Abstract
Background
Frailty is a frequent condition in patients with knee osteoarthritis (KOA). However, there are different constructs on how to define it. Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) is one of them.
Aim
To assess the prevalence of frailty, according to the SHARE-FI definition in patients with symptomatic KOA, and to establish its associated factors.
Methods
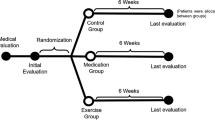
Symptomatic KOA patients were evaluated for pain symptoms, quality of life, comorbidities, ongoing drug therapy, and radiological damage. Patients were categorised according to the SHARE-FI definition into frail, pre-frail, and non-frail, and compared to a group of healthy controls associated by age and gender.
Results
170 symptomatic KOA patients (76.5% female, mean age 70.1 years) and 186 healthy controls were included. According to SHARE-FI criteria, 35 patients (20.6%) were categorised frail, 50 (29.4%) pre-frail, and 85 (50%) non-frail. The prevalence of frail or pre-frail subjects was statistically significantly higher in patients with symptomatic KOA. Stratifying the patients according to the frailty categories, frail subjects showed significantly higher mean values of pain. The results from logistic regression analysis revealed that polypharmacy (p = 0.003), pain (p = 0.016) and comorbidities (p = 0.035) were the variables independently associated with frailty in symptomatic KOA.
Discussion
Frailty or pre-frailty, defined by SHARE-FI, is common in symptomatic KOA. The main factors associated with frailty were polypharmacy, pain and comorbidity burden.
Conclusions
SHARE-FI can represent an useful tool to define frailty in symptomatic KOA.
Similar content being viewed by others
Introduction
Knee osteoarthritis (KOA) is the most prevalent chronic joint disease in the world, and one of the most common sources of pain [1]. Especially in the elderly, KOA is a cause of reduced function, generally concerning mobility and is an important cause of frailty and pre-frailty [2].
In recent years frailty, defined as “a biologic syndrome of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiologic systems, and causing vulnerability to adverse outcomes” [3], has emerged as a significant area of research in rheumatology [4,5,6].
KOA is associated with accelerated biological aging and, as a result, geriatric syndromes like frailty are more likely to present irrespective of chronological age. Data from the European Project on OSteoArthritis (EPOSA) demonstrated that frailty and pre-frailty were, respectively, present in the 10.2% and in the 51.0% of the KOA patients. The odd ratio for developing frailty was 2.96 in KOA patients [7]. Pain is a major contributor in developing frailty in KOA patients. A recent study demonstrated that after adjusting for potential confounders (age, gender, anthropometric and demographic data, comorbidities), people with KOA and pain were significantly more likely to have frailty compared with those with KOA without pain [8].
The association between frailty and polypharmacy is also close in the elderly patient [9, 10]. While there are reports of an association between frailty and polypharmacy, causality has not been demonstrated [11]. A large Australian study has revealed that polypharmacy increases the risk of frailty by more than two times [10]. A better understanding of the relationship between KOA, polypharmacy, and frailty is a key challenge from both a clinical and public health perspective. Identifying risk factors for the development of frailty, in a prevailing condition such as KOA, could guide preventive actions in the most susceptible subjects.
On the other hand, there is no consensus on the frailty definition. To date, there are no studies evaluating the prevalence of frailty in symptomatic KOA according to the Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) definition [12].
Based on these considerations, the aims of this study were to determine the prevalence of frailty from the Research on Osteoarthritis Against Frailty (ROAF) study, and to determine the factors associated with frailty in elderly patients with symptomatic KOA, using the SHARE-FI.
Methods
Subjects
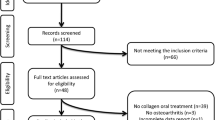
The study population was composed of subjects enrolled in the ROAF study, a study cohort of OA adult patients whose particular focus was to assess the prevalence of frailty and to establish its potential associated independent and combined factors. The patients of the ROAF study enrolled at the Rheumatology Clinic of the Università Politecnica delle Marche from 2018. Patients with symptomatic KOA were consecutively included, diagnosed based on clinical history and objective examination. Pain was the entry criterion, evaluated by the Italian version of the Western Ontario and McMaster Universities OA Index (WOMAC) pain subscale score [13], and in addition three of the following criteria: age ≥ 50 years, morning stiffness < 30 min evaluated by the WOMAC stiffness subscale (score from ‘mild’ to extreme’), crepitus on active motion in at least one knee, bony tenderness in at least one knee, bony enlargement in at least one knee, and no palpable synovial fluid collections or warmth in both knees [14]. All participants were independent in their activities of daily life. Patients on drug treatment for pain with analgesics or non-steroid anti-inflammatory drugs had to be at a stable dosage for at least 2 weeks.
Exclusion criteria were the presence of a coexisting inflammatory joint disease, of medical comorbidities that would render the patient unable to participate fully in study procedures (e.g., terminal conditions such as end-stage renal disease, heart failure or malignancy), alcohol abuse, psychiatric disorder, or previous or planned knee arthroplasty.
Data for the healthy control group were collected from a previous cross-sectional population-based study, called MArche Pain Prevalence INvestigation Group (MAPPING). This study has been described in detail elsewhere [1, 15]. The data collected from 186 healthy controls was used in this study. This sample reflects the age/gender related stratification/distribution of the KOA population under study.
Frailty definition
The definition of frailty used refers to the variables of the SHARE-FI study [12]. The SHARE-FI instrument was created as per the standard procedure [16]. In SHARE-FI, the cut-offs of the frailty categories (i.e., non-frail, pre-frail and frail) are based on latent variable modelling. The variables previously selected by Santos-Eggimann and coworkers were included [17], and were the following. “Exhaustion” was identified with the question: "In the last month, have you had too little energy to do the things you wanted to do?". A positive answer coded as 1, a negative answer as 0. “Weight loss” was identified by reporting a "Diminution in desire for food" in response to the question: "What has your appetite been like?" or, in the case of a non-specific or uncodeable response to this question, by responding "Less" to the question: "So, have you been eating more or less than usual?". The presence of the criterion was coded as 1, its absence as 0. “Slowness” was defined as a positive answer to either of the following two items: "Because of a health problem, do you have difficulty [expected to last more than 3 months] walking 100 m?" or "… climbing one flight of stairs without resting?". One or two positive answers were scored 1, and two negative answers were scored 0. “Low activity” was assessed by the question: "How often do you engage in activities that require a low or moderate level of energy such as gardening, cleaning the car, or doing a walk?". This variable was kept ordinal: 1 = "More than once a week"; 2 = "Once a week"; 3 = One to three times a month" and 4 = "Hardly ever or never". "Weakness" was the only criterion that required instrumental measurement, for which a five-sensor electric dynamometer (FSR-402) was used, connected to a microprocessor Arduino Mega 2560, already employed by our group both in the context of rheumatoid arthritis and fibromyalgia [18]. This variable was kept as continuous, and the other variables were calculated as indicated in the validation work [12].
The parameters above mentioned allowed the calculation of the SHARE-FI. Its translated calculators (one for each sex) are freely accessible on https://sites.google.com/a/tcd.ie/share-frailtyinstrument-calculators/. When data are entered into the calculator, the tool provides a continuous frailty score and enables automatic classification into phenotypic frailty categories.
SHARE-FI has proven to be a tool with good construct and predictive validity [12]. It offers a quick and reliable way to assess and monitor frailty in community dwelling individuals over the age of 50, can help to prioritise subjects access to resources, and can serve as an instrument for audit and research [19].
Demographic, clinical and radiographic variables
Clinical and demographic variables were collected during outpatient visits.
The educational level was considered counting the school years from the first year of primary school.
Body mass index (BMI) was categorised accordingly as normal (18.5 to < 25 kg/m2), overweight (25 to < 30 kg/m2), and obesity (≥ 30 kg/m2).
Polypharmacy has been defined by the presence of a therapy with between five and nine drugs; more than 10 drugs define excessive polypharmacy [9, 10].
The comorbidity burden has been defined with modified Rheumatic Disease Comorbidity Index (mRDCI), calculated with the formula: 1* lung disease and [2* (myocardial infarction, other cardiovascular diseases, or stroke) or 1* hypertension] and 1* (ulcer or other gastrointestinal diseases) and 2* kidney disease and 1* BMI > 30 or 2* if BMI is > 35, and 1 for each of diabetes, fracture, depression and cancer. The index has proved its validity and has already been used in various conditions of rheumatological interest [20].
Pain due to KOA was evaluated with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and its subscales [13, 21].
The Italian version of the 36-item Short Form Health Survey (SF-36) was used as a generic health-related quality of life (HRQoL) scale, computing the two psychometrically based summary measures Physical Component Summary Scale Score (PCS) and Mental Component Summary Scale Score (MCS) [22].
X-rays of the knees were evaluated in the antero-posterior, weight-bearing, semiflexed views. Recent (within one year) images were scored by a musculoskeletal radiologist (MC) according to the Kellgren and Lawrence (K/L) grading system [23].
Statistical analysis
Data were stored in a Microsoft Excel database and have been processed with MedCalc 19.0.6 (statistical software packages for Windows XP). Parametric techniques may be applicable for certain ordinal level data; however, our data were generally normally distributed. The Kolmogorov–Smirnov test was used to determine the normal distribution. The data were generally normally distributed and, however, presented for the sake of exhaustiveness as means and standard deviations (SDs) and as median and interquartile ranges (IQR). In accordance with the SHARE-FI calculation, patients have been categorised into frail, pre-frail or non-frail.
In the symptomatic KOA patients group, the frailty phenotype comparison (dependent variable) was tested with the chi-square test or Fisher’s exact test for comparison with categorical variables. The non-parametric Spearman’s rank correlation coefficient was used to assess the relationships between clinical, functional and radiological measures and SHARE-FI scores. Differences in participant characteristics between patients and controls and between frailty categories were tested with one-way analysis of variance (ANOVA), or Kruskal–Wallis analysis as appropriate. To assess the relative contribution of the single variable (age, sex, disease duration, level of education, polypharmacy, mRDCI, BMI, SF-36, and radiographic OA severity) on the SHARE-FI score (considered as dependent variable), a multivariate logistic regression analysis in symptomatic KOA patients was performed. Analysis with backward elimination included variables that yielded p values of 0.1 or lower in the initial univariate analysis. p values < 0.05 were considered statistically significant.
Results
One-hundred and seventy consecutive symptomatic KOA patients (76.5% females, mean age 70.1 years) were included, 96 (56.5%) complaining symptoms in the right knee and 74 (43.5%) in the left one. The mean duration of KOA symptoms until the diagnosis was 7.5 years (range 1–19 years). The education level was generally low, 43.5% had received only a primary school education, and just 9.4% had received a high school education or more. The majority of the patients (73.5%) were married living family, up to 53.8% were housewives. BMI indicative of overweight were recorded for 59.7% of the patients. The radiological severity of the KOA was predominantly in the second and third degree K/L (respectively, 43.5% and 35.3%). Polypharmacy was very common in our study population, with 53.6% of the subjects receiving 5–9 drugs per day and 13.8% receiving 10 drugs per day or more. Control subjects differed from symptomatic KOA patients for a lower mean comorbid score (mRDCI 3.5 ± 1.9 versus 3.0 ± 2.0; p = 0.042), lower daily drug consumption (3.5 ± 1.9 versus 2.5 ± 2.0; p = 0.002) and a lower mean BMI value (26.8 ± 3.9 versus 25.7 ± 3.3; p = 0.003) (Table 1).
The prevalence of frail or pre-frail subjects was statistically significantly higher in patients with symptomatic KOA. According to SHARE-FI, 35 symptomatic KOA patients (20.6%) were identified as frail, 49 (26.4%) as pre-frail, and 85 (50.0%) as non-frail. In healthy group, 22 subjects (11.8%) were identified as frail, 50 (29.4%) as pre-frail, and 115 (61.8%) as non-frail (chi-squared = 6.77; p = 0.033) (Fig. 1).
By making a gender distinction, male patients were significantly more frail (p = 0.036) than female patients (Fig. 2).
Stratifying symptomatic KOA patients according to the frailty categories, frail patients showed significantly higher mean values of WOMAC Pain (Fig. 3) and SF-36.
The mean number of drugs prescribed increased with increasing frailty in symptomatic KOA patients: 4.1 ± 1.1 in non-frail subjects, 6.0 ± 1.6 in pre-frail subjects, 10.3 ± 1.8 in frail subjects (F-ratio = 239.387, p < 0.001). Moreover, mRDCI differed significantly between in symptomatic KOA patients classified as frail, pre-frail, and non-frail (F-ratio = 73.87, p < 0.001) (Table 2).
The positive correlations of WOMAC pain were significant with SHARE-FI (rho = 0.445, p < 0.0001), polypharmacy (rho = 0.481, p < 0.0001), and mRDCI (rho = 0.311, p < 0.0001). Conversely, WOMAC pain was negatively associated with physical function and psychological distress (SF-36 PCS and SF-36 MCS scales, respectively, rho = − 0.480; p = 0.004 and rho = − 0.256; p = 0.026) (Table 3).
The results from logistic regression analysis revealed that polypharmacy (Wald statistic = 8.740; p = 0.003), WOMAC pain (Wald statistic = 5.828; p = 0.016) and comorbidities (Wald statistic = 4.445; p = 0.035) were independently associated with frailty in symptomatic KOA (Table 4).
Discussion
In this study, we demonstrated an association between symptomatic KOA and frailty. Compared to healthy subjects, frailty and pre-frailty showed a higher prevalence in patients with symptomatic KOA. Frailty seems to be significantly conditioned by polypharmacy and by the presence of comorbidity in patients suffering from symptomatic KOA. For the first time, the definition of frailty covered by SHARE-FI was applied in patients with symptomatic KOA. The SHARE-FI implies a relative ease of use, combining patient-reported evaluations with objective measures such as the assessment of handgrip strength.
From a medical point of view, the term "frail" identifies patients with a reduced ability to effectively compensate for external stressors, and who are consequently at greater risk of negative outcomes, including prolonged hospitalization, institutionalization, worsening disability, and even death [3]. There is an agreement that the biological basis of frailty is multifactorial. Frailty includes dysfunctions of various systems, its risk increases in a non-linear model according to the number of altered systems, and is independent of chronic diseases and chronological age. In literature, different criteria have been validated to identify frail older subjects, which mainly refer to two conceptual models: the physical frailty phenotype proposed by Fried [3], and the cumulative deficit approach proposed by Rockwood [16, 24].
A number of studies have demonstrated a significant relationship between KOA and frailty [25, 26]. Symptomatic KOA predisposes affected individuals to multiple variables included in the definition of frailty, including sarcopenia, fatigue and low activity. Symptomatic KOA, particularly if characterised by significant painful symptoms, is a condition that the clinician must be able to manage to avoid the appearance or worsening of frailty. This study also investigated the presence of collateral variables involved in the increased risk of frailty, emerging polypharmacy and comorbidities as two conditions that are associated to frailty. In our cohort, we found an overall prevalence of frailty in KOA of 20.6%, a higher rate than described by Fried and colleagues (6.9%) [3] and by other European studies [2, 7]. These differences may depend on several factors, the main one seems to be the definition of frailty itself. From large multicentre and multinational studies, it emerges that frailty affects 10.2% of subjects aged 65–85 years, and OA increases the probability of frailty by a factor of 2.96 compared to subjects without OA [7]. Some differences have also been documented on a geographical basis, finding in Mediterranean countries (Italy and Spain) an increased risk of frailty.
The association between KOA-related pain and frailty can be clarified by a variety of interconnected mechanisms, and has already been demonstrated in several cohort studies, and the presence of moderate or severe knee pain increases the likelihood of pre-frailty or frailty [27]. Bilateral knee pain increases this probability, both for pre-frailty and frailty, compared to monolateral symptomatology.
The fact that the more severe the pain and the greater the condition of frailty also emerges from cross-sectional studies [28]. Persistent pain contributes to and accelerates the onset of frailty or development of frailty in elderly people through mechanisms involving reduced movement ability, decreased nutritional intake, and finally the onset of new comorbidities such as depression [29]. Besides the symptomatology due to KOA, a certain importance is also covered by radiological damage. Radiological damage on a symptomatic KOA would seem to confer an additional risk of frailty [2].
The pain symptom, however, when connoted by particular characteristics of pervasiveness, is the major determinant of frailty within KOA [30], and remains such even without considering associated confounding factors such as depression and the use of opioid drugs. Pain also translates into an increased risk of falling with the consequent unfavourable outcomes [31].
Our study confirmed an already known association between polypharmacy and frailty [3]. On average, frail subjects consume more drugs, and this finding is also directly related to comorbidities. Frail subjects, frequently elderly, suffer from multiple chronic diseases, such as cardiovascular diseases and hypertension, obesity, respiratory diseases, and type II diabetes mellitus [32]. Polypharmacy, defined as five prescribed drugs or more, in our case history covered more than two thirds of the sample. This confirms the existence of a gradient between the number of drugs prescribed and the prevalence of frailty. Polypharmacy and excessive polypharmacy (10 drugs or more) are a common condition in subjects over 75 years, reported with a frequency of 34% and 23%, respectively [33]. After adjustment for socio-demographic and health variables, polypharmacy and excessive polypharmacy were associated with frailty with a probability ratio of 1.77 and 4.47, respectively. Chronic KOA pain is also a predisposing factor for polypharmacy, since it increases the consumption of opioid and non-opioid analgesic drugs [34, 35]. Although analgesics can alleviate painful symptoms, their use in older people is characterised by an increased risk of adverse events (falls, fractures, and delirium) due to the pharmacokinetic and pharmacodynamic changes common in old age [35]. Polypharmacy also increases the risk of inappropriate prescription [36], drug interactions [37], and overall adverse events including functional impairment and hospitalisation [38]. To all effects, polypharmacy is to be considered a factor predisposing to frailty [39].
Finally, when considering the limitations of the study, mention should be made of the cross-sectional assessment, which does not provide evidence of causality. Furthermore, the vast majority of the data collected are patient-reported measures affected by possible recall errors. Another limitation of the study is that the potential effect of analgesic/anti-inflammatory treatment was not considered, recruiting patients with symptomatic KOA both in treatment and out of treatment.
Conclusions
The results of this study suggest that pre-frailty and frailty, measured with SHARE-FI, are common in the symptomatic KOA patients. Pain, together with comorbidities and polypharmacy are the main determinants of frailty in the course of symptomatic KOA. Further studies are needed to identify in detail the pathophysiological mechanisms of these associations to provide effective treatment strategies.
Availability of data and material
The data are available upon reasonable request to the corresponding author.
References
Salaffi F, De Angelis R, Grassi W, MArche Pain Prevalence; INvestigation Group (MAPPING) study (2005) Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. I. The MAPPING study. Clin Exp Rheumatol 23:819–828
Misra D, Felson DT, Silliman RA et al (2015) Knee osteoarthritis and frailty: findings from the Multicenter Osteoarthritis Study and Osteoarthritis Initiative. J Gerontol A Biol Sci Med Sci 70:339–344
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Salaffi F, Di Carlo M, Farah S et al (2019) Prevalence of frailty and its associated factors in patients with rheumatoid arthritis: a cross-sectional analysis. Clin Rheumatol 38:1823–1830
Salaffi F, Farah S, Di Carlo M (2020) Frailty syndrome in rheumatoid arthritis and symptomatic osteoarthritis: an emerging concept in rheumatology. Acta Biomed 91:274–296
Andrews JS, Trupin L, Yelin EH et al (2017) Frailty and reduced physical function go hand in hand in adults with rheumatoid arthritis: a US observational cohort study. Clin Rheumatol 36:1031–1039
Castell MV, van der Pas S, Otero A et al (2015) Osteoarthritis and frailty in elderly individuals across six European countries: results from the European Project on OSteoArthritis (EPOSA). BMC Musculoskelet Disord 16:359
Veronese N, Maggi S, Trevisan C et al (2017) Pain increases the risk of developing frailty in older adults with osteoarthritis. Pain Med 18:414–427
Gnjidic D, Hilmer SN, Blyth FM et al (2012) High-risk prescribing and incidence of frailty among older community-dwelling men. Clin Pharmacol Ther 91:521–528
Herr M, Robine JM, Pinot J et al (2015) Polypharmacy and frailty: prevalence, relationship, and impact on mortality in a French sample of 2,350 old people. Pharmacoepidemiol Drug Saf 24:637–646
Gnjidic D, Hilmer SN (2012) Potential contribution of medications to frailty. J Am Geriatr Soc 60:401
Romero-Ortuno R, Walsh CD, Lawlor BA et al (2010) A frailty instrument for primary care: findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). BMC Geriatr 10:57
Salaffi F, Leardini G, Canesi B et al (2003) Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560
Zhang W, Doherty M, Peat G et al (2010) EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 69:483–489
Salaffi F, De Angelis R, Stancati A, Grassi W, MArche Pain; Prevalence INvestigation Group (MAPPING) study (2005) Health-related quality of life in multiple musculoskeletal conditions: a cross-sectional population based epidemiological study. II. The MAPPING study. Clin Exp Rheumatol 23:829–839
Searle SD, Mitnitski A, Gahbauer EA et al (2008) A standard procedure for creating a frailty index. BMC Geriatr 8:24
Santos-Eggimann B, Cuénoud P, Spagnoli J et al (2009) Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci 64:675–681
Salaffi F, Farah S, Di Carlo M (2020) Force-time curve features of handgrip strength in fibromyalgia syndrome. Sci Rep 10:3372
Romero-Ortuno R, O'Shea D, Kenny RA (2011) The SHARE frailty instrument for primary care predicts incident disability in a European population-based sample. Qual Prim Care 19:301–309
Iannone F, Salaffi F, Fornaro M et al (2018) Influence of baseline modified Rheumatic Disease Comorbidity Index (mRDCI) on drug survival and effectiveness of biological treatment in patients affected with Rheumatoid arthritis, Spondyloarthritis and Psoriatic arthritis in real-world settings. Eur J Clin Invest 48:e13013
Bellamy N, Buchanan W, Goldsmith CH et al (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis in the knee or the hip. J Rheumatol 30:167–178
Apolone G, Mosconi P (1998) The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol 51:1025–1036
Salaffi F, Carotti M, Stancati A et al (2003) Radiographic assessment of osteoarthritis: analysis of disease progression. Aging Clin Exp Res 15:391–404
Moorhouse P, Rockwood K (2012) Frailty and its quantitative clinical evaluation. J R Coll Phys Edinb 42:333–340
Miguel Rde C, Dias RC, Dias JM et al (2012) Frailty syndrome in the community-dwelling elderly with osteoarthritis. Rev Bras Reumatol 52:331–347
Misra D, Felson DT, Silliman RA et al (2015) Knee osteoarthritis and frailty: findings from the multicenter osteoarthritis study and osteoarthritis initiative. J Gerontol A Biol Sci Med Sci 70:339–344
Wade KF, Lee DM, McBeth J et al (2016) Chronic widespread pain is associated with worsening frailty in European men. Age Ageing 45:268–274
Weaver GD, Kuo YF, Raji MA et al (2009) Pain and disability in older Mexican-American adults. J Am Geriatr Soc 57:992–999
Rudy TE, Weiner DK, Lieber SJ et al (2007) The impact of chronic low back pain on older adults: a comparative study of patients and controls. Pain 131:293–301
Mezuk B, Edwards L, Lohman M et al (2012) Depression and frailty in later life: a synthetic review. Int J Geriatr Psychiatry 27:879–892
Stubbs B, Binnekade T, Eggermont L et al (2014) Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil 95:175–187
Grant JF, Martin SA, Taylor AW et al (2014) Cohort profile: the men androgen inflammation lifestyle environment and stress (MAILES) study. Int J Epidemiol 43:1040–1053
Jyrkka J, Enlund H, Korhonen MJ et al (2009) Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75+ study: a cross-sectional analysis. Drugs Aging 26:493–503
Koponen MPH, Bell JS, Karttunen NM et al (2013) Analgesic use and frailty among community-dwelling older people: a population-based study. Drugs Aging 30:129–136
O’Neil CK, Hanlon JT, Marcum ZA (2012) Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother 10:331–342
Bradley MC, Motterlini N, Padmanabhan S et al (2014) Potentially inappropriate prescribing among older people in the United Kingdom. BMC Geriatr 14:72
Fialova D, Onder G (2009) Medication errors in elderly people: contributing factors and future perspectives. Br J Clin Pharmacol 67:641–645
Wallace E, Stuart E, Vaughan N et al (2014) Risk prediction models to predict emergency hospital admission in community-dwelling adults: a systematic review. Med Care 52:751–765
Salaffi F, Di Carlo M, Farah S et al (2020) The Comprehensive Rheumatologic Assessment of Frailty (CRAF): development and validation of a multidimensional frailty screening tool in patients with rheumatoid arthritis. Clin Exp Rheumatol 38:488–499
Acknowledgments
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement.
Funding
No funding source to be declared for this study.
Author information
Authors and Affiliations
Contributions
FS, MC and AG gave substantial contributions to the conception and design of the work. FS, SF, and MDC performed the clinical data collection. FS was the major contributor in writing the manuscript and performed the statistical analysis. MC and AG analysed X-rays of the knees. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
All the procedures conducted in this study were in accordance with the 1964 Helsinki Declaration and its later amendments. The study was approved by the local ethics committee (Comitato Etico Unico Regionale, prot. no 22418).
Consent to participate
All patients gave written informed consent for participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salaffi, F., Di Carlo, M., Carotti, M. et al. Frailty prevalence according to the Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) definition, and its variables associated, in patients with symptomatic knee osteoarthritis: findings from a cross-sectional study. Aging Clin Exp Res 33, 1519–1527 (2021). https://doi.org/10.1007/s40520-020-01667-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01667-0