Abstract
Background
With the demographic change, the treatment of elderly patients has become a major issue for health systems worldwide.
Aims
The aim of this study was to analyze the change in the rate of surgical treatment of pelvic ring fractures in patients with an age of ≥60 years over a 22-year period depending on fracture type, age and sex.
Methods
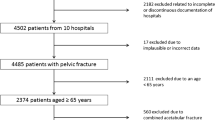
Data of 5665 patients with an age of ≥60 years, who were treated for pelvic ring fractures from 1991 to 2013 in one of 31 hospitals participating in the German Pelvic Trauma Registry, were included. The registry is divided into four time periods: t 1 = 1991–1993, t 2 = 1997–2000, t 3 = 2001–2008 and t 4 = 2009–2013. Data had been collected prospectively and was analyzed retrospectively, stratified for age and sex of the patients as well as type of fracture and mode of therapy (surgical vs. conservative).
Results
There was a significant increase (p < 0.05) in the overall rate of surgical treatment. Nonetheless, during all time periods patients with an age of >70 years were significantly less frequently surgically treated compared to 60- to 70-year-olds. Regardless of the fracture type, the rate of surgical treatment was significantly higher (p < 0.05) in male compared to female patients during t 1. While this difference persisted for type A and type B fractures, the frequency of surgical treatment of type C fractures approximated in males and females.
Conclusions
The present data indicate that the rate of surgical treatment of pelvic ring fractures in elderly patients has significantly increased over the 22-year period. Nonetheless, older patients (>70 years) as well as female patients are still less frequently surgically treated.




Similar content being viewed by others
References
National Institute on Aging, Why Population Aging Matters: A Global Perspective. National Institute on Aging (2008) US National Institutes of Health. http://www.nia.nih.gov/health/publication/why-population-aging-matters-global-perspective/trend-1-aging-population. Accessed 17 Sep 17
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37:691–697
Tosounidis G, Holstein JH, Culemann U et al (2010) Changes in epidemiology and treatment of pelvic ring fractures in Germany: an analysis on data of German Pelvic Multicenter Study Groups I and III (DGU/AO). Acta Chir Orthop Traumatol Cech 77:450–456
Culemann U, Oestern HJ, Pohlemann T (2014) Aktuelle Behandlung der Beckenringfraktur. Der Unfallchirurg 117:145–161
Baker SD, Grochow LB (1997) Pharmacology of cancer chemotherapy in the older person. Clin Geriatr Med 13:169–183
Blair SN, Kohl HW 3rd, Barlow CE et al (1995) Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 273:1093–1098
Jorm AF, Jolley D (1998) The incidence of dementia: a meta-analysis. Neurology 51:728–733
Pohlemann T, Tosounidis G, Bircher M et al (2007) The German Multicentre Pelvis Registry: a template for an European expert network? Injury 38:416–423
Isler B, Ganz R (1996) Classification of pelvic ring injuries. Injury 27:3–12
Diel P, Thier C, Aghayev E et al (2010) The international documentation and evaluation system IDES: a single center observational case series for development of an ankle prosthesis documentation questionnaire and study of its feasibility and face validity. J Foot Ankle Res 3:4
Holstein JH, Culemann U, Pohlemann T et al (2012) What are predictors of mortality in patients with pelvic fractures? Clin Orthop Relat Res 470:2090–2097
Holstein JH, Pizanis A, Kohler D et al (2013) What are predictors for patients’ quality of life after pelvic ring fractures? Clin Orthop Relat Res 471:2841–2845
Furey AJ, O’Toole RV, Nascone JW et al (2009) Classification of pelvic fractures: analysis of inter- and intraobserver variability using the Young-Burgess and Tile classification systems. Orthopedics 32:401
Barzilay Y, Liebergall M, Safran O et al (2005) Pelvic fractures in a level I trauma center: a test case for the efficacy of the evolving trauma system in Israel. Isr Med Assoc J 7:619–622
Crimmins EM, Reynolds SL, Saito Y (1999) Trends in health and ability to work among the older working-age population. J Gerontol B Psychol Sci Soc Sci 54:S31–S40
Manton KG, Gu X, Lamb VL (2006) Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the US elderly population. Proc Natl Acad Sci USA 103:18374–18379
Sophie S (2007) Anaesthesia for the elderly patient. J Pak Med Assoc 57:196–201
Klenk J, Rapp K, Buchele G et al (2007) Increasing life expectancy in Germany: quantitative contributions from changes in age- and disease-specific mortality. Eur J Public Health 17:587–592
Wahnert D, Raschke MJ, Fuchs T (2013) Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum: a new method using modified implants. Int Orthop 37:1147–1150
Bartley EJ, Fillingim RB (2013) Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 111:52–58
Mogil JS (2012) Sex differences in pain and pain inhibition: multiple explanations of a controversial phenomenon. Nat Rev Neurosci 13:859–866
Paller CJ, Campbell CM, Edwards RR et al (2009) Sex-based differences in pain perception and treatment. Pain Med 10:289–299
Popescu A, LeResche L, Truelove EL et al (2010) Gender differences in pain modulation by diffuse noxious inhibitory controls: a systematic review. Pain 150:309–318
Riley JL 3rd, Robinson ME, Wise EA et al (1998) Sex differences in the perception of noxious experimental stimuli: a meta-analysis. Pain 74:181–187
Arber S, McKinlay J, Adams A et al (2006) Patient characteristics and inequalities in doctors’ diagnostic and management strategies relating to CHD: a video-simulation experiment. Soc Sci Med 62:103–115
Borkhoff CM, Hawker GA, Wright JG (2011) Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res 469:1829–1837
Daly C, Clemens F, Lopez Sendon JL et al (2006) Gender differences in the management and clinical outcome of stable angina. Circulation 113:490–498
Katz JN, Wright EA, Guadagnoli E et al (1994) Differences between men and women undergoing major orthopedic surgery for degenerative arthritis. Arthr Rheum 37:687–694
McMurray RJ, Clarke MJAB, Dexanne BC et al (1991) Gender disparities in clinical decision making. Council on Ethical and Judicial Affairs, American Medical Association. JAMA 266:559–562
Valentin A, Jordan B, Lang T et al (2003) Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med 31:1901–1907
Hawker GA, Wright JG, Coyte PC et al (2000) Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med 342:1016–1022
Juni P, Low N, Reichenbach S et al (2010) Gender inequity in the provision of care for hip disease: population-based cross-sectional study. Osteoarthr Cartil 18:640–645
Hawker G, Wright J, Coyte P et al (1998) Health-related quality of life after knee replacement. J Bone Joint Surg Am 80:163–173
Holtzman J, Saleh K, Kane R (2002) Gender differences in functional status and pain in a Medicare population undergoing elective total hip arthroplasty. Med Care 40:461–470
Parsley BS, Bertolusso R, Harrington M et al (2010) Influence of gender on age of treatment with TKA and functional outcome. Clin Orthop Relat Res 468:1759–1764
Acknowledgments
We thank all members of the Pelvic Trauma Working Group of the German Association, who continuously invest a lot of time and effort in scientific projects and the procurement of knowledge, leading to a continuous improvement of the standards of care for patients with pelvic and acetabular fractures. Without their efforts, the German Pelvic Trauma registry and this study would not have been possible. We thank S. Drum, Center for Clinical Studies of the Department of Trauma, Hand and Reconstructive Surgery, University of Homburg for her ongoing support in data entry and processing. Institutions contributing to the German Pelvic Injury Registry Initiative: A Institutions contributing to the German Pelvic Trauma Registry include: ZNA Stuivenberg Antwerpen, Belgium; AZ Groeninge Hospital, Kortrijk, Belgium; Jolimont-Lobbes Hospital, Lobbes, Belgium; University Hospital Aachen, Aachen, Germany; General Hospital Augsburg, Germany; Charité Campus Virchow Hospital, Berlin, Germany; Kreisklinik Biberach, Germany; Municipal Hospital, Braunschweig, Germany; General Hospital, Celle, Germany; General Hospital Dortmund, Germany; Diakonissenkrankenhaus, Flensburg, Germany; University Hospital, Freiburg, Germany; BG Trauma Hospital, Halle, Germany; University Hospital, Halle, Germany; University Hospital, Hamburg, Germany; Friederikenstift Hospital, Hannover, Germany; Medizinische Hochschule, Hannover, Germany; University Hospital, Homburg, Germany; University Hospital, Jena, Germany; Westpfalz Hospital, Kaiserslautern, Germany; Municipal Hospital Karlsruhe, Germany; University Hospital, Kiel, Germany; SKM Hospital, Koblenz, Germany; University Hospital, Leipzig, Germany; General Hospital, Ludwigsburg, Germany; BG Trauma Hospital, Ludwigshafen, Germany; University Hospital, Mainz, Germany; University Hospital, Magdeburg, Germany; Hospital of the Technical University, Munich, Germany; BG Trauma Hospital, Murnau, Germany; University Hospital, Münster, Germany; Municipal Hospital Nuernberg, Germany; University Hospital, Regensburg, Germany; Klinikum Schwerin, Germany; BG Trauma Hospital, Tübingen, Germany; German Army Hospital, Ulm, Germany; University Hospital, Ulm, Germany; and Sahlgrenska University Hospital, Gothenburg, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
The study has been approved by the ethics commitee of the Saarland phyisician chamber.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The pelvic trauma registry of the DGU.
Rights and permissions
About this article
Cite this article
Rollmann, M.F., Herath, S.C., Holstein, J.H. et al. Surgical treatment of pelvic ring fractures in the elderly now and then: a pelvic registry study. Aging Clin Exp Res 29, 639–646 (2017). https://doi.org/10.1007/s40520-016-0612-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0612-8