Abstract
Background:
Bone is one of the most common sites of distant metastasis in breast cancer. The purpose of this study was to combine selected clinical and pathologic variables to develop a nomogram that can predict the likelihood of bone-only metastasis (BOM) as the first site of recurrence in patients with early breast cancer.
Methods:
Medical records of patients with non-metastatic breast cancer were retrospectively collected. On the basis of the analysis of patient and tumour characteristics using the Cox proportional hazards regression model, a nomogram to predict BOM was constructed for a 4175-patient-training cohort. The nomogram was validated in an independent cohort of 579 patients.
Results:
Among 4175 patients with non-metastatic breast cancer, 314 developed subsequent BOM. Age, T classification, lymph node status, lymphovascular space invasion, and hormone receptor status were significantly and independently associated with subsequent BOM. The nomogram had a concordance index of 0.69 in the training set and 0.73 in the validation set.
Conclusions:
We have developed a clinical nomogram to predict subsequent BOM in patients with non-metastatic breast cancer. Selection of a patient population at high risk for BOM could facilitate research of more specific staging approaches or the selective use of bone-targeted therapy.
Similar content being viewed by others
Main
Bone is the first site of distant disease in 25–40% of patient with metastatic breast cancer, and ∼60–80% of patients with recurrent disease have skeletal involvement (Coleman 1997).
Breast cancers are heterogeneous tumours that result from several molecular progression pathways (Esteva et al, 2002). Analyses of breast cancer progression suggest that the disease preferentially metastasises to the bone, with or without metastasis to visceral organs, loco-regional sites, or the brain (Smid et al, 2008; Kennecke et al, 2010). Several hypotheses have been developed to explain this phenomenon, including the favourable chemokine milieu or microenvironment of the bone and intrinsic molecular features of cancer cells (Kang et al, 2003; Jones et al, 2006; Smid et al, 2006; Jamieson-Gladney et al, 2011). Although these hypotheses are promising, clinicians are still determining prognosis on the basis of anatomical characteristics such as tumour size or nodal status, in addition to biological information like tumour grade, hormone receptor status, human epidermal growth factor 2 (HER2) status, and proliferation. These factors, however, evaluate the risk of metastasis in general, while predictors of bone-only metastasis (BOM) remain a clinical uncertainty (Galea et al, 1992; Hess et al, 2003; Millar et al, 2009).
Nomograms constructed on the basis of known prognostic factors are increasingly being used to predict specific outcomes (Rouzier et al, 2005; Werkoff et al, 2009; Graesslin et al, 2010). The purpose of this study was to develop and validate a nomogram based on clinical and pathologic variables that is able to predict the likelihood of BOM in patients with early breast cancer. Such a nomogram, after validation, could be used to identify a subgroup of patients who may benefit from adjuvant bisphosphonates (or other bone-specific targeted agents) (Wong et al, 2012), or develop radiologic screening and novel preventive treatment strategies for patients with early-stage breast cancer, potentially improving quality of life measures, if not improving disease outcomes as well.
Patients and Methods
Study population
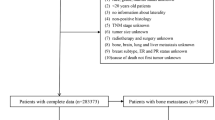
We searched the clinical database of the Department of Breast Medical Oncology at The University of Texas MD Anderson Cancer Center (Houston, Texas) for the medical records of all patients with stage I–III breast cancer at diagnosis who presented to MD Anderson Cancer Center for treatment between January 1997 and December 2004. We identified 4175 consecutive patients with primary non-metastatic breast cancer. This cohort was used as a training set to develop a model to predict BOM in a population of non-metastatic breast cancer patients. A second cohort that consisted of 579 breast cancer patients referred to Tenon Hospital (Paris, France) between January 2003 and December 2005 was used as a validation set. The Institutional Review Board of MD Anderson Cancer Center approved the study.
Patient characteristics
The clinical and histologic characteristics of all patients were acquired retrospectively from MD Anderson Cancer Center institutional electronic databases and from Tenon Hospital medical records (Table 1). Clinical tumour stage was determined at presentation by physical examination and standard-of-care imaging modalities (mammography, ultrasonography, computerised tomography (CT), and/or bone scans), and tumour biology (biomarkers) was determined before any treatment initiation. No central pathology review was performed, but for the MD Anderson cohort, a breast pathologist reviewed all outside pathology reports and stained slides at the time of referral to the centre. As institutional policy at MD Anderson Cancer Center, unstained slides are requested on rare occasions when discrepancy exists between the outside report and the review performed at MD Anderson Cancer Center. Similarly, for the Tenon cohort, the outside pathology reports were reviewed only when discordance was found between the diagnostic biopsy and the final report based on the surgical specimen. Oestrogen receptor (ER), progesterone receptor (PR), and HER2 measurements were available for all patients.
As our study period predates the American Society of Clinical Oncology’s recommendation for ER and PR positivity/negativity thresholds (Hammond et al, 2010), ER and PR positivity were each defined as nuclear staining ⩾10%, and HER2 positivity was defined as 3+ staining on immunohistochemistry or gene amplification by FISH. For our retrospective data analysis, we grouped the tumours according to hormone receptor (HR) status as follows: positive (ER+ and/or PR+) or negative (ER− and PR−). In the MD Anderson cohort, the grade was defined according to the modified Black’s nuclear grade. In the Tenon cohort, the tumour grade was defined according to the modified Scarff–Bloom–Richardson system. In both institutions, the number of histologically positive axillary lymph nodes was determined after surgery by examination of serial macroscopic sections of each node.
Patients received neoadjuvant and/or adjuvant systemic therapy (endocrine therapy and/or chemotherapy) according to their TNM classification and standard-of-care recommendations. In the MD Anderson cohort, 1636 patients received neoadjuvant chemotherapy, and all patients underwent breast and axillary surgery. However, some details were missing in 13% of the patients in the MD Anderson cohort.
Overall survival was measured from the date of diagnosis of primary cancer to the date of death from any cause. Patients who were alive at last follow-up were censored. Time to isolated bone metastasis was calculated from the date of diagnosis to the date of BOM. In this study, BOM was defined as the group of patients with bone-only disease, as demonstrated by current standard-of-care staging workup, which entailed the use of bone scans and/or positron emission tomography (PET) scans/PET–CT scans. As needed, confirmatory studies were conducted using CT scans, MRI, and plain X-ray films, as well as biopsy of an identified solitary lesion. Patients with metastasis other than bone (with or without bone metastasis) at the first recurrence were censored.
Nomogram development and statistical analyses
The χ2-test and Student’s t-test were used to compare patient characteristics by cohort origin (training cohort vs validation cohort).
Univariate analysis was performed using the log-rank test to assess the association between clinical–pathological variables and the risk of BOM. The following variables were tested: age at diagnosis (<35 years, 35–50 years, >50 years), menopausal status, race, T classification at diagnosis (T1, T2, T3), lymphovascular space involvement, axillary lymph node metastasis, nuclear grade, HR status, and HER2 status.
Cox proportional hazards regression was used for multivariate analysis. This model was then used to predict individual patient probability of BOM. Variables were eliminated from the model if their removal improved the overall model quality (as measured by the Akaike information criterion). P-values <0.05 were considered significant.
The Cox proportional hazards regression model was used to construct the nomogram. The model performance was quantified with respect to discrimination and calibration. Discrimination (i.e., whether the relative ranking of individual predictions is in the correct order) was quantified using the concordance index. The concordance index ranges from 0 to 1, with 1 indicating perfect concordance, 0.5 indicating no better concordance than chance, and 0 indicating perfect discordance. The 95% confidence interval (CI) was obtained by bootstrapping (1000 repetitions).
There is no accepted test to assess the calibration (i.e., agreement between observed outcome frequencies and predicted probabilities) of a censored model. Calibration was studied with graphical representations of relationships between the predicted probability of BOM and the observed frequencies of BOM in the validation set. The grouped proportions of BOM vs the mean predicted probabilities were represented at 3, 5, 7, and 10 years. The average absolute difference between the lowest estimated calibration curve and the line of identity was measured. All analyses were performed using the R package with the survival, r.m.s., and Hmisc libraries (http://lib.stat.cmu.edu/R/CRAN/).
To illustrate whether this nomogram can optimise the design of clinical trials of bone-specific metastasis prevention measures, we designed a virtual prevention trial. We determined the theoretical sample size required to test the efficacy of an experimental bone-modifying drug, such as a bisphosphonate, for preventing bone metastases in a population of patients with early breast cancer at 7 years after diagnosis. The sample size in the virtual trial was calculated using a two-arm binomial design. (http://www.swogstat.org/stat/public/binomial_twoarm.htm) to demonstrate a benefit with α=5% and a power of 80%. The nomogram at 7 years was used to select several subgroups of patients at risk for BOM according to different cutoffs of probability. The rate of BOM in each group was calculated based on the training set before year 7. Relative risk reductions (15, 25, and 35%) of isolated bone metastases were tested.
Results
Prediction of bone-only metastases in the MD Anderson cohort (training set)
In the MD Anderson cohort, the first site of recurrence was BOM in 314 patients, bone and concurrent visceral or soft tissue metastases in 329 patients, and a non-bone distant metastasis in 658 patients (Table 2). Comparisons were performed between those who developed BOM and the rest of the patient cohort, regardless of disease outcome. The majority of the MD Anderson patients received anthracycline-based adjuvant chemotherapy, in addition to adjuvant hormonal therapy and/or adjuvant radiation therapy (Table 1), as deemed necessary for the individual patient. The probabilities of developing BOM were 5% (95% CI, 5.7–4.3), 8.1% (95% CI, 9.1–7.1), and 10.2% (95% CI, 11.4–9%) at 3, 5, and 7 years, respectively. The median follow-up times for patients with BOM and patients with non-BOM disease were 66 months (range, 9–259) and 60 months (range, 3–477), respectively.
Upon univariate analysis, BOM was strongly associated with HR-positive tumours (P<0.001; Table 3). The other factors correlated with BOM were younger age (age <35 years), T2 or T3 classification at diagnosis, lymphovascular space involvement, and axillary lymph node involvement. However, BOM was not associated with histologic subtype (P=0.4 for ductal carcinoma vs lobular carcinoma), grade (P=0.7), multifocality (P=0.7), or HER2 status (P=0.6).
All of the covariates, except for menopausal status, significant on univariate analysis were still significant after multivariate hazard ratio regression analysis (P<0.001 for all covariates). On the basis of the covariates independently associated with BOM, we constructed a nomogram, and probabilities of BOM were reported at 3, 5, 7, and 10 years (Figure 1). The prediction model had a good concordance index, 0.69 (95% CI, 0.68–0.71), in the training set (internal validation).
External validation of the nomogram
Compared with patients in the MD Anderson cohort, those in the Tenon cohort were older, had smaller (stage T1) and lower-grade (grade I/II) tumours, and had more ER+ and/or PR+ tumours (Table 1). Endocrine therapy alone was more often used in the Tenon cohort than in the MD Anderson cohort, and fewer patients received treatment with chemotherapy alone. Patients in the Tenon cohort had fewer distant recurrences, but the proportion of BOM compared with other sites of metastasis was higher (28 out of 67; 42%) in the Tenon cohort than in the MD Anderson cohort (314 out of 1301; 24%).
The concordance index of the nomogram in the external validation model was 0.73 (95% CI, 0.68–0.79). Of note, the nomogram was well calibrated at 3, 5, 7, and 10 years, with a slight underestimation in the validation set (Figure 2). The mean absolute error in predicted probabilities was 2.3%, and the 0.9 quintile of absolute errors was 4%.
Clinical utility of the nomogram
Once the nomogram had been developed using commonly measured clinical covariates, we sought to use it to identify a subgroup of patients at high risk of developing isolated bone metastasis. Our virtual prevention trial showed that the nomogram would help to select patients with a higher risk of BOM for a clinical trial. As shown in Table 4, the number of patients for clinical/translational trials could be markedly reduced if patient selection was based on the results of this nomogram.
Discussion
Using a large retrospective database, we developed the first clinical nomogram to predict the likelihood of BOM for patients diagnosed with non-metastatic breast cancer. We validated this nomogram with an independent cohort having different tumour characteristics, prognoses, and outcomes, supporting the excellent exportability of our model. Although some models have been developed to predict the risk of breast cancer recurrence (Mazouni et al, 2011), few are validated to specifically predict the risk of bone metastasis in patients with breast cancer. On the basis of 855 breast cancer samples, Zhou and Liu, (2014) identified eight genetic pathways significantly associated with metastasis to bone. By integrating these pathways into one molecular, computational model, patients at high and low risks for developing bone metastasis were identified. Importantly, other genetic pathways, characterised by non-bone metastasis, were also discerned. Further analysis revealed that the major difference between these two metastatic pathways (bone and non-bone) was that certain dysregulated immune genes (FAS, IL2RG, and IL7R) were more strongly associated with bone metastasis from breast cancer.
It has been demonstrated that the ER-positive status is correlated with the development of bone metastasis (Coleman et al, 1998; Diel, 2001; Hess et al, 2003). Our model substantiates such findings, and shows that patients with HR-positive breast cancer have an increased risk of bone metastases (hazard ratio=1.66; 95% CI, 1.25–2.2), as well as a 10.2% absolute probability of developing bone metastasis after 7 years. However, the other factors analysed are also in agreement with those reported by the International Breast Cancer Study Group, which found that a higher number of involved nodes, larger tumour size, and tumour oestrogen expression were associated with BOM as well (Colleoni et al, 2000).
Several studies conducted on murine models have shown that metastatic lesions can lead to further metastatic spread (Klein, 2009). Therefore, preventing metastasis may reduce the risk of subsequent (secondary) metastatic progression. Agents that may interrupt metastasis to certain organs may help to alter the natural history of the disease, such as the inhibition of bone resorption and osteoclast activity on bone metastasis. A meta-analysis showed that the adjuvant use of zoledronic acid improves overall survival, distant metastasis-free survival, bone metastasis-free survival, and the fracture-free rate in patients with early-stage breast cancer (He et al, 2013). Nonetheless, the use of bisphosphonates as adjuvant therapy remains controversial. A growing body of evidence, however, indicates that adjuvant bisphosphonates may be effective in preventing bone metastasis in patients who are postmenopausal for more than 5 years (Gnant et al, 2009, 2011; Eidtmann et al, 2010; Coleman et al, 2011; Marshall et al, 2012). Although the benefits of bisphosphonates are not limited only to those who develop bone disease, by identifying a patient population at higher risk for BOM, this nomogram may be used as a research tool to resolve controversies surrounding the adjuvant use of bisphosphonates, and better understand the prevention or treatment of bone-specific metastasis.
In adult knock-in mice made to express chimeric (murine/human) receptor activator of nuclear factor-κB ligand (RANKL), denosumab, a fully human monoclonal antibody to RANKL, suppresses bone resorption and increases bone mineral density (Kostenuik et al, 2009). Similarly, dasatinib, a SRC tyrosine kinase inhibitor, has been shown to block cellular proliferation, along with various activities required for metastasis and osteoclast activity (Araujo and Logothetis, 2010). Therefore, with the availability of drugs that may have a preferential effect on particular metastatic organ sites (e.g., bone), this nomogram can be used to facilitate future clinical trials by enriching the patient population needed, resulting in a smaller study without compromising power (Graesslin et al, 2010). Much like the risk assessment process proved successful in selecting patients for preventive trials (Fisher et al, 1998), it can be hypothesised that nomograms will prove to be essential tools in the selection of clinical trial participants.
We validated our nomogram with respect to good discrimination and calibration by testing it in a different population. Because of censored data, the discrimination could not be determined using the classical area under the receiver-operating curve. Thus, we report the concordance index, which indicates whether the relative ranking of individual prediction is in the correct order. The concordance index was good in both the training set and the validation set. The calibration between the training and validation sets gives an idea of a model’s performance when extrapolated to new patient populations. In our case, the Tenon cohort characteristics were clearly different from the MD Anderson ones, but the calibration was still consistent. Consequently, we can speculate that because the nomogram worked in these two different populations, it will work in other groups of patients as well.
There is a complicated interface between breast cancer cells and the bone microenvironment (Korde and Gralow, 2011). Bone marrow can be a sanctuary for cancer cells, and bone marrow micrometastases not only lead to subsequent bone relapse, but distant metastasis and overall poor disease outcome as well (Braun et al, 2005; Bidard et al, 2008). Lipton et al, (2011) have reported a biochemical marker of bone resorption, which reflects alterations in bone turnover and predicts bone metastasis. Other groups have focused on microarray multigene expression profiles that may also be predictive of bone metastases from breast cancer. However, there is still no validated marker or molecular signature to predict an increased risk of subsequent bone metastasis (Kang et al, 2003; Minn et al, 2005; Smid et al, 2006). Prediction models using routine clinical variables and multigene signatures have been compared and shown to be complementary (Lee et al, 2010). Future studies that combine a clinical nomogram with relevant molecular markers and a genomic signature may be the best solution for obtaining accurate predictions.
This study has several limitations. Patients in both cohorts were retrospectively selected from prospectively maintained databases, and bone metastases were diagnosed as part of routine care. Some patients might have had undiagnosed, asymptomatic, or isolated bone metastases, meaning that the actual rate of isolated bone metastases may have been higher than our findings indicate. However, we think that this potential source of bias makes our results more relevant for everyday practice because systematic screening is not currently recommended. A small proportion of patients may also have received bisphosphonates for concomitant osteoporosis. This confounding factor would make the correlation between the covariates and the BOM outcome more difficult to detect, and therefore renders the observed significant associations even more remarkable. Finally, nodal status was assessed at the time of surgery, after some patients had received neoadjuvant chemotherapy. This may have generated an underestimation of nodal status, which is a parameter in the final model. This potential bias concerns patients who achieved a pathologic complete response, but was likely balanced by the very large number of patients in the cohort. In conclusion, we have developed a nomogram that is able to predict isolated bone metastases in patients diagnosed with non-metastatic breast cancer. Use of this nomogram could enrich the selection of patient populations for clinical trials.
Change history
29 September 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Araujo J, Logothetis C (2010) Dasatinib: a potent src inhibitor in clinical development for the treatment of solid tumors. Cancer Treat Rev 36: 492–500.
Bidard FC, Vincent-Salomon A, Gomme S, Nos C, de Rycke Y, Thiery JP, Sigal-Zafrani B, Mignot L, Sastre-Garau X, Pierga JY (2008) Disseminated tumor cells of breast cancer patients: a strong prognostic factor for distant and local relapse. Clin Cancer Res 14: 3306–3311.
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Commbes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Perga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353: 793–802.
Coleman RE (1997) Skeletal complications of malignancy. Cancer 80: 1588–1594.
Coleman RE, Marshall H, Cameron D, Dodwell D, Burkinshaw R, Keane M, Gil M, Houston SJ, Grieve RJ, Barrett-Lee PJ, Ritchie D, Pugh J, Gaunt C, Rea U, Peterson J, Davies C, Hiley V, Gregory W, Bell R (2011) Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med 365: 1396–1405.
Coleman RE, Smith P, Rubens RD (1998) Clinical course and prognostic factors following bone recurrence from breast cancer. Br J Cancer 77: 336–340.
Colleoni M, O’Neill A, Goldhirsch A, Gelber RD, Bonetti M, Thurlimann B, Price KN, Castiglione-Gertsch M, Coates AS, Lindtner J, Collins J, Senn HJ, Cavalli F, Forbes J, Gudgeon A, Simoncini E, Cortes-Funes H, Veronesi A, Fey M, Rudenstam CM (2000) Identifying breast cancer patients at high risk for bone metastases. J Clin Oncol 18: 3925–3935.
Diel IJ (2001) Prognostic factors for skeletal relapse in breast cancer. Cancer Treat Rev 27: 153–157,, discussion 159–164.
Eidtmann H, de Boer R, Bundred N, Llombart-Cussac A, Davidson N, Neven P, von Minckwitz G, Miller J, Schenk N, Coleman R (2010) Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann Oncol 21: 2188–2194.
Esteva FJ, Sahin AA, Cristofanilli M, Arun B, Hortobagyi GN (2002) Molecular prognostic factors for breast cancer metastasis and survival. Semin Radiat Oncol 12: 319–328.
Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, Vogel V, Robidoux A, Dimitrov N, Atkins J, Daly M, Wieand S, Tan-Chiu E, Ford L, Wolmark K (1998) Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90: 1371–1388.
Galea MH, Blamey RW, Elston CE, Ellis IO (1992) The Nottingham Prognostic Index in primary breast cancer. Breast Cancer Res Treat 22: 207–219.
Gnant M, Mlineritsch B, Schippinger W, Luschin-Ebengreuth G, Postlberger S, Menzel C, Jakesz R, Seifert M, Hubalek M, Bjelic-Radisic V, Samonigg H, Tausch C, Eidtmann H, Steger G, Kwasny W, Dubsky P, Fridrik M, Fitzal F, Steirer M, Rucklinger E, Greil R, Marth C (2009) Endocrine therapy plus zoledronic acid in premenopausal breast cancer. N Engl J Med 360: 679–691.
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C, Jakesz R, Seifert M, Hubalek M, Pristauz G, Bauernhofer T, Eidtmann H, Eiermann W, Steger G, Kwasny W, Dubsky P, Hochreiner G, Forsthuber EP, Fesl C, Greil R (2011) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol 12: 631–641.
Graesslin O, Abdulkarim BS, Coutant C, Huguet F, Gabos Z, Hsu L, Marpeau O, Uzan S, Pusztai L, Strom EA, Hortobagyi GN, Rouzier R, Ibrahim NK (2010) Nomogram to predict subsequent brain metastasis in patients with metastatic breast cancer. J Clin Oncol 28: 2032–2037.
Hammond MEH, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FCG, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American Society of Clinical Oncology/College fo American Pathologists Guidleine recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28: 2784–2795.
He M, Fan W, Zhang X (2013) Adjuvant zoledronic acid therapy for patients with early stage breast cancer: an updated systematic review and meta-analysis. J Hematol Oncol 6: 80–88.
Hess KR, Pusztai L, Buzdar AU, Hortobagyi GN (2003) Estrogen receptors and distinct patterns of breast cancer relapse. Breast Cancer Res Treat 78: 105–118.
Jamieson-Gladney WL, Zhang Y, Fong AM, Meucci O, Fatatis A (2011) The chemokine receptor CX(3)CR1 is directly involved in the arrest of breast cancer cells to the skeleton. Breast Cancer Res 13: R91.
Jones DH, Nakashima T, Sanchez OH, Kozieradzki I, Komarova SV, Sarosi I, Morony S, Rubin E, Sarao R, Hojilla CV, Komnenovic V, Kong YY, Schreiber M, Dixon SJ, Sims SM, Khoka R, Wada T, Penninger JM (2006) Regulation of cancer cell migration and bone metastasis by RANKL. Nature 440: 692–696.
Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C, Guise TA, Massague J (2003) A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 3: 537–549.
Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, Nielsen TO, Gelmon K (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28: 3271–3277.
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cancer 9: 302–312.
Korde LA, Gralow JR (2011) Can we predict who’s at risk for developing bone metastases in breast cancer? J Clin Oncol 29: 3600–3604.
Kostenuik PJ, Nguyen HQ, McCabe J, Warmington KS, Karuhara C, Sun N, Chen C, Li L, Cattley RC, Van G, Scully S, Elliot R, Grisanti M, Morony S, Tan HL, Asuncion F, Li X, Ominsky MS, Stolina M, Dwyer D, Dougall WC, Hawkins N, Boyle WJ, Simonet WS, Sullivan JK (2009) Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. J Bone Miner Res 24: 182–195.
Lee JK, Coutant C, Kim YC, Qi Y, Theodorescu D, Symmans WF, Baggerly K, Rouzier R, Pusztai L (2010) Prospective comparison of clinical and genomic multivariate predictors of response to neoadjuvant chemotherapy in breast cancer. Clin Cancer Res 16: 711–718.
Lipton A, Chapman JA, Demers L, Shepherd LE, Han L, Wilson CF, Pritchard KI, Leitzel KE, Ali SM, Pollak M (2011) Elevated bone turnover predicts for bone metastasis in postmenopausal breast cancer: results of NCIC CTG MA.14. J Clin Oncol 29: 3605–3610.
Marshall H, Gregory W, Bell R, Cameron DA, Dodwell DJ, Keane MM, Gil MJ, Davies C, Coleman RE (2012) Adjuvant therapy with zoledronic acid (AZURE-BIG 01/04): The influence of menopausal status and age on treatment effects. J Clin Oncol 30: 502.
Mazouni C, Bonnier P, Romain S, Martin PM (2011) A nomogram predicting the probability of primary breast cancer survival at 2- and 5-years using pathological and biological tumor parameters. J Surg Oncol 103: 746–750.
Millar EK, Graham PH, O'Toole SA, McNeil CM, Browne L, Morey AL, Eggleton S, Beretov J, Theocharous C, Capp A, Nasser E, Kearsley JH, Delaney G, Papadatos G, Fox C, Sutherland L (2009) Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol 27: 4701–4708.
Minn AJ, Kang Y, Serganova I, Gupta GP, Giri DD, Doubrovin M, Ponomarev V, Gerald WL, Blasberg R, Massague J (2005) Distinct organ-specific metastatic potential of individual breast cancer cells and primary tumors. J Clin Invest 115: 44–55.
Rouzier R, Pusztai L, Delaloge S, Gonzalez-Angulo AM, Andre F, Hess KR, Buzdar AU, Garbay JR, Spielmann M, Mathieu MC, Symmans WF, Wagner P, Atallah D, Valero V, Berry DA, Hortobagyi GN (2005) Nomograms to predict pathologic complete response and metastasis-free survival after preoperative chemotherapy for breast cancer. J Clin Oncol 23: 8331–8339.
Smid M, Wang Y, Klijn JG, Sieuwerts AM, Zhang Y, Atkins D, Martens JW, Foekens JA (2006) Genes associated with breast cancer metastatic to bone. J Clin Oncol 24: 2261–2267.
Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JGM, Foekens JA, Martens JWM (2008) Subtypes of breast cancer show preferential site of relapse. Cancer Res 68: 3108–3114.
Werkoff G, Lambaudie E, Fondrinier E, Leveque J, Marchal F, Uzan M, Barrabger E, Guillemin F, Darai E, Uzan S, Houvenaeghel G, Rouzier R, Coutant C (2009) Prospective multicenter comparison of models to predict four or more involved axillary lymph nodes in patients with breast cancer with one to three metastatic sentinel lymph nodes. J Clin Oncol 27: 5707–5712.
Wong MH, Stockler MR, Pavlakis N (2012) Bisphosphonates and other bone agents for breast cancer. Cochrane Database Syst Rev 2: CD003474.
Zhou X, Liu J (2014) A computational model to predict bone metastasis in breast cancer by integrating the dysregulated pathways. BMC Cancer 14: 6–18.
Acknowledgements
This work was supported by the Nellie B. Connally Breast Cancer Center, MD Anderson Cancer Center; La Fondation de France; and La Fondation pour la Recherche Médicale.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Delpech, Y., Bashour, S., Lousquy, R. et al. Clinical nomogram to predict bone-only metastasis in patients with early breast carcinoma. Br J Cancer 113, 1003–1009 (2015). https://doi.org/10.1038/bjc.2015.308
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.308
Keywords
This article is cited by
-
MR imaging phenotypes and features associated with pathogenic mutation to predict recurrence or metastasis in breast cancer
BMC Cancer (2023)
-
Implications for surveillance for breast cancer patients based on the internally and externally validated BRENDA-metastatic recurrence score
Breast Cancer Research and Treatment (2023)
-
Postmastectomy radiotherapy benefit in Chinese breast cancer patients with T1–T2 tumor and 1–3 positive axillary lymph nodes by molecular subtypes: an analysis of 1369 cases
Tumor Biology (2016)