Abstract
Introduction
The central diagnostic feature of rosacea is diffuse central-facial erythema. The objective was to summarize published and unpublished health-related quality of life (HRQoL) data from seven previous studies in rosacea patients.
Methods
A meta-analysis was performed on baseline HRQoL data of subjects with erythema of rosacea from five randomized controlled trials, one open-label safety study and one epidemiological study. The data from four questionnaires were analyzed, including the Euro QoL 5-dimension (EQ5D) generic questionnaire, the Dermatology Life Quality Index (DLQI) dermatology-specific quality of life instrument, the Productivity and Social Life Questionnaire and the Facial Redness Questionnaire.
Results
The global EQ5D index score was 0.859 and the domains of pain/discomfort (31.5% moderate or extreme pain) and anxiety/depression (26.4% moderate or extreme) were most affected. Worse scores were observed with erythema of rosacea in the absence of inflammatory lesions (EQ5D score of 0.832 for no lesions vs 0.919 for subjects with ≥1 lesion). Almost half (43%) the subjects had at least moderately impaired HRQoL, including 19.8% with a DLQI total score of ≥11 indicating severely impaired HRQoL; symptoms/feelings was the most affected domain. Subjects with a patient self-assessment (PSA) of severe erythema of rosacea had a worse mean DLQI score than moderate PSA subjects (8.6 vs 6.0). Work life and social life were affected, especially in subjects with severe PSA (62% with social life at least somewhat affected).
Conclusion
Erythema of rosacea causes a marked decrease in HRQoL in most patients, especially those with self-perceived severe erythema and without inflammatory lesions, and should thus be considered as an important medical problem requiring medical intervention.
Funding
Galderma UK.
Similar content being viewed by others
Introduction
Rosacea is a common chronic inflammatory skin disease causing flushing, redness, red pimples and pustules on the face [1]. Furthermore, symptoms of rosacea may lead to physical discomfort (e.g., burning and stinging) and may have considerable psychosocial impact causing embarrassment, anxiety and low self-esteem among patients [2]. As erythema or facial redness is clearly visible, it is one of the main factors contributing to low health-related quality of life (HRQoL) in rosacea patients [3].
It has been reported that some clinicians consider erythema of rosacea as mainly a cosmetic problem and underestimate the HRQoL burden [4, 5]. Providing physicians and decision-makers with HRQoL data on the facial redness of rosacea is therefore important in the management of the disease, especially since effective treatments for erythema of rosacea currently exist.
The most recent Cochrane review on interventions for rosacea listed change in HRQoL as their first priority primary outcome, highlighting the relevance of measuring HRQoL in research and clinical practice [6]. In fact, of the 106 articles in that Cochrane review, only 11 studies reported assessments of change in quality of life following treatment for rosacea [6]. HRQoL data has not always been collected in a structured manner and a systematic review found it was difficult to summarize HRQoL data from rosacea studies due to the wide heterogeneity of the studies [7]. A small pilot study investigating the burden of the disease among the various different types of rosacea found that all subtypes had a relatively similar negative impact on HRQoL [8]. However, only two studies (38 patients in total) have been identified reporting HRQoL data specifically in patients with erythematotelangiectatic rosacea [9, 10].
The aim of this meta-analysis was to analyze the effect of facial erythema of rosacea on HRQoL by pooling data from four questionnaires (two validated generic and dermatology-specific and two non-validated rosacea and redness-specific questionnaires) used in seven recent studies.
Methods
Study Selection
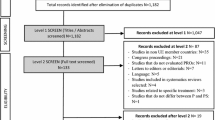
A meta-analysis was performed on published and unpublished baseline (before any treatment) HRQoL data from previous Galderma-sponsored studies. The incorporation criteria were all studies that generated HRQoL data using at least one of the following questionnaires, including the Euro QoL 5-dimension 3-level (EQ5D-3L), Dermatology Life Quality Index (DLQI), the Productivity and Social Life Questionnaire (PSLQ) or Facial Redness Questionnaire (FRQ). Data were available for a total of 1624 subjects with erythema of rosacea from five randomized controlled trials [11–13], one open-label safety study [14] and one epidemiological study [15].
HRQoL Instruments
Questionnaires used were the validated EQ5D generic instrument applicable to a wide range of health conditions: the validated ten-question dermatology-specific DLQI instrument [16]; the rosacea-specific PSLQ designed to assess the effect on work and social life; and the redness-specific FRQ [11]. The EQ-5D-3L provided a simple descriptive profile of five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) with three levels (no problems, some problems, extreme problems). The respondent’s self-rated health state was recorded on a vertical, visual analog scale (VAS) (100 = best imaginable health state).
Statistical Methods
The EQ-5D results for each of the three levels in each of the five dimensions were converted into a single summary index (where 0 = dead and 1.0 = full health) by applying the UK preference weights. The DLQI questions had four possible responses from not at all (0) to very much (3). The DLQI total score was calculated by summing the score of each question, resulting in a maximum of 30 and a minimum of 0, where a higher score represents worse quality of life. In addition to the DLQI total score, six domains were calculated and expressed as a percentage of the maximum score: symptoms and feelings, daily activities, leisure, work and school, personal relationships and treatment. To evaluate the impact due to erythema alone, results were calculated for the subgroups of subjects with and without lesions. To evaluate the impact of self-perceived severe erythema of rosacea, the DLQI total score was calculated for subjects with moderate and severe patient self-assessed (PSA) erythema. Analysis was performed using SAS statistical software, version 9.3 (SAS Institute Inc., Cary, NC, USA).
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Results
Subject Disposition
Demographic data for subjects responding to the questionnaires are summarized in Table 1. Pooled baseline DLQI data was reported for 622 subjects with a mean age of 44.3 years: 74.3% were women, 38.5% had ≥1 inflammatory lesion and around three-quarters (74.8%) had clinician-assessed moderate erythema (CEA) (Table 1). A total of 92 subjects completed the EQ5D and FRQ questionnaires with a mean age of 54.1 years; 30.4% had inflammatory lesions (a maximum of 5 inflammatory lesions were allowed) and all subjects assessed their erythema (PSA) as being severe (Table 1). The PSLQ questionnaire was completed by 1002 subjects, the majority of whom had moderate erythema based on either CEA (83.9%) or PSA (84.9%) (Table 1).
EQ5D Questionnaire
Overall, the mean of the VAS was 74.0 out of 100 and the overall EQ5D single index score was 0.859 (Table 2).
The most affected domains were pain/discomfort (31.5% of subjects reported having moderate or extreme pain) and anxiety/depression (26.4% of subjects reported being moderately or extremely anxious or depressed).
A worse mean health state was observed for subjects without inflammatory lesions (72.3) than in subjects with ≥1 lesion (78.0) and this was the case across all domains (Table 2). Similarly, the global EQ5D score was 0.832 for subjects with no lesions (n = 64) and 0.919 for subjects with at least one lesion (n = 28 subjects) (Table 2).
DLQI Questionnaire
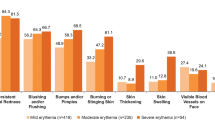
The mean DLQI total score for the pooled data of 622 subjects was 6.2 points, indicating a moderate influence of erythema of rosacea on HRQoL. Almost half the subjects (43%) had at least a moderate effect on their HRQoL and 19.8% of subjects had a total score of ≥11, indicating severely impaired HRQoL (Fig. 1a). Symptoms and feelings were the most affected domain with a mean score of 2.3. The mean DLQI scores expressed as a percentage of the maximum score for each domain are shown in Fig. 2.
Subjects with a PSA of severe erythema of rosacea had a worse mean total DLQI score than moderate PSA subjects (8.6 vs 6.0) (see Fig. 1b for an interpretation of the scores). Also, subjects without inflammatory lesions had a worse DLQI score than subjects with ≥1 lesion (7.4 vs 6.3).
PSLQ
Of the subjects who worked, 11% indicated that their rosacea had affected their productivity at work (Table 3). Around a quarter of subjects (26.1%) responded that they had avoided public contact or canceled social engagements because of their rosacea (Table 3).
FRQ
Of the 92 subjects, 79.4% were extremely, moderately or somewhat self-conscious about their facial redness (Fig. 3). In this population of PSA severe subjects, almost two-thirds (62%) and almost half (47.8%) reported that their erythema of rosacea at least somewhat interfered with their social life and work life, respectively.
Discussion
This pooled analysis incorporating data collected from a total of 1624 subjects in seven recent studies, using four questionnaires, confirms that erythema of rosacea significantly affects patients’ HRQoL. All HRQoL instruments have conceptual limitations; hence we chose to incorporate validated generic (EQ5D is very widely used in health economic analyses) and dermatology-specific (DLQI was the first HRQoL instrument and is the most widely used) questionnaires based on the quantity of available data for comparison with other diseases. Furthermore, to obtain a better sense of what it is like to live with erythema of rosacea, we also included the rosacea-specific PSLQ and redness-specific FRQ questionnaires, albeit non-validated questionnaires.
The EQ5D highlighted pain/discomfort and anxiety/depression as the main drivers of reduced HRQoL in rosacea subjects. Overall, the mean EQ-5D scores (VAS 74.0 and index score 0.859) were similar to values reported for other severe conditions. For comparison, a systematic literature review of HRQoL in psoriasis reported mean EQ-5D VAS scores ranging from 50.7 to 75.1 and mean EQ-5D utility index scores from 0.52 to 0.9 [17]. The authors concluded that these values for patients with psoriasis corresponded to the same level of deterioration in HRQoL as for patients with other serious chronic diseases, e.g., cardiovascular disease.
The relatively low EQ-5D HRQoL score for erythema of rosacea may reflect the fact that all the EQ-5D population subjects (100%) had self-perceived severe erythema, which was confirmed for around half of them (51.1%) by a clinician’s assessment. Indeed, PSA severe subjects had a worse mean DLQI score than moderate PSA subjects (8.6 vs 6.0). Furthermore, a systematic review exploring HRQoL in patients with cutaneous rosacea identified an association between negative impact on HRQoL and disease severity [7].
Symptoms/feelings was the most impacted DLQI domain. Overall, the mean DLQI total score of 6.2 points indicates a moderate influence of erythema of rosacea on HRQoL. This value is very similar to that in existing literature since a review on 10 years of experience with the DLQI reported a mean of means of 6.7 for rosacea/rhinophyma [18]. This score is lower than the mean of means reported for psoriasis (8.8) or acne (11.9), but higher than the scores for Darier’s disease (5.9) or Hailey–Hailey disease (6.1) [18]. Two previous studies in subjects exclusively with erythematotelangiectatic rosacea reported comparable DLQI scores of 5.6 and 7.8 [9, 10].
The subjects without lesions (EQ5D VAS of 72.3; EQ5D single index score of 0.83; DLQI total score of 7.4) appeared to have even worse HRQoL than subjects with ≥1 inflammatory lesion (EQ5D VAS of 78; EQ5D single index score of 0.92; DLQI total score of 6.3); patients may thus be most concerned about the persistent redness or erythema of rosacea rather than the presence of inflammatory lesions.
Results of the non-validated disease-specific PSLQ and redness-specific FRQ confirmed the results observed with the validated questionnaires. Rosacea was shown to affect work life and social life using the PSLQ (subjects mostly with moderate redness). An even larger effect on work and social life was observed with the FRQ in subjects with PSA severe redness. Similarly, a large-scale international survey showed that erythema of rosacea can lead to stigmatization, as well as having an impact on emotional and psychological well-being [19].
Treatments for the persistent redness of rosacea, e.g., brimonidine 0.33% gel (3.3 mg/g) [11–14, 20, 21] and laser and intense-pulsed light [9, 10], have been reported to improve patients’ HRQoL [22]. However, despite the availability of effective treatments, many rosacea patients are underdiagnosed, misdiagnosed and undertreated [15]. It appears that patients do not always seek medical advice [23], may be unable to successfully convey the impact on HRQoL and/or clinicians may overlook the psychological impact. A possible explanation for this may be that physicians have limited time during a consultation for effective communication and do not encourage patients to express their views [24, 25].
The use of HRQoL instruments in clinical practice, combined with effective patient–physician communication, should help facilitate dialog between physicians and patients, so that treatment decisions can be based on the patient’s priorities and preferences informed by best medical evidence [25–28].
Recommendations have been developed to help the introduction of HRQoL tools into clinical practice and new technology may be able to address many of the practical problems associated with measuring HRQoL in clinical practice [28].
A possible limitation of this meta-analysis is that it was not from a systematic review of the literature. However, it was a pooled analysis of seven existing studies and included published and unpublished data that met our incorporation criteria (data from one of the four questionnaires) to avoid publication bias. It is noteworthy that the EQ5D and FRQ data were from a single study (n = 92 subjects), in which the maximum number of lesions allowed was limited to five [11]. Although subjects participating in clinical studies may not be representative of the general population [11–14] (except for subjects in the epidemiological study [15]), an advantage of these subjects is that they all had a confirmed diagnosis of rosacea.
Conclusion
This meta-analysis demonstrated that erythema of rosacea causes a marked decrease in HRQoL, especially in subjects with self-perceived severe erythema. Patients without inflammatory lesions may be even more concerned about the persistent redness or erythema of rosacea than those with inflammatory lesions. The results highlight the need for medical intervention to treat the symptoms of erythema of rosacea and improve patients’ well-being.
References
Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46(4):584–7.
Aksoy B, Altaykan-Hapa A, Egemen D, Karagöz F, Atakan N. The impact of rosacea on quality of life: effects of demographic and clinical characteristics and various treatment modalities. Br J Dermatol. 2010;163(4):719–25.
National rosacea Society survey available at: http://www.rosacea.org/weblog/survey-shows-facial-redness-takes-emotional-toll. Accessed Jan 28, 2016.
Lowe NJ, Behr KL, Fitzpatrick R, Goldman M, Ruiz-Esparza J. Flash lamp pumped dye laser for rosacea-associated telangiectasia and erythema. J Dermatol Surg Oncol. 1991;17(6):522–5.
Balkrishnan R, McMichael AJ, Hu JY, et al. Corrective cosmetics are effective for women with facial pigmentary disorders. Cutis. 2005;75(3):181–7.
van Zuuren EJ, Fedorowicz Z, Carter B, van der Linden MMD, Charland L. Interventions for rosacea. Cochrane Database Syst Rev. 2015;4:CD003262.
van der Linden MM, van Rappard DC, Daams JG, Sprangers MA, Spuls PI, de Korte J. Health-related quality of life in patients with cutaneous rosacea: a systematic review. Acta Derm Venereol. 2015;95(4):395–400.
Kini SP, Nicholson K, De Long LK, et al. A pilot study in discrepancies in quality of life among three cutaneous types of rosacea. J Am Acad Dermatol. 2010;62(6):1069–71.
Menezes N, Moreira A, Mota G, Baptista A. Quality of life and rosacea: pulsed dye laser impact. J Cosmet Laser Ther. 2009;11(3):139–41.
Tan SR, Tope WD. Pulsed dye laser treatment of rosacea improves erythema, symptomatology, and quality of life. J Am Acad Dermatol. 2004;51(4):592–9.
Layton AM, Schaller M, Homey B, et al. Brimonidine gel 0.33% rapidly improves patient-reported outcomes by controlling facial erythema of rosacea: a randomised double-blind vehicle-controlled study. J Eur Acad Dermatol Venereol. 2015;29:2405–10.
Fowler J, Jarratt M, Moore A, et al. Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol. 2012;166(3):633–41.
Fowler J Jr, Jackson JM, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, and vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650–6.
Moore A, Kempers S, Murakawa G, et al. Long-term safety and efficacy of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of a 1-year open-label study. J Drugs Dermatol. 2014;13:56–61.
Tan J, Schöfer H, Araviiskaia E, Audibert F, Kerrouche N, Berg M, The RISE study group. Prevalence of rosacea in the general population of Germany and Russia—the RISE study. J Eur Acad Dermatol Venereol. 2016;30:428–34.
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210–6.
Møller AH, Erntoft S, Vinding GR, Jemec GB. A systematic literature review to compare quality of life in psoriasis with other chronic diseases using EQ-5D-derived utility values. Patient Relat Outcome Meas. 2015;6:167–77.
Lewis V, Finlay AY. 10 Years experience of the Dermatology Life Quality Index (DLQI). J Investig Dermatol Symp Proc. 2004;9(2):169–80 (Review).
Dirschka T, Micali G, Papadopoulos L, Tan J, Layton A, Moore S. Perceptions on the psychological impact of facial erythema associated with Rosacea: results of International Survey. Dermatol Ther (Heidelb). 2015;5(2):117–27.
Fowler J, Tan J, Jackson JM, et al. Treatment of facial erythema in patients with rosacea with topical brimonidine tartrate: correlation of patient satisfaction with standard clinical endpoints of improvement of facial erythema. J Eur Acad Dermatol Venereol. 2015;29:474–81.
Johnson AW, Johnson SM. The role of topical brimonidine tartrate gel as a novel therapeutic option for persistent facial erythema associated with rosacea. Dermatol Ther (Heidelb). 2015;5(3):171–81.
Moustafa F, Lewallen RS, Feldman SR. The psychological impact of rosacea and the influence of current management options. J Am Acad Dermatol. 2014;71(5):973–80.
Huynh TT. Burden of disease: the psychosocial impact of rosacea on a patient’s quality of life. Am Health Drug Benefits. 2013;6(6):348–54.
Tan J. Challenges and solutions in selecting systemic antipsoriasis agents. J Cutan Med Surg. 2007;11(S1):S48–53.
Naldi L. Health-related quality of life: from health economics to bedside? Dermatology. 2007;215(4):273–6.
Chen SC. Health-related quality of life in dermatology: introduction and overview. Dermatol Clin. 2012;30(2):205–8.
Higginson IJ, Carr AJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ. 2001;322(7297):1297–300.
Salek S, Roberts A, Finlay AY. The practical reality of using a patient-reported outcome measure in a routine dermatology clinic. Dermatology. 2007;215(4):315–9.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Galderma.
The authors would like to thank Helen Simpson, PhD, of Galderma for medical writing and editorial assistance, as well all the study investigators involved in the various studies. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval for the version to be published.
Disclosures
Nabil Kerrouche is an employee of Galderma.
Vincent Rives is an employee of Galderma.
Anthony Bewley was an investigator and has served as a member on the rosacea advisory board of Galderma.
Joseph Fowler was an investigator and has served as a member on the rosacea advisory board and speaker’s bureau of Galderma.
Helmut Schöfer was an investigator and has been an advisor and speaker for Galderma.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/2884F06075A3983E.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bewley, A., Fowler, J., Schöfer, H. et al. Erythema of Rosacea Impairs Health-Related Quality of Life: Results of a Meta-analysis. Dermatol Ther (Heidelb) 6, 237–247 (2016). https://doi.org/10.1007/s13555-016-0106-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-016-0106-9