Abstract
Aniridia is a rare, bilateral, congenital ocular disorder causing incomplete formation of the iris, usually characterized by iris aplasia/hypoplasia. It can also appear with other ocular anomalies, such as cataracts, glaucoma, corneal pannus, optic nerve hypoplasia, macular hypoplasia, or ectopia lentis. In the majority of cases, it is caused by mutation in the PAX6 gene, but it can also be caused by microdeletions that involve the 11p13 region. Twelve unrelated patients of Polish origin with a clinical diagnosis of aniridia were screened for the presence of microdeletions in the 11p13 region by means of multiplex ligation probe amplification (MLPA). Additionally, the coding regions of the PAX6 gene were sequenced in all probands. MLPA examination revealed different size deletions of the 11p13 region in five patients. In three cases, deletions encompassed the entire PAX6 gene and a few adjacent genes. In one case, a fragment of the PAX6 gene was deleted only. In the final case, the deletion did not include any PAX6 sequence. Our molecular findings provide further evidence of the existence of the distant 3′ regulatory elements in the downstream region of the PAX6 gene, which is known from other studies to influence the level of protein expression. Sequence analysis of the PAX6 gene revealed the three different point mutations in the remaining four patients with aniridia. All the detected mutations were reported earlier. Based on accomplished results, the great diversity of the molecular basis of aniridia was found. It varies from point mutations to different size deletions in the 11p13 region which encompass partly or completely the PAX6 gene or cause a position effect.
Similar content being viewed by others
Introduction
Aniridia (MIM:106210) is a rare, bilateral, congenital ocular disorder causing incomplete formation of the iris. The visual impairment caused by iris aplasia/hypoplasia might be enhanced by several ocular anomalies, such as cataracts, glaucoma, corneal pannus, macular hypoplasia, nystagmus, and photophobia. The prevalence of aniridia in the general population is approximately 1 in 64,000 to 1 in 96,000 live births. Two-thirds of cases are familial, with autosomal dominant mode of inheritance, complete penetrance, and variable expressivity. One-third of cases are sporadic and result from de novo mutations (Kokotas and Petersen 2010).
Mutations in the PAX6 gene
PAX6 (MIM:607108; NM_001604.4) was identified as a candidate gene for aniridia by positional cloning in 1991 (Ton et al. 1991). Mutations in the PAX6 gene are the major cause of congenital aniridia. PAX6 is a member of the paired box gene family, located on chromosome 11p13, and consists of 14 exons that span over 22 kb in length. It encodes a 422-amino acid transcriptional factor, involved in oculogenesis and other developmental processes. The protein contains three functional domains: paired domain (PD) and homeodomain (HD), separated by the proline/serine/threonine-rich transactivation domain (PST). The paired domain comprises two structurally distinct DNA-binding subdomains: the N-terminal subdomain (NTS) and the C-terminal subdomain (CTS) (Kokotas and Petersen 2010). The protein is abundantly expressed in the forebrain, early eye structures, ventral spinal cord, and endocrine pancreas (Lauderdale et al. 2000). Pathogenic alterations in the PAX6 gene reported to date include: nonsense, splicing, frame-shifting insertions or deletions, in-frame insertions or deletions, missense, and run-on mutations (D’Elia et al. 2007). Human PAX6 mutations are archived in the PAX6 Allelic Variant Database (LOVD: Leiden Open Variation Database, http://lsdb.hgu.mrc.ac.uk/home.php). The majority of mutations in the PAX6 gene are nonsense mutations, which are considered to produce truncated transcripts that activate the nonsense-mediated decay (NMD) process, resulting in haploinsufficiency of PAX6 (Fantes et al. 1995).
11p13 deletions
Aniridia can be also caused by chromosomal rearrangements that involve the 11p13 region. A significant proportion of chromosomal rearrangements are submicroscopic microdeletions (Crolla and van Heyningen 2002). There have been described cases of aniridia with deletions not involving the structure of the gene but with the removal of 3’ regulatory elements essential for adequate PAX6 expression and known as a “position effect” (Fantes et al. 1995).
Chromosomal alterations in the chromosome 11p, encompassing the PAX6 and WT1 (*607102) genes, may cause WAGR syndrome (MIM:194072). WAGR syndrome is a rare contiguous gene deletion syndrome, clinically associated with Wilms’ tumor, aniridia, genitourinary anomalies, and mental retardation (Fischbach et al. 2005). Wilms’ tumor is one of the most common solid tumors of childhood, which affects approximately 1 in 10,000 children. In patients with WAGR syndrome, the risk that Wilms’ tumor will develop reaches 45 % (Crolla and van Heyningen 2002).
The aim of this study was to analyze the genetic background of disease in Polish patients with aniridia.
Materials and methods
Patients
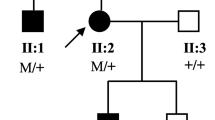
This study comprises 12 unrelated patients of Polish origin, with a clinical diagnosis of aniridia, based on ophthalmologic examination and family history. Among them, there are five patients with positive family history, six sporadic cases, and one patient (p6) who was adopted, for whom we have no information about the patient’s biological parents. The ophthalmologic findings of the patients are summarized and compared in Table 1. The local ethics committee approved the study and a written informed consent was obtained from all subjects or their legal guardians.
Methods
Genomic DNA was extracted from venous blood samples using a standard salting-out procedure. Patients were screened for structural rearrangements in the 11p13 region, using multiplex ligation probe amplification (MLPA) analysis. MLPA allowed in the first instance to exclude WT1 gene deletion, associated with a high risk of Wilms’ tumor. MLPA reaction was performed using the P219-B1 commercial kit (MRC-Holland, Amsterdam, Netherlands), following the manufacturer’s instructions and using an exactly defined amount of genomic DNA (200 ng). The kit contains probes for the PAX6 gene (with the exception of exon 6) and for the following genes located upstream, WT1, HIPK3, LMO2, EHF, CD44, and RCN1, and downstream, BDNF, FSHB, DCDC1, and ELP4, of PAX6. Data were intra-normalized by dividing the area of the peak for each amplification product by the total area of the reference probes’ products in the probemix. Inter-sample normalization was achieved by dividing the intra-normalized probe ratio of all reference samples. Data normalization was performed within one experiment (MRC-Holland). Peak areas in the range 0.65–1.31 were considered normal, below 0.65 as a deletion, and above 1.31 as a duplication. Each MLPA analysis included several control samples (DNA from healthy individuals).
The coding regions of the PAX6 gene were sequenced (exon 5a included) to exclude point mutations. PCR products were separated on an ABI 3130xl Capillary Sequencer (Applied Biosystems). Additionally, in patients p2, p3, and p6, the PAX6 gene promoter was sequenced. The sequenced fragment included 5′UTR and 1,500 nucleotides upstream of the 5′UTR fragment of the PAX6 gene. The sequences of the primers used in the amplification and sequencing of the PAX6 gene and PAX6 promoter are given in Table 2. Subsequently, to uncover probable, smaller, rare copy number variations (CNVs), array comparative genomic hybridization analysis (using NimbleGen Human CGH 6x630K, Roche) of these three patients was performed. The DNA labeling reaction and hybridization were carried out according to the manufacturer’s instructions.
Results
MLPA examination revealed different size heterozygous deletions of the 11p13 region in five patients. In three cases, deletions encompassed the PAX6 gene and a few adjacent genes. The heterozygous deletion in patient p8 contains five annotated genes: PAX6, doublecortin domain-containing protein 1 (DCDC1, MIM:608062), elongation factor protein 4 (ELP4, MIM:606985), brain-derived neurotrophic factor (BDNF, MIM:113505), and beta polypeptide of follicle-stimulating hormone (FSHB, MIM:136530) (Fig. 1a). The heterozygous deletion in patient p9 harbors the following six genes: PAX6, DCDC1, ELP4, FSHB, reticulocalbin 1 (RCN1, MIM:602735), and DKFZp686K1684. In patient p11, a large heterozygous deletion of the 11p13 region (WT1 gene included) was found (Fig. 1b), which confirmed the diagnosis of WAGR syndrome. In one patient (p12), a heterozygous deletion of several contiguous exons (exons 1–8) of the PAX6 gene was found (Fig.1c). In patient p10, MLPA revealed a heterozygous deletion of approximately 0.6 Mb on chromosome 11. The deletion did not include the PAX6 sequence. The following four genes located downstream of PAX6 are present in the deleted region: DCDC1, zinc finger CLS domain containing protein 3 (DPH4, MIM:611072), IMP1 inner mitochondrial membrane peptidase (IMMP1L, MIM:612323), and ELP4 (published data, Wawrocka et al. 2012).
The analysis of the coding region of the PAX6 gene by direct sequencing revealed three different point mutations in the remaining four patients. All the detected mutations were previously reported. In patient p1, we identified a c.718C > T heterozygous nonsense mutation, which occurred in the protein homeodomain (HD), resulting in a change of arginine to stop codon (p.Arg240*). In patients p4 and p7, another heterozygous nonsense mutation at position c.949C > T was identified. It is present in the PST domain coding region, and results in a premature termination of the PAX6 protein (p.Arg317*). According to the database, the identified mutations are common deleterious mutations in the PAX6 gene and they probably encode a non-functional protein. Bidirectional sequencing of exon/intron boundaries for patient p5 resulted in the identification of a nucleotide substitution at the splice donor sequence of intron 6, c.357 + 1G > A (IVS6 + 1G > A) (Fig. 2).
Sequencing of the PAX6 gene promoter in patients p2, p3, and p6 did not identify any mutation in this region. So, the molecular methods used in this study did not allow to detect any mutations in patients p2, p3, and p6. Therefore, array comparative genomic hybridization analysis of these three patients was performed. However, array comparative genomic hybridization (aCGH) analysis also did not reveal any causative mutation. The patients’ molecular findings are summarized in Table 3.
Discussion
This is the first molecular study carried out on Polish patients with aniridia. In this study, we identified the alterations that cause the disease in 9 of 12 examined (75 %) patients with aniridia. The major finding of the present study is the great diversity of the molecular basis of aniridia in Polish patients. It is also worth mentioning that, in our group of patients, aniridia is more frequently caused by large deletions than by the PAX6 gene point mutations. This statement is in contrast to larger studies done by Ton et al. (1991), Kokotas and Petersen (2010), and Park et al. (2012). Those researchers stated that heterozygous mutations in the PAX6 gene are found in about 40–80 % of all non-syndromic aniridia patients. However, we must remember that our results are based on a small group, thus, our conclusion requires further verification with a larger cohort of aniridia patients.
The large deletion containing not only PAX6 but also several other genes and the RCN1 gene was detected by MLPA analysis in patient p9 (Table 3). The RCN1 gene is a Ca2+ binding protein, participating in the secretory pathway. Favor et al. (2009) reported that mouse, containing a heterozygous deletion of the AX6 and RCN1 genes, presents an extreme microphthalmia. They suggest that RCN1 may have an influence on the eye phenotype in PAX6 contiguous gene deletions. A familial case of aniridia resulting from a deletion containing PAX6, RCN1, and DKFZp686k1684 was reported by Zhang et al. (2011). Severe visual impairment observed in the described family is compatible with the mouse phenotype reported by Favor et al. (2009). Patient p9 contains a very similar deletion of the downstream flanking region of PAX6 to the family described by Zhang et al. (2011). However, our patient exhibits no significant phenotype differences in comparison to other aniridia patients presented in this study. Microphthalmia was not observed.
When the deletion does not include the PAX6 sequence, then the so-called “position effect” is the underlying pathogenic mechanism of aniridia in these patients. Such a case is observed in patient p10, who has been diagnosed to have aniridia, despite the fact that the structure of the PAX6 gene was normal. Submicroscopic deletions not involving the PAX6 gene in the patients with aniridia were previously described by several authors (Lauderdale et al. 2000; D’Elia et al. 2007; Davis et al. 2008; Wawrocka et al. 2012). MLPA analysis revealed in this patient a heterozygous deletion encompassing several genes, including the ELP4 gene. Kleinjan et al. (2006) confirmed that cis-regulatory elements located within the introns of the ELP4 gene are PAX6-specific long-range control elements, essential for normal expression of the gene. Functional studies in human cells and animal models confirmed the presence of 3′ regulatory elements in the downstream region of PAX6, which are essential for normal expression of the gene. Our molecular findings provide further evidence of the existence of the distant 3′ regulatory elements in the downstream region of the PAX6 gene, which are known from other studies to influence the level of protein expression.
DNA sequencing of the PAX6 gene revealed three different mutations: two nonsense mutations, c.718C > T and c.949C > T (in two patients), and one splice-site mutation, c.357 + 1G > A. It was previously described that the mutation c.357 + 1G > A lead to the use of a cryptic splice donor site within exon 6, leading to an in-frame deletion of 36 amino acids from the PD (Hingorani et al. 2009). The heterozygous mutation c.718C > T (p.Arg240*) in patient p1 occurred in the protein HD. In two unrelated patients (p4 and p7), identical heterozygous substitution c.949C > T (p.Arg317*) in the PST domain coding region was discovered. In accordance to the PAX6 mutation database: c.718C > T and c.949 C > T are the most frequent PAX6 mutations causing aniridia. Despite the presence of the same mutation, both patients represent quite divergent phenotypes. Singh et al. (1998) showed that the variable phenotype could be explained by differences in PAX6 protein levels, the ratio of mutant and normal protein, and interaction with different molecular factors. It was reported that mutations behind the HD could lead to more severe phenotypes in comparison with truncating mutations in the PD or HD domains (Kokotas and Petersen 2010; Park et al. 2012). This partly agrees with our observations that patient p4 (mutation in the PST domain) showed a more severe phenotype of aniridia in comparison to patient p1 (mutation in the HD) (Table 1).
We have not determined any genetic causes of aniridia in three patients (p2, p3, and p6). The disease can be caused by abnormalities in the PAX6 gene promoter or in the regulatory elements that affect the normal expression of the gene but are not routinely subjected to sequencing. Therefore, we decided to sequence the PAX6 gene promoter in these patients. However, the sequencing did not reveal any mutation in the PAX6 promoter. Another possible explanation for this fact is that chromosomal rearrangements that involved a gene or genes in the 11p13 region do not include the probes used in the MLPA analyses. Patient p2 suffers from aniridia and microphthalmia. The presence of microphthalmia with aniridia suggests the possibility of genocopy. Therefore, another gene involved in oculogenesis can be responsible for the disease. Possibly, the damage of the iris only resembles aniridia. aCGH analysis of patient p2 was performed, as well as in two other patients, in whom the genetic background of aniridia was not determined (p3, p6). This analysis allows to uncover smaller, rare CNVs that cannot be detected by lower resolution molecular techniques. However, no causative mutation was found.
Ophthalmic findings revealed nearly no phenotypic variabilities of the aniridia. Patients having deletion 3′ to the PAX6 gene exhibit no significant phenotypic differences compared to the patients with point mutations in the PAX6 gene. Due to quite the homogenous clinical symptoms and a small number of patients, we were not able to define any genotype–phenotype correlations. The findings of the current study are consistent with those of D’Elia et al. (2007), Lim et al. (2012), and Park et al. (2012), who did not find any phenotypic differences according to the identified genotype. Defining the genotype–phenotype correlation requires the analysis of a larger cohort of patients.
In connection to the great variability of mutations in aniridia patients, it is recommended to perform several analyses to detect the genetic background of aniridia. First of all, we care about the exclusion of life-threatening Wilms’ tumor (associated with the WT1 gene deletion) and then the detection of genetic causes of aniridia. Therefore, we decided to perform MLPA analysis first (to detect structural rearrangements in the PAX6 gene and 11p13 region) and then PAX6 gene sequencing (to identify point mutations). Additionally, gene sequencing is not usually used to detect copy number changes; therefore, in our opinion, it is better to begin the molecular analysis with MLPA or aCGH.
References
Crolla JA, van Heyningen V (2002) Frequent chromosome aberrations revealed by molecular cytogenetic studies in patients with aniridia. Am J Hum Genet 71:1138–1149
Davis LK, Meyer KJ, Rudd DS, Librant AL, Epping EA, Sheffield VC, Wassink TH (2008) Pax6 3′ deletion results in aniridia, autism and mental retardation. Hum Genet 123:371–378
D’Elia AV, Pellizzari L, Fabbro D, Pianta A, Divizia MT, Rinaldi R, Grammatico B, Grammatico P, Arduino C, Damante G (2007) A deletion 3′ to the PAX6 gene in familial aniridia cases. Mol Vis 13:1245–1250
Fantes J, Redeker B, Breen M, Boyle S, Brown J, Fletcher J, Jones S, Bickmore W, Fukushima Y, Mannens M, Danes S, van Heyningen V, Hanson I (1995) Aniridia-associated cytogenetic rearrangements suggest that a position effect may cause the mutant phenotype. Hum Mol Genet 4(3):415–422
Favor J, Bradley A, Conte N, Janik D, Pretsch W, Reitmeir P, Rosemann M, Schmahl W, Wienberg J, Zaus I (2009) Analysis of Pax6 contiguous gene deletions in the mouse, Mus musculus, identifies regions distinct from Pax6 responsible for extreme small-eye and belly-spotting phenotypes. Genetics 182(4):1077–1088
Fischbach BV, Trout KL, Lewis J, Luis CA, Sika M (2005) WAGR syndrome: a clinical review of 54 cases. Pediatrics 116(4):984–988
Hingorani M, Williamson KA, Moore AT, van Heyningen V (2009) Detailed ophthalmologic evaluation of 43 Individuals with PAX6 mutations. Invest Ophthalmol Vis Sci 50(6):2581–2590
Kleinjan DA, Seawright A, Mella S, Carr CB, Tyas DA, Simpson TI, Mason JO, Price DJ, van Heyningen V (2006) Long-range downstream enhancers are essential for Pax6 expression. Dev Biol 299(2):563–581
Kokotas H, Petersen MB (2010) Clinical and molecular aspects of aniridia. Clin Genet 77:409–420
Lauderdale JD, Wilensky JS, Oliver ER, Walton DS, Glaser T (2000) 3′ deletions cause aniridia by preventing PAX6 gene expression. Proc Natl Acad Sci USA 97(25):13755–13759
Lim HT, Seo EJ, Kim GH, Ahn H, Lee HJ, Shin KH, Lee JK, Yoo HW (2012) Comparison between aniridia with and without PAX6 mutations: clinical and molecular analysis in 14 Korean patients with aniridia. Ophthalmology 119(6):1258–1264
Park SH, Kim MS, Chae H, Kim Y, Kim M (2012) Molecular analysis of the PAX6 gene for congenital aniridia in the Korean population: identification of four novel mutations. Mol Vis 18:488–494
Singh S, Tang HK, Lee JY, Saunders GF (1998) Truncation mutations in the transacitivation region of PAX6 result in dominant-negative mutants. J Biol Chem 273:21531–21541
Ton CC, Hirvonen H, Miwa H, Weil MM, Monaghan P, Jordan T, van Heyningen V, Hastie ND, Meijers-Heijboer H, Drechsler M, Royer-Pokora B, Collins F, Swaroop A, Strong LC, Saunders GF (1991) Positional cloning and characterization of a paired box- and homeobox-containing gene from the aniridia region. Cell 67(6):1059–1074
Wawrocka A, Budny B, Debicki S, Jamsheer A, Sowinska A, Krawczynski MR (2012) PAX6 3′ deletion in a family with aniridia. Ophthalmic Genet 33(1):44–48
Zhang X, Zhang Q, Tong Y, Dai H, Zhao X, Bai F, Xu L, Li Y (2011) Large novel deletions detected in Chinese families with aniridia: correlation between genotype and phenotype. Mol Vis 17:548–577
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Wawrocka, A., Sikora, A., Kuszel, L. et al. 11p13 deletions can be more frequent than the PAX6 gene point mutations in Polish patients with aniridia. J Appl Genetics 54, 345–351 (2013). https://doi.org/10.1007/s13353-013-0154-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13353-013-0154-0