poisoning (SAP). This was a case-control study in adults at three tertiary-care hospitals and one regional Poison Control Center. We compared 34 cases of SAP complicated by ACVE to 101 consecutive control patients with uncomplicated SAP. The initial ECG was analyzed for rhythm, intervals, QT dispersion, ischemia, and infarction. ECGs were interpreted by a cardiologist, blinded to study hypothesis and case data. Subjects were 48% male, with mean age 42 ± 19 years. In addition to clinical suspicion of poisoning in 100% of patients, routine toxicology screens were positive in 77%, most commonly for benzodiazepines, opioids, and/or acetaminophen. Neither the ventricular rate, the QRS duration, nor the presence of infarction predicted the risk of ACVE. However, the rhythm, QTc, QT dispersion, and presence of ischemia correlated with the risk of ACVE. Independent predictors of ACVE based on multivariable logistic regression were prolonged QTc, any non-sinus rhythm, ventricular ectopy, and ischemia. Recursive partitioning analysis identified very low risk criteria (94.1% sensitivity, 96.2% NPV) and high risk criteria (95% specificity). Among patients with SAP, the presence of QTc prolongation, QT dispersion, ventricular ectopy, any non-sinus rhythm, and evidence of ischemia on the initial ECG are strongly associated with ACVE.
Similar content being viewed by others
Introduction
Although poisoning is an infrequent cause of cardiac arrest in elderly patients, it is the leading cause of cardiac arrest in patients <40 years of age [1–4]. There are over two million suspected acute poisonings (SAP) reported to Poison Control Centers in the USA each year [1]. Poisoning, defined as exposure to any drug, chemical, or toxin that results in injury, is the second leading cause of injury-related fatality in the USA behind only motor-vehicle collisions [3]. Many recommendations for the emergency cardiovascular care of poisoned patients are based on expert consensus, not scientific evidence [4]. Additionally, because standard guidelines for emergency cardiovascular care may not be optimal for the management of acute poisoning and overdose, urgent consultation with a medical toxicologist or regional Poison Control Center is recommended by the American Heart Association, the American Academy of Clinical Toxicologists, and the American College of Emergency Physicians, for patients with cardiovascular toxicity [4–6]. In-hospital adverse cardiovascular events (ACVE) frequently complicate poisoning and include myocardial injury [7–11], shock [12], dysrhythmias [13–18], and cardiac arrest [4, 19–21]. We conducted the present study to define the electrocardiographic (ECG) factors associated with ACVE in poisoning, with emphasis on analysis of the QT interval. We hypothesized that occurrence of ECG abnormalities, including QTc prolongation and increased QT dispersion (QTD), would correlate with elevated risk of ACVE in patients with SAP.
Materials and Methods
In a case-control study, we first prospectively identified 34 cases of ACVE complicating SAP among referrals to one Poison Control Center over the 12-month period between July 1, 2006 and June 30, 2007. ACVE was defined as a composite endpoint that included shock (hypotension with vasopressor requirement), myocardial injury (elevation of serum cardiac troponin on at least one measurement), ventricular dysrhythmia (ventricular tachycardia or ventricular fibrillation), and cardiac arrest (loss of pulse requiring cardiopulmonary resuscitation). We then prospectively evaluated the records of 101 consecutive patients presenting to the emergency department with SAP who were severe enough to warrant bedside consultation with the medical toxicology service but were not complicated by ACVE.
The regional Poison Control Center involved in the study is an urban referral center with an annual referral volume of approximately 45,000 cases. The medical toxicology service affiliated with the Poison Control Center serves three teaching hospitals with an annual consult volume of approximately 500 cases. The study protocol was approved by the Institutional Review Boards of the New York City Department of Health and Mental Hygiene as well as the New York University School of Medicine with waiver of informed consent.
Selection of cases was from Poison Control Center referrals during the study period who suffered at least one ACVE (as defined above). Patients who suffered ACVE prior to the initial ECG were not included in the study (n = 3). Exclusion criteria were absence of an available copy of the presentation ECG, ocular or dermal exposures, withdrawal syndromes, and significant trauma or burns.
The protocol for case follow-up was daily telephone follow-up obtained by a team of rotating house staff and clinical fellows per routine Poison Control Center protocol. Upon occurrence of an ACVE, a fax copy of the presentation ECG was obtained by a study investigator and subsequently de-identified for later review.
Selection of control patients was from consecutive patients presenting to the Emergency Department (ED) with SAP who were severe enough to warrant bedside consultation with the medical toxicology service but were not complicated by ACVE. Control patients were referred from the EDs of three urban university teaching hospitals to ensure complete and valid collection of data. All controls underwent consultation from the Poison Control Center-affiliated medical toxicology service consisting of at least one clinical fellow supported by a board-certified medical toxicologist. Exclusion criteria were the same as that for cases (see above).
All control patients had evaluation for SAP including bedside history, physical examination, and performance of an ECG on presentation. A de-identified photocopy of the ECG was saved for further review.
Standardized data collection was obtained by a single trained abstractor who was blinded to final cardiologist interpretation of ECGs at the time of abstraction. Sources of data included Poison Control Center electronic records, consultation notes, and hospital medical records. Using a standardized data collection instrument, demographics (age, gender), history of exposure (intent, timing, toxin, etc.), and initial vital signs were recorded. In addition to confirmation of exposure by history, laboratory confirmation of exposures using routine toxicology screens was recorded, if available.
All 12-lead ECGs were performed during the initial ED presentation using a standard paper speed of 25 mm/s with standard lead positions. ECGs were interpreted by a cardiologist who was blinded to the study hypothesis and case data. Using a copy of the original ECG, evaluation of the initial rhythm and intervals, as well as the presence or absence of ventricular ectopy, ischemia (based on the presence of ST segment changes or T wave abnormalities in two or more adjacent leads), infarction (based on the presence of Q waves in two or more adjacent leads), and an R wave >3 mm in lead AVR (R avr) was performed [22].
QT interval was measured from the beginning of the QRS complex to the end of the T wave (defined as the return to T–P baseline). When U waves were present, the QT interval was measured as the nadir of the curve between T and U waves. QT intervals were corrected for heart rate (QTc) using the computer-generated value from Bazett’s correction equation (QT/RR1/2). “Long QTc” was defined using standard criteria as QTc ≥470 ms in females and ≥450 ms in males [23]. Additionally, a QTc cutoff of ≥500 ms regardless of gender was evaluated based on prior data suggesting utility of this cutpoint to predict adverse cardiovascular outcomes [24, 25].
QTD was defined as the difference between the longest and the shortest QT interval on a 12-lead ECG according to the optimal technique described by Malik and colleagues and was determined manually by a blinded cardiologist [26]. To ensure validity of QTD measurements, a random sampling of 10 ECGs underwent independent QTD interpretation by a second study investigator, and inter-rater reliability was assessed with kappa statistics. A QTD cutoff of 50 ms was chosen based on cutpoints previously derived in the available literature [26].
Descriptive statistics were performed when appropriate. Continuous variables were analyzed with the independent sample Student t test for parametric data. Categorical variables were analyzed using the chi-squared test or Fisher’s exact test when appropriate. Receiver operating characteristics (area under the curve or c statistic) of QT interval measurements (QTc, QTD) were analyzed and plotted. Odds ratios (OR) and 95% confidence intervals (CI) were calculated by univariate analysis. Significant variables from univariate analysis were included in a multivariable model, and logistic regression analysis was performed. Independent predictors from the logistic regression were used as dichotomous variables for recursive partitioning analysis to develop a risk stratification algorithm. All tests were two-sided, and a p value <0.05 were considered statistically significant. With an estimated 30% prevalence of prolonged QT in our control subjects [15, 23, 27], we estimated that the present study (101 controls, 34 cases) could detect a 2-fold increased risk effect from the predictor variable with 83.3% power and 3-fold increased risk with 100% power. Analyses were performed by SPSS version 14.0 (SPSS Inc., Chicago, IL) and STATA version 8.2 (STATA Corp., College Station, TX) software packages.
Results
Over the 12-month study period, 34 cases of ACVE (referred to the Poison Center from 18 hospitals) were compared to 101 control subjects (from the three Poison Center-affiliate base hospitals). Out of 34 cases, there were 19 patients with shock, 16 patients with myocardial injury, nine patients with dysrhythmias, and 15 patients with cardiac arrest (some cases had more than one outcome). Subjects were 48% male with a mean age of 42 ± 19 years. Cases were significantly older (t test p < 0.05) and had higher proportions of subjects with age over 55, hypertension history, and presentation of multidrug overdose (chi-squared p < 0.05). Baseline clinical characteristics of study subjects are summarized in Table 1.
In addition to history and clinical suspicion of at least one toxic exposure in 100% of patients, there was laboratory confirmation of at least one toxic exposure obtained in 77% of study patients. By history, the most common exposures were benzodiazepines (23 exposures, 17% of patients), opioids (21 exposures, 16% of patients), and acetaminophen (20 exposures, 15% of patients). There were 82 (61%) single exposures, of which the most common were acetaminophen (10 single exposures, 12% of patients), alcohols (eight single exposures, 10% of patients), and opioids (eight single exposures, 10% of patients). The only exposure class that was significantly associated with ACVE was opioids (OR 3.0, 95% CI 1.1–7.9, p = 0.025). Further information about the most common exposures is summarized in Table 2.
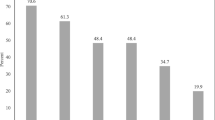
ECG variables for cases and controls are summarized in Table 3. Sinus rhythm was the most common presenting rhythm in both groups. The most common abnormal presenting rhythm was ventricular ectopy and that was observed in 26% of the cases and 9% of the control patients (p < 0.01). Cases were more likely to have ECG evidence of ischemia (p < 0.01), but evidence of infarction was nonsignificant. There was no difference in mean QRS duration between cases and controls. QTc interval was highly associated with ACVE using continuous (p = 0.02, see Fig. 1) and categorical variables for long QTc (p = 0.02) and QTc cutoff >500 ms (p < 0.01), observed in 68% and 41% of cases, respectively. QTD (see Fig. 2) was also highly associated with ACVE with a cutoff >50 ms (p = 0.02), observed in 79% of cases. Inter-observer agreement of the ability to reliably distinguish QTD >50 ms was verified using 10 randomly selected ECGs (k = 1.0, 95% CI 1.0–1.0).
Association of QTc with ACVE. This figure demonstrates a box-plot of QTc duration for patients with ACVE (cases) and controls. The box-plot represents the median, 25th and 75th quartiles, range, and outlying data points by a horizontal line, a box, vertical line, and dots, respectively. *Mean QTc was analyzed using the Student’s t test
Association of QT dispersion with ACVE. This figure demonstrates a box-plot of 12-lead QT dispersion for patients with ACVE (cases) and controls. The box-plot represents the median, 25th and 75th quartiles, range, and outlying data points by a horizontal line, a box, vertical line, and dots, respectively. *Mean QTD was analyzed using the Student’s t test
As a secondary analysis, ECG variables were analyzed for associations with individual components of the ACVE composite endpoint and the narrowed endpoint of just cardiac arrest or dysrhythmia. ECG findings associated with the narrowed endpoint (i.e., cardiac arrest or dysrhythmia), in ascending order of strength of association, were QRS > 120 ms (p < 0.05, OR = 4.0), QTc > 500 ms (p < 0.01, OR = 5.5), ectopy (p < 0.01, OR = 7.5), and non-sinus rhythm (p < 0.01, OR = 10.5). The ROC area under the curve (c-tatistic) to predict the narrowed endpoint (i.e., cardiac arrest or dysrhythmia) for QRS (c = 0.66, p < 0.05) and QTc (c = 0.67, p < 0.05) were also significant, while QTD only approached significance (c = 0.64, p = 0.07). ECG findings (e.g., QTc, QRS) associated with individual components of the ACVE composite outcome (i.e., shock, dysrhythmia, myocardial injury, cardiac arrest) are summarized in Table 4.
ROC curves for the ability of QTc and QTD to predict ACVE are represented in Figs. 3 and 4, respectively. Areas under the curve were similar for both measures (0.656 vs. 0.660), and each were statistically significant (p < 0.05). The optimal cutpoint for each was chosen based on the value that maximized the sum of sensitivity plus specificity; these values were QTc ≥ 504 ms (41.2% sensitivity, 88.1% specificity) and QTD ≥ 70 ms (58.8% sensitivity, 68.3% specificity). Test characteristics of QTc and QTD are summarized in Table 5.
ROC curve of QTc for prediction of adverse cardiovascular events. This figure demonstrates the ROC curve of QTc to predict ACVE. The area under the curve of 0.66 was statistically significant (95% CI 0.54–0.77). The cutpoint that maximized the sum of sensitivity and specificity was 504 ms. ACVE adverse cardiovascular events; CI confidence intervals; ROC receiver operating characteristics
ROC curve of QT dispersion for prediction of adverse cardiovascular events. This figure demonstrates the ROC curve of QTD to predict ACVE. The area under the curve of 0.66 was statistically significant (95% CI 0.55–0.76). The cutpoint that maximized the sum of sensitivity and specificity was 70 ms. ACVE adverse cardiovascular events; CI confidence intervals; QTD QT dispersion; ROC receiver operating characteristics
The multivariable model included significant factors from univariate analysis (see Table 6), including non-sinus rhythm (p < 0.01), ectopy (p < 0.01), QTc > 500 ms (p = 0.02), ischemia (p < 0.01), prolonged QTc (p < 0.01), and QTD > 50 ms (p = 0.02). Independent predictors of ACVE using adjusted odds ratios (OR) included the following: ectopy (OR 3.4, CI 1.0–13.4), non-sinus rhythm (OR 4.1, CI 1.3–9.7), QTc > 500 ms (OR 3.5, CI 1.3–9.4), long QTc (OR 3.1, CI 1.1–8.4), and evidence of ischemia (OR 3.5, CI 1.3–9.7).
Using independent predictors of ACVE (as dichotomous variables) based on the logistic regression (above), recursive partitioning analysis was performed for derivation of a decision tree to risk-stratify for ACVE. The number of decision nodes was predefined to a maximum of five or until ACVE risk was less than 5% in the final node. Presence of ectopy was a high-risk feature (ACVE in 9/14 or 64%). Any non-sinus rhythm (ACVE in 7/17 or 41%) and QTc ≥ 500 ms (ACVE in 8/21 or 38%) were both moderate risk features. Presence of long QTc (but less than 500 ms) yielded a low-risk group (ACVE in 8/31 or 26%). Absence of all of the above (i.e., no ectopy, sinus rhythm, normal QTc) yielded a very low-risk group (ACVE in 2/52 or 3.8%). The final recursive partitioning model for ACVE-risk stratification of patients with SAP is outlined in Fig. 5.
Risk stratification for adverse cardiovascular events in patients with suspected acute poisoning. Risk stratification scheme based on recursive partitioning analysis. *Long QTc was defined as ≥470 ms in females and ≥450 ms in males.23 ACVE adverse cardiovascular events; ms milliseconds; QTc corrected QT interval
Discussion
In this study, several characteristics of the presentation ECG were associated with in-hospital ACVE in patients with SAP. More specifically, analysis of the presenting rhythm, the QTc interval, and evidence of ischemia were the most useful for risk stratification. These findings demonstrate the clinical utility of the presentation ECG in the evaluation of patients with acute poisoning. The risk factors found to be most useful in this analysis were ectopy, non-sinus rhythm, QTc > 500 ms, long QTc, and evidence of ischemia.
These findings add substantially to the existing literature regarding the utility of the presentation ECG in the evaluation of acute poisoning. According to recently published guidelines from the American Heart Association, the approach to patients with symptoms of myocardial injury and a history of drug or toxin exposure should differ in both diagnostic evaluation and therapeutic management [10]. However, such guidelines currently rely upon expert consensus due to lack of adequate tools to risk-stratify poisoned patients. Our data address this deficiency by suggesting that the presentation ECG may aid prediction of cardiovascular complications in the setting of poisoning. This is the first study to our knowledge evaluating the use of the ECG to evaluate a diverse sample of patients with heterogeneous poisonings. We derived stratification criteria based on the initial ECG (ventricular ectopy, any non-sinus rhythm, and QTc prolongation) that estimate risk of ACVE on the basis of features of the initial ECG. If validated prospectively, these estimates of risk may help in making rational decisions about the appropriate level of medical care for patients with suspected poisoning.
Remarkably, little is known about the ECG predictors of cardiovascular complications in acute poisoning. It is thought that drug-induced vulnerability to ventricular dysrhythmias may be detected electrocardiographically by examination of the QT interval duration [18, 26]. QT prolongation pharmacologically occurs via three predominant mechanisms: slowed recovery from inactivation of Na+ channels [16], delayed inactivation of Na+ channels [27, 28], and K+ channel (e.g., rapid potassium rectifier current, or I Kr) blockade [29]. Detailed animal experiments show that prolongation of ventricular repolarization is a prerequisite for some ventricular dysrhythmias, particularly torsade de pointes (TdP) [30].
The QT interval has long been noted to vary among the individual 12 surface leads of the ECG, but increased inhomogeneity may occur during toxic exposures that alter repolarization timing. Through the development of conduction blocks and changes to the refractory periods within the atria and ventricles, increased dispersion of repolarization produces a myocardial substrate which is vulnerable to afterdepolarizations that can “trigger” lethal dysrhythmias [31–33]. Toxins that increase the dispersion of repolarization typically do so non-uniformly across the myocardium [34]. This phenomenon likely relates to the varying ion channel distribution within different myocardial layers and the dissimilar effects of toxins on these ion channels. The ECG metric typically used for detection of changes to the homogeneity of repolarization is measurement of QTD [26, 33].
Our data did not demonstrate an association between the QRS interval and ACVE; however, the secondary analysis did show an association between QRS >120 ms and VT/VF alone (p < 0.01, see Table 4). Previously, QRS >160 ms and the presence of R avr were demonstrated to predict dysrhythmia in patients with tricyclic antidepressant poisoning [13, 22, 35]. In contrast, we were unable to confirm the previous association between QRS duration and R avr with our primary outcome (i.e., ACVE). It should be noted that those associations exist in known TCA overdose, whereas the present study was designed for a heterogeneous group of suspected acute poisoning. Our data should in no way dissuade use of QRS duration and R avr to risk-stratify patients with known or suspected tricyclic toxicity.
Ectopy on the initial ECG was present in 26% of cases, one of the strongest ECG associations with ACVE (p < 0.001), and conferred significantly increased odds of ACVE (OR 3.4, CI 1.01–13.4) in the adjusted analysis. To investigate the role of digoxin (a known cause of ectopy) to explain these findings, we evaluated the 14 subjects with ectopy and of these, compared the three subjects with digoxin toxicity (one case and two controls) with the other 11 subjects without digoxin toxicity (eight cases and three controls). Running a Fisher’s exact test on this data revealed no significant difference between this proportion (p = 0.53). Thus, digoxin toxicity may have caused ectopy in only one case subject and did not explain the predictive power of ectopy for ACVE.
Further research is needed to define predictors of ACVE in poisoning. Because ACVE are remarkably difficult to predict among the large number of patients with SAP, there is uncertainty regarding the optimal utilization of hospital resources to monitor these patients. Often, patients assigned to monitored beds wait for prolonged periods of time in hospital EDs before monitored floor beds become available [36]. This situation leads to increased ED waiting times, overcrowding, and compromised patient care. Conversely, patients at risk for cardiovascular events may be admitted to unmonitored beds, transferred to an inpatient psychiatric service, or discharged home. Early risk assessment for poisoned patients is thus essential not only to prevent morbidity and mortality but also to improve hospital resource utilization.
Results of several large epidemiologic studies have yielded conflicting results about the relationship between QTc prolongation and sudden cardiac death [37]. In patients with cardiac disease, QTc prolongation predicts myocardial injury and TdP [24, 25]. Our data extend the predictive utility of QTc prolongation to a heterogeneous population of patients with suspected poisoning. In our population, we found that prolonged QTc as well as a QTc cutoff of ≥500 ms on the initial ECG were both independent predictors of ACVE. This finding must be tempered by the reported observation that the QT interval slightly increases with age [38]; given that the proportion of cases over 55 years of age was significantly higher than controls (see Table 1), the age-related QT interval increase may have confounded these QT data away from the null hypothesis. However, in their study of age-related effects on QT interval, Mangoni et al. compared a group with mean age 74 to a group with mean age 50 and found a mean QTc difference of 6 ms [38]. In contrast, the present study found the mean difference in QTc between cases and controls to be much larger (25 ms); thus, age-related QT prolongation is unlikely to completely explain the findings of the present study. Furthermore, although we derived an optimal cutpoint of ≥504 ms based on this population, use of this cutpoint requires validation in prospective studies.
Risk stratification for sudden cardiac death using QTD is a Class III recommendation of the Task Force on Sudden Cardiac Death of the European Society of Cardiology, although its use has never been adequately evaluated in toxicology studies or in drug overdose literature [39]. In patients with cardiac disease, QTD predicts myocardial injury and cardiac death, as well as adverse cardiac events in patients with Long QT Syndrome [25, 40, 41]. We found that QTD was significantly associated with ACVE using univariate analysis, but it lost significance in the multivariable model. This may have been due to several factors such as covariance with QTc interval and/or effects of the heart rate as a confounder. Furthermore, ROC analysis of this data demonstrated that QTD performed no better than QTc as far as area under the curve (Figs. 3 and 4) and diagnostic test characteristics (Table 5). Therefore, at this point, we cannot recommend routine calculation of the QTD for patients with suspected poisoning based on this study alone. Further studies evaluating QTD for suspected and confirmed poisoning are necessary to further investigate its potential utility.
Limitations
There are several limitations that must be considered with the analysis of this dataset, including all the inherent limitations of the case-control study design. As this is the first controlled study to evaluate the role of the ECG in undifferentiated poisoning, we did not stratify patients according to mechanism of drug overdose; however, as the probability of ACVE may vary across drug class, this should be the subject of future study. Identification of cases may have been subject to selection bias based on the availability of telephone follow-up, the availability of faxed ECGs, and possible underreporting of referrals to the Poison Control Center [42]. Differences in the protocol for selection of cases and controls were used to generate sufficient numbers of cases with a relatively unbiased source of control subjects and may itself have biased the results; however, there were few significant differences in the baseline clinical characteristics between cases and controls so we believe this is unlikely to significantly impact on the results of the current analysis. Unfortunately, a larger sample was not available for this analysis to allow for perfect matching, but given the constraints of this dataset, we settled on having the match be simply suspected acute poisoning. Future studies are warranted to confirm and further explore the myriad hypotheses generated by this dataset and should aim for more complete matching of controls. Telephone follow-up is subject to reporting bias; however, this is more of a problem for misclassification of cases as controls, which in this study was unlikely to happen due to the sampling of controls from three Poison Center-affiliate base hospitals with bedside consultation and medical record availability. Routine, clinically indicated toxicology screens (both serum and urine) were used rather than specific, send-out confirmatory tests for each suspected exposure; while the presence of a positive routine toxicology screen is unlikely to affect clinical management, for research purposes, it adds credibility to the notion that the patient has suspected acute poisoning, especially in cases where the results are consistent with the clinical suspicion.
Limitations of ECG interpretation should also be considered in the analysis of this data. Interpretation of manually measured QT dispersion is subject to inter-observer variation [26]. Despite this, there was excellent inter-observer agreement in a randomly selected set of ECGs with a second observer. A further limitation included lack of availability of previous ECGs for baseline interpretation which would have allowed interpretation of changes in QT interval from baseline.
Conclusions
ECG factors that correlate with increased risk of ACVE during SAP include QTc prolongation, QT dispersion, ventricular ectopy, non-sinus rhythm, and evidence of ischemia. Further prospective study of these criteria is necessary to validate a strategy for prediction of adverse outcomes in poisoned patients.
References
Bronstein AC, Spyker DA, Cantilena LR Jr, Green JL, Rumack BH, Heard SE (2008) 2007 Annual report of the American Association of Poison Centers’ National Poison Data System (NPDS): 25th annual report. Clin Toxicol (Phila) 46:927–1057
McCaig LF, Burt CW (1999) Poisoning-related visits to emergency departments in the United States, 1993-1996. J Toxicol Clin Toxicol 37:817–826
Paulozzi L, Crosby A, Ryan G (2007) Increases in age-group-specific injury mortality–United States, 1999–2004. MMWR 56:1281–1284
ESC Committee, Subcommittees, and Task Forces of the American Heart Association (2005) American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 112(24 Suppl):1–203
American Academy of Clinical Toxicology (1993) Facility assessment guidelines for regional toxicology treatment centers. J Toxicol Clin Toxicol 31:211–217
American College of Emergency Physicians (1996) Poison information and treatment systems. Ann Emerg Med 28:384
Thygesen K, Alpert JS, White HD (2007) Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol 50:2173–2195
Henry CR, Satran D, Lindgren B, Adkinson C, Nicholson CI, Henry TD (2006) Myocardial injury and long-term mortality following moderate to severe carbon monoxide poisoning. JAMA 295:398–402
Satran D, Henry CR, Adkinson C, Nicholson CI, Bracha Y, Henry TD (2005) Cardiovascular manifestations of moderate to severe carbon monoxide poisoning. J Am Coll Cardiol 45:1513–1516
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction), American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Academic Emergency Medicine (2007) ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST elevation myocardial infarction. Circulation 116:e148–e304
Manini AF, Kabrhel C, Thomsen TW (2005) Acute myocardial infarction following over-the-counter use of pseudoephedrine. Ann Emerg Med 45:213–216
Schoffstall JM, Spivey WH, Gambone LM, Shaw RP, Sit SP (1991) Effects of calcium channel blocker overdose-induced toxicity in the conscious dog. Ann Emerg Med 20:1104–1108
Boehnert MT, Lovejoy FH Jr (1985) Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med 313:474–479
Huikuri HV, Castellanos A, Myerburg RJ (2001) Sudden death due to cardiac arrhythmias. N Engl J Med 345:1473–1482
Roden D, Woosley R, Primm R (1986) Incidence and clinical features of the quinidine-associated long QT syndrome: implications for patient care. Am Heart J 111:1088–1093
The Cardiac Arrhythmia Suppression Trial (CAST) Investigators (1989) Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med 321:406–412
Manini AF, Raspberry D, Hoffman RS, Nelson LS (2007) QT prolongation and torsades de pointes following overdose of ziprasidone and amantadine. J Med Toxicol 3:178–181
Yamaura K, Kao B, Iimori E, Urakami H, Takahashi S (1997) Recurrent ventricular tachyarrhythmias associated with QT prolongation following hydrofluoric acid burns. J Toxicol Clin Toxicol 35:311–313
Manini AF, Nelson LS, Hoffman RS (2007) Characteristics of poison-related fatality and timing of cardiac arrest. Clin Toxicol (Phila) 45:388, abstract
Fingerhut LA, Cox CS (1998) Poisoning mortality, 1985-1995. Public Health Rep 113:218–233
Centers for Disease Control and Prevention (2004) Unintentional and undetermined poisoning deaths – 11 states 1990-2001. MMWR 53:233–238
Liebelt EL, Francis PD, Wolf AD (1995) ECG lead aVR versus QRS interval in predicting seizures and arrhythmias in acute tricyclic antidepressant toxicity. Ann Emerg Med 26:195–201
Committee for Proprietary Medicinal Products (1997) The assessment of the potential for QT interval prolongation by non-cardiovascular medicinal products. Committee for Proprietary Medicinal Products, London
Kenigsberg DN, Khanal S, Kowalski M, Krishnan SC (2007) Prolongation of the QTc interval is seen uniformly during early transmural ischemia. J Am Coll Cardiol 49:1299–1305
Calder K, Tomongin C, Mallon WK, Genna T, Bretsky P, Henderson SO (2002) Manual measurement of QT dispersion in patients with acute myocardial infarction and nondiagnostic electrocardiograms. Acad Emerg Med 9:851–854
Malik M, Batchvarov VN (2000) Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol 36:1749–1766
Viskin S (1999) Long QT syndromes and torsades de pointes. Lancet 354:1625–1633
Sawanobori T, Adaniya H, Hirano Y, Hiraoka M (1996) Effects of antiarrhythmic agents and Mg2+ on aconitine-induced arrhythmias. Jpn Heart J 37:709–718
Teschemacher AG, Seward EP, Hancox JC, Witchel HJ (1999) Inhibition of the current of heterologously expressed HERG potassium channels by imipramine and amitriptyline. Br J Pharmacol 128:479–485
Volders PG, Sipido KR, Vos MA, Spätjens RL, Leunissen JD, Carmeliet E et al (1999) Downregulation of delayed rectifier K (+) currents in dogs with chronic complete atrioventricular block and acquired torsades de pointes. Circulation 100:2455–2461
Yan GX, Wu Y, Liu T, Wang J, Marinchak RA, Kowey PR (2001) Phase 2 early afterdepolarizations as a trigger of polymorphic ventricular tachycardia in acquired long-QT syndrome: direct evidence from intracellular recordings in the intact left ventricular wall. Circulation 103:2851–2856
Nelson LS (2002) Toxicologic myocardial sensitization. J Toxicol Clin Toxicol 40:867–880
Day CP, McComb JM, Campbell RW (1992) QT dispersion: an indication of arrhythmia risk in patients with long QT intervals. Br Heart J 67:39–41
Surawicz B (1989) Electrophysiologic substrate of torsades de pointes: dispersion of repolarization or early afterdepolarizations. J Am Coll Cardiol 14:172–184
Niemann JT, Bessen HA, Rothstein RJ, Laks MM (1986) Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol 57:1154–1159
Institute of Medicine, Board on Health Care Services (2006) Hospital-based emergency care: at the breaking point. National Academies Press, Washington, DC
Straus SMJM, Kors JA, De Bruin ML, van der Hooft CS, Hofman A, Heeringa J et al (2006) Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol 47:362–367
Mangoni A, Kinirons M, Swift C, Jackson S (2003) Impact of age on QT interval and QT dispersion in healthy subjects. Age Ageing 32:326–331
Priori SG, Aliot E, Blømstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P et al (2001) Task force on sudden cardiac death of the European Society of Cardiology. Eur Heart J 22:1374–1450
Darbar D, Luck J, Davidson N, Pringle T, Main G, McNeill G et al (1996) Sensitivity and specificity of QTc dispersion for identification of risk of cardiac death in patients with peripheral vascular disease. BMJ 312:874–878
Sauer AJ, Moss AJ, McNitt S, Peterson DR, Zareba W, Robinson JL et al (2007) Long QT syndrome in adults. J Am Coll Cardiol 49:329–337
Linakis JG, Frederick KA (1993) Poisoning deaths not reported to the regional Poison Control Center. Ann Emerg Med 22:1822–1828
Acknowledgements
None
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant Support: Supported in part by a grant from a career development award (K23DA026476) from the National Institute on Drug Abuse (PI: AFM) and a grant from the Speakers Fund for Biomedical Research: Towards the Science of Patient Care awarded by the City of New York (PI: AFM).
Rights and permissions
About this article
Cite this article
Manini, A.F., Nelson, L.S., Skolnick, A.H. et al. Electrocardiographic Predictors of Adverse Cardiovascular Events in Suspected Poisoning. J. Med. Toxicol. 6, 106–115 (2010). https://doi.org/10.1007/s13181-010-0074-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-010-0074-x