Abstract
Purpose
To analyse clinical outcomes of trabeculectomy with mitomycin C (MMC) in eyes with uveitic glaucoma (UG) with inactive uveitis and compare them to those in eyes with primary open-angle glaucoma (POAG).
Design
Retrospective non-randomized comparative interventional case series.
Methods
A total of 53 eyes with UG and 80 eyes with POAG that received MMC trabeculectomy as an initial ocular surgery with average follow-up of 5.4 years were reviewed retrospectively. The intraocular pressure (IOP) control and persistence of filtering bleb were analysed using the Kaplan–Meier life-table method based on two definitions of successful IOP control, ie complete success (IOP⩽15 mm Hg without anti-glaucoma medications) and qualified success (IOP⩽15 mm Hg with topical anti-glaucoma medications). The incidences of postoperative complications were also examined.
Results
Complete success rate for postoperative IOP control at 5 years after trabeculectomy was 57.1±7.5% (mean±SE) in UG, being comparable to that in POAG (53.7±6.1%), and those of qualified success was 64.7±7.0 and 65.9±5.5% (P=0.60 and 0.53) respectively. Persistence of filtrating blebs was shorter in UG than in POAG (P=0.031). Postoperative inflammation in UG was associated with worse postoperative IOP control and loss of filtering bleb (P=0.027 and 0.021). Postoperative long-standing ocular hypotony was more frequent in UG (P=0.0063).
Conclusions
An MMC trabeculectomy for UG with inactive uveitis as an initial ocular surgery had IOP control comparable to that for POAG, suggesting that pre-existing uveitis itself is not a risk factor for failure of a filtering surgery.
Similar content being viewed by others
Introduction
Although treatment of the causative disease and medical ocular hypotensive therapy are the first choices for control of intraocular pressure (IOP) reduction in patients with uveitic glaucoma (UG), surgical therapy often becomes necessary. Trabeculectomy is the most widely used glaucoma surgery method for medically uncontrolled glaucoma,1 though pre-existing uveitis is generally considered to be one of the risk factors for failure of glaucoma filtrating surgery.2, 3, 4, 5 Recently, the results of trabeculectomy for patients with glaucoma who have a high risk for failure of filtrating surgery have been considerably improved by concomitant usage of mitomycin C (MMC),6, 7, 8 and several reports have also proposed that MMC use might improve the success rate of a trabeculectomy for UG, ranging from 50 to 90% with various criteria of success.5, 9, 10, 11, 12
However, most of the published studies of a trabeculectomy with MMC (MMC trabeculectomy) for UG have included only a clinically small number of patients or have not reported the results of long-term follow-up.5, 9, 10, 11, 12 Moreover, patients who previously received cataract or glaucoma surgery were included in those reports, though a previous ocular surgery is known to be a risk factor for trabeculectomy failure.13 Thus, to estimate the influence of pre-existing uveitis itself on the outcome of trabeculectomy procedures, it is necessary to analyse results obtained only from the eyes with inactive phase of uveitis that had no history of ocular surgery. Only two reports have analysed the outcome of MMC trabeculectomy in 27–30 UG eyes without previous ocular surgeries.11, 12 However, the average follow-up in those studies was only 2.5 and 1.9 years respectively. Thus, long-term outcomes of the initial MMC trabeculectomy in UG eyes that had no previous ocular surgery are still of clinical interest.
In the present study, we retrospectively analysed the outcomes of MMC trabeculectomy as an initial ocular surgery procedure in 53 UG eyes of 53 patients with a mean postoperative follow-up period of more than 5 years and compared the results with those of 80 eyes of 80 age-matched primary open-angle glaucoma (POAG) patients who underwent MMC trabeculectomy as an initial ocular surgery at the same period.
Materials and methods
Patients
Eyes in patients who suffered from UG refractory to medical treatment and received an MMC trabeculectomy as an initial ocular surgery at the University of Tokyo Hospital from May 1996 to November 2004 were included. Inclusion criteria were (1) uveitis was judged to be relatively controlled during the preoperative 3-month period (aqueous cellular score⩽ 1+ (0, trace or 1+)11, 14); (2) eyes had not received any kind of ocular surgery and did not undergo combined trabeculectomy and cataract or vitreo-retinal surgery; (3) eyes without neovascularizations; and (4) eyes that could be followed at least 1 year postoperatively at our clinic.
For comparison, from the database of Tokyo University Hospital, eyes in patients who suffered from POAG and received a trabeculectomy as an initial ocular surgery during the same periods (from May 1996 to November 2004) were selected. Inclusion criteria were (1) eyes had not received any kind of ocular surgery and did not undergo combined trabeculectomy and cataract or vitreo-retinal surgery, and (2) eyes that could be followed at least 1 year postoperatively at our clinic.
The following variables were analysed: age, sex, score of medication used preoperatively, preoperative IOP, postoperative IOP during the follow-up period, period of persistence of filtering bleb, and postoperative complications. Medication score (0–5, maximum score was determined as 5) was calculated by the numbers of added topical anti-glaucoma eye drops used and oral acetazolamide score (usage of oral acetazolamide at 500 mg per day or less was counted as a score of 2 and more than 500 mg per day was counted as a score of 3). As for postoperative complications, we reviewed the following major complications after MMC trabeculectomy: hyphaema, leakage from bleb, choroidal detachment, cataract progression that required operation, long-standing ocular hypotony, hypotonic maculopathy, and blebitis/endophthalmitis.
Surgical technique
Operations were performed superiorly using a limbus-based conjunctival flap and a modified Cairns technique. After dissecting a 4 × 4 mm scleral flap, intraoperative MMC (Kyowa-Hakko Co., Tokyo, Japan) was applied for 3 min using a surgical sponge soaked in 0.04% MMC solution. Thereafter, 150 ml of balanced salt solution (Alcon, Fort Worth, TX, USA) was used for washing out. A block of tissue located just anterior to the scleral spur of 1.5 × 3.0 mm wide was removed, followed by a peripheral iridectomy. The scleral flap was closed with 2–4 sutures using 10–0 nylon adjusted to allow minimal leakage during reformation of the anterior chamber. Finally, the incision of Tenon's capsule and conjunctiva was carefully closed with a 10–0 nylon running suture.
Following the operation, all patients received topical ofloxacin or levofloxacin four times a day, 0.1% betamethasone four times a day, and topical 1% atropine once a day. In seven patients (13.2%), patients with UG who had received systemic corticosteroid or immunosuppressants (cyclosporin or colchicine) preoperatively for control of the condition, those medications were continued postoperatively. Laser suture lysis was performed when an inadequate filtering bleb was noted. Digital massage was given to patients with signs of bleb encapsulation.
Follow-up and evaluation of surgical outcomes
All patients were subjected to detailed ophthalmic examinations, including best corrected-visual acuities, a Goldmann applanation tonometer, slit-lamp microscopy examination, and funduscopy. IOP values measured at three different visits just before surgery were averaged to create baseline IOP. In principle, patients were examined in detail on 1 and 3 days, and 1 and 2 weeks after surgery, and then every month for 2 years, and bimonthly during the follow-up periods after 2 years.
To evaluate IOP controls during the follow-up period, we used a Kaplan–Meier life-table, with two different definitions of successful IOP control. Complete success was defined as postoperative IOP⩽15 mm Hg without anti-glaucoma medications. Qualified success was defined as postoperative IOP ⩽15 mm Hg with use of topical anti-glaucoma drugs. Failure of IOP control was defined as postoperative IOP not meeting the above criteria at three consecutive observations, use of any anti-glaucoma medications (complete success), or the need for oral acetazolamide or additional glaucoma surgery. When a patient met either definition of failure on three consecutive visits, the first of the three visits was considered to be the time of failed IOP control. Because the results of visual field test do not always represent the stage of glaucoma in UG patients because of possible involvement of retina and/or choroid, visual field results were not factored into the failure of trabeculectomy in this study. The second needling procedure was considered a re-operation and patients who received the second needling procedure were considered to have failed.
Presence or absence of intraocular inflammation was graded by slit-lamp microscopic findings. The presence of cells and flare in the anterior chamber was scored using semi-quantitative scoring with six grades (0, trace, 1+, 2+, 3+, and 4+).14 The presence of preoperative inflammation was defined as cells or flare graded 1+ at any examination during 1 month before surgery. The presence of postoperative inflammation was defined as cells or flare graded 1+ or more at any examination from 2 weeks to 3 months after surgery. The persistence of a filtering bleb after surgery was examined by slit-lamp microscopy, and was considered to have scarred down when the filtering bleb appeared to have disappeared and could not be increased with digital massage.15
The presence of postoperative complications was examined at each clinical visit. Leakage from the bleb was tested using the Seidel test, which was routinely carried out at every visit. Long-standing ocular hypotony was defined as IOP of less than 5 mm Hg lasting more than 3 months after the first postoperative month. Hypotonic maculopathy was defined as retinal and/or choroidal folds at the posterior pole of the fundus with IOP of less than 5 mm Hg.
Statistical analysis
Evaluation of continuous variables (age, follow-up period, IOP) was achieved using two-tailed t-test. Categorical variables (sex, numbers of anti-glaucoma drugs) were evaluated with χ2-test. A Kaplan–Meier life-table was used for calculation of success rate of postoperative IOP control and persistence of the filtering bleb on both UG and POAG eyes and UG eyes with or without activity of intraocular inflammation. Comparisons of survival curves among the groups were conducted with a log-rank test. A level of P<0.05 was accepted as statistically significant. All statistical analyses were performed with SPSS for Windows version 11.0 (SPSS Inc., Chicago, IL, USA). Values are shown as the mean±SD or mean±SE.
Results
A total of 53 eyes from 53 patients (30 men, 23 women; 52.0±16.5 years old) with secondary glaucoma due to various uveitis-related conditions (preoperative mean follow-up period 1.6±1.9 years, postoperative mean follow-up period 5.5±3.0 years; range 1.0–10.4 years, median 5.6 years) were included. All patients were Japanese. Diagnoses of UG in the study subjects include Posner–Schlossmann syndrome (nine patients), Behcet's disease (seven patients), sarcoidosis (six patients), Vogt–Koyanagi–Harada disease (five patients), herpes simplex kerato-uveitis (two patients), rheumatoid arthritis (two patients), Fuchs' heterochromic iridocyclitis (one patient), ocular tuberculosis (one patient), and human T lymphotropic virus type 1-associated UG (one patient). In addition, 19 patients were diagnosed with idiopathic UG without clinical features characteristic of any recognized uveitic entities or not attributed to a specific systemic disease.
A total of 91 POAG patients who received a trabeculectomy as an initial ocular surgery during the same periods were screened. The eyes that received combined surgery with cataract operations (n=6) were excluded. To match the range of patient's age with that of UG group, we excluded the oldest five patients. Finally, 80 eyes of age-matched 80 Japanese patients (51 men and 29 women, 55.7±12.9 years old) with POAG refractory to medical treatment and received an MMC trabeculectomy as an initial ocular surgery (preoperative mean follow-up period 1.0±2.2 years, postoperative mean follow-up period 5.3±2.2 years; range 1.0–11.6 years, median 5.4 years) at the same period were included in this study. In patients who underwent bilateral filtration surgery, only the first eye was included. All eyes in both groups were operated by two surgeons (MA and SS).
Demographics of the patients are shown in Table 1. There were no significant differences in age, sex, preoperative and postoperative follow-up periods between the patients with UG and POAG (χ2-test or unpaired t-test, P=0.13, 0.41, 0.19 and 0.56 respectively). However, preoperative IOP was significantly higher in UG group (30.5±8.4 mm Hg) than POAG group (22.2±5.5 mm Hg, P<0.001, unpaired t-test), and was associated with increased numbers of preoperative anti-glaucoma drugs (4.47±0.58 vs 4.11±1.03, P=0.023, unpaired t-test). During the follow-up periods, suture lysis was performed in 32 cases (60.4%) of eyes with UG and 56 cases (70%) with POAG (P=0.25, χ2-test). Needling procedure was performed in seven cases (13.2%) of eyes with UG and nine cases (8.8%) of eyes with POAG (P=0.73, χ2-test). Needling procedure was performed twice in four eyes with POAG, whereas in none with UG. In 43 (81.1%) of the 53 eyes with UG, topical corticosteroids (0.1% dexamethasone, 29 eyes; 0.1% fluocinolone acetonide, 14 eyes) had been administered preoperatively. During the postoperative follow-up periods, cataract surgeries were performed in 15 eyes (28.3%) with UG and 11 eyes (13.8%) with POAG, and penetrating keratoplasty was performed in 2 eyes with UG.
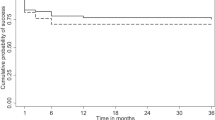
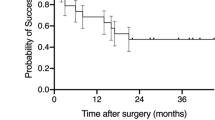
Figures 1 and 2 show the survival curves based on the two definitions of failed postoperative IOP control. The probability of complete success (Figure 1) at 5 years after surgery was 57.1±7.5% (mean±SE) in eyes with UG and 53.7±6.1% in eyes with POAG, respectively, whereas that of qualified success (Figure 2) was 64.7±7.0 and 65.9±5.5% respectively. In both definitions of failed postoperative IOP control, there were no significant differences in estimated success probability between the two groups (P=0.60 and 0.53, respectively, log-rank test).
Kaplan–Meier curves for successful intraocular pressure (IOP) control by trabeculectomy with mitomycin C in the patients with uveitic glaucoma (UG, broken line) and primary open-angle glaucoma (POAG, solid line). Definition of success of IOP control was IOP⩽15 mm Hg without anti-glaucoma medications (complete success). Probability of complete success at 5 years was 57.1±7.5% in eyes with UG and 53.7±6.1% in eyes with POAG (P=0.60, log-rank test). The number of the patients who could be followed-up at 5 years after trabeculectomy was 32 (60.4%) in UG and 47 (58.8%) in POAG, and those at 8 years was 11 (20.8%) in UG and 9 (11.3%) in POAG.
Kaplan–Meier curves for successful intraocular pressure (IOP) control by trabeculectomy with mitomycin C in the patients with uveitic glaucoma (UG, broken line) and primary open-angle glaucoma (POAG, solid line). Definition of success of IOP control was IOP⩽15 mm Hg with topical anti-glaucoma medications (qualified success). Probability of qualified success at 5 years was 64.7±7.0% in UG and 65.9±5.5% in POAG (P=0.53, log-rank test).
The estimate of bleb survival rate at 5 years after surgery was 59.1±7.6% in eyes with UG and 72.0±5.3% in eyes with POAG (Figure 3). The survival of filtering bleb was significantly shorter in the patients with UG than those with POAG (P=0.031, log-rank test).
Kaplan–Meier curves for survival of persistence of filtering bleb after trabeculectomy with mitomycin C in the patients with uveitic glaucoma (UG, broken line) and primary open-angle glaucoma (POAG, solid line). The estimate of bleb survival rate at 5 years after surgery was 59.1±7.6% in UG and 72.0±5.3% in POAG (P=0.031, log-rank test).
To elucidate the influence of preoperative and postoperative activities of intraocular inflammation on the successful IOP control by an MMC trabeculectomy, we divided eyes with UG into two groups according to the presence or absence of preoperative (n=15 with preoperative aqueous cell score of 1+ and 38 with preoperative score of 0 or trace respectively) or postoperative (n=23 and 30 respectively) inflammation. There were no significant differences in probability of complete success and qualified success between the groups with and without preoperative inflammation (data not shown; P=0.92 and 0.70, log-rank test), whereas significant differences were found in the probability of complete and qualified success rates between the groups with and without postoperative inflammation (P=0.027, Figure 4 and P=0.083, data not shown, log-rank test). Moreover, by comparing the persistence of filtering bleb between the patients of with and without postoperative inflammation, it was found that postoperative inflammation significantly worsened the survival of filtering blebs (Figure 5; P=0.021, log-rank test).
Presence or absence of postoperative intraocular inflammation and Kaplan–Meier curves for successful intraocular pressure (IOP) control by trabeculectomy with mitomycin C in the patients with uveitic glaucoma. Definition of success of IOP control was IOP⩽15 mm Hg without topical anti-glaucoma medications (complete success). There was a significant difference in the probability of success rate between the patients with postoperative inflammation (n=23, broken line) and those without postoperative inflammation (n=30, solid line) (P=0.027, log-rank test).
Presence or absence of postoperative intraocular inflammation and Kaplan–Meier curves for survival of persistence of filtering bleb after trabeculectomy with mitomycin C in the patients with uveitic glaucoma. There was a significant difference in the probability of bleb survival between the patients with postoperative inflammation (n=23, broken line) and those without postoperative inflammation (n=30, solid line) (P=0.021, log-rank test).
The incidences of postoperative complications in eyes with UG and POAG were as follows: hyphaema (24.5 and 17.5%, P=0.32, χ2-test), leakage from bleb during the follow-up (7.5 and 12.5%, P=0.53), long-standing ocular hypotony (28.3 and 10.0%, P=0.0063), hypotonic maculopathy (15.1 and 3.8%, P=0.018), and cataract progression that required operation (28.3 and 13.8%, P=0.038). Twelve eyes (22.6%) with UG and 18 eyes (22.5%) with POAG were complicated with choroidal detachments in the early postoperative period (P=0.98). In the cases with choroidal detachments, two eyes with UG (16.7%) and two eyes (11.1%) with POAG required surgical intervention (transscleral drainage). None of the present patients were complicated with blebitis or endophthalmitis.
Conclusion
In the present study, we analysed the postoperative outcomes of 53 UG eyes of 53 patients with inactive uveitis that had no previous ocular surgeries and received an initial MMC trabeculectomy, with a mean postoperative follow-up of 5.5 years. This study included the largest series of UG patients without any previous ocular surgeries with the longest follow-up reported. The probability of complete success of IOP control (IOP⩽15 mm Hg without anti-glaucoma medications) and qualified success of IOP control (IOP⩽15 mm Hg with topical anti-glaucoma medications) was 57.1±7.5 and 64.7±7.0%, respectively, at 5 years.
Prata et al9 reported that the probability of successful IOP control was 75% at 20 months for an MMC trabeculectomy in eyes with UG, when the target IOP was set at 21 mm Hg or less, whereas Wright et al10 reported the probability of 58% at 1.5 years using the same success criteria. Noble et al5 recently reported that the probability of successful IOP control was 79% at 2 years, when the target IOP reduction was 30% or more with glaucoma mediation. These reports included patients who had a history of prior ocular surgeries, which is one of the important risk factors for trabeculectomy failure.13 Ceballos et al11 analysed the outcomes of MMC trabeculectomy in UG eyes that had previously received ocular surgery (14 eyes) and those without previous surgery (30 eyes), with an average postoperative follow-up period of 2.5 years. They reported that the probability of successful IOP control in eyes with and without previous surgery was 70 and 58%, respectively, after 2 years, when the target IOP was set at 21 mm Hg or less. There were no significant differences between two groups. Imaizumi et al12 treated 27 eyes with UG that had no previous ocular surgery by an initial MMC trabeculectomy (average postoperative follow-up, 1.9 years) and reported that the probability of success was 76% after 5 years, when the target IOP was set at 21 mm Hg or less. If the target IOP was set at 21 mm Hg or less in the current cases, the probability of successful IOP control was calculated to be 84.0±5.2% at 2 years and 79.1±6.0% at 5 years, respectively, which is favourable compared to the previous reports.
In the current study, we also retrospectively compared the outcomes of the initial MMC trabeculectomy in UG eyes with those of the age- and sex-matched POAG eyes being operated at the same period, and found that probability of successful IOP control was similar between the current UG and POAG eyes (57.1±7.5 and 53.7±6.1% at 5 years for the probability of complete success and 64.7±7.0 and 65.9±5.5% at 5 years for the probability of qualified success). Several reports regarding long-term outcome of the initial MMC trabeculectomy in eyes with POAG have been published. In a recent study by Fontana et al,16 the probability of successful IOP control was 62±4% after 5 years for that procedure in 292 eyes of 225 phakic patients with open-angle glaucoma that had no previous ocular surgeries, when the target IOP was 18 mm Hg or less and the target IOP reduction was 20% or more. Moreover, Kim et al17 performed primary trabeculectomy with MMC (3–5 min at a concentration of 0.5 mg/ml) in 38 phakic POAG patients and reported that the probability of successful IOP control was approximately 75% at 3 years after the surgeries, when the target IOP was set at 21 mm Hg or less. Shigeeda et al18 reported that the probability of successful IOP control following MMC trabeculectomy in Japanese POAG patients with no previous ocular surgery was 71.3±4.1% after 5 years, when the target IOP was 18 mm Hg or less. If the target IOP was set at 18 mm Hg or less in the POAG cases in the current study, the probability of successful IOP control for the initial MMC trabeculectomy was calculated to be 82.4±4.3% at 2 years and 74.1±5.3% at 5 years for qualified success (with topical anti-glaucoma medications), respectively, which was comparable to those reported for the initial MMC trabeculectomy in phakic eyes with POAG in the United States16, 17 or Japan.18
Thus, our results suggested that pre-existing uveitis itself is not a significant risk factor for the failure of trabeculectomy, when the uveitis was controlled at the time of surgery and the procedure was performed as an initial surgery and with MMC. Long-term preoperative topical corticosteroid usage for UG may be at least partly responsible for the current rather unexpected results, because topical corticosteroid can reduce the numbers of fibroblasts and macrophages in the conjunctiva,19 and, in the same manner, long-term postoperative use of topical corticosteroid in eyes with UG to control uveitis might also have favourable impact on the success rate of trabeculectomy.20
Regarding the appearance of a filtering bleb, the current study suggested that the blebs in the current UG patients lost their appearance more rapidly compared with POAG patients (Figure 3). However, success rates of postoperative IOP control in the current UG and POAG were comparable (Figures 1 and 2). Indeed, we sometimes experienced UG eyes with low postoperative IOP without apparently functioning filtering bleb after trabeculectomy. Reduced aqueous production in chronic uveitis patients21 and/or high levels of intrinsic prostaglandins in aqueous humor of uveitic eyes might be at least partly responsible for the above finding.
We are also interested in the influence of postoperative intraocular inflammation on the success rate of MMC trabeculectomy in UG patients. One retrospective study of trabeculectomy procedures without anti-proliferative agents in eyes with UG suggested that surgical success was dependant on postoperative inflammation, but not on inflammation at the time of surgery.22 In the present study, the presence of low-grade intraocular inflammation at the time of surgery showed little influence on the probability of successful IOP control (data not shown), whereas the presence of postoperative inflammation between 2 weeks and 3 months after surgery significantly worsened the probability of successful IOP control (Figure 4). The present findings also showed that postoperative intraocular inflammation reduced the probability of persistence of the filtering bleb (Figure 5). Failure of filtration surgery is believed to be mainly due to conjunctival fibroblast proliferation, collagen synthesis, and subconjunctival fibrosis.23 Because many kinds of inflammatory cytokines could become chemoattractants or activators of fibroblasts, they have the possibility of accelerating subconjunctival fibrosis after trabeculectomy.23 In fact, a number of fibroblasts and inflammatory leucocytes, such as lymphocytes and macrophages, were observed in the conjunctiva in the area of filtering blebs in UG patients after a trabeculectomy.24 Thus, our results suggest the importance of suppressing inflammation postoperatively for a better outcome of trabeculectomy in eyes with UG.
Because many eyes with UG are already associated with damage by inflammation before surgery, they are expected to have a higher complication rate than eyes with POAG.10 Ceballos et al11 reported that the most common complication after an MMC trabeculectomy in UG was transient worsening of intraocular inflammation (27%), followed by serous choroidal detachment (21%), a shallow or flat anterior chamber (16%), transient hyphaema (11%), and hypotony maculopathy (7%). Although the incidence of hypotonic maculopathy was rather high (15.1%) in our UG cases, the incidences of the other postoperative complications in the current UG eyes were comparable with those of previous reports.11, 12 In addition, the current study demonstrated a higher incidence of postoperative cataract progression, hypotonic maculopathy, and long-standing hypotony in eyes with UG than the eyes with POAG . Cataract progression might be accelerated by longer history of intraocular inflammation and longer topical corticosteroid use in eyes with UG. Hypotonic maculopathy and long-standing hypotony in eyes with UG might be partly attributed to the reduced aqueous production associated with uveitis.21
In conclusion, although our study has limitations that are common to retrospective investigations, our results demonstrated that an initial trabeculectomy with MMC for UG eyes with inactive uveitis that had no previous ocular surgeries had outcomes comparable to that for POAG eyes, suggesting that the pre-existing uveitis itself is not a significant risk factor for the failure of a trabeculectomy with MMC when the uveitis was under control. However, a decrease in the success rate of IOP control and persistence of the filtering bleb were found to be associated with the presence of postoperative intraocular inflammation in eyes with UG.
References
Katz LJ, Costa VP, Spaeth GL . Filtration surgery. In: Ritch R, Shields MB, Krupin T (eds). The Glaucomas, 2nd edn. Mosby: St Louis, 1996, pp 1661–1702.
Krupin T, Feitl ME, Karalekas D . Glaucoma associated with uveitis. In: Ritch R, Shields MB, Krupin T (eds). The Glaucomas, 2nd edn. Mosby: St Louis, 1996, pp 1225–1257.
Kanski JJ, Shun-Shin GA . Systemic uveitis syndromes in childhood: an analysis of 340 cases. Ophthalmology 1984; 91: 1247–1252.
Panek WC, Holland GN, Lee DA, Christensen RE . Glaucoma in patients with uveitis. Br J Ophthalmol 1990; 74: 223–227.
Noble J, Derzko-Dzulynsky L, Rabinovitch T, Birt C . Outcome of trabeculectomy with intraoperative mitomycin C for uveitic glaucoma. Can J Ophthalmol 2007; 42: 89–94.
Kitazawa Y, Kawase Y, Matsushita H, Minobe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch Ophthalmol 1991; 109: 1693–1698.
Cheung JC, Wright MN, Murali S, Pederson JE . Intermediate-term outcome of variable dose mitomycin C filtering surgery. Ophthalmology 1997; 104: 143–149.
Perkins TW, Gangnon R, Ladd W, Kaufman PL, Heatley GA . Trabeculectomy with mitomycin C: intermediate-term results. J Glaucoma 1998; 7: 230–236.
Prata Jr JA, Neves RA, Minckler DS, Mermoud A, Heuer DK . Trabeculectomy with mitomycin C in glaucoma associated with uveitis. Ophthalmic Surg 1994; 25: 616–620.
Wright MM, McGehee RF, Pederson JE . Intraoperative mitomycin-C for glaucoma associated with ocular inflammation. Ophthalmic Surg Lasers 1997; 28: 370–376.
Ceballos EM, Beck AD, Lynn MJ . Trabeculectomy with antiproliferative agents in uveitic glaucoma. J Glaucoma 2002; 11: 189–196.
Imaizumi Y, Kurita M, Sugita M, Saito H, Ohno S . Outcome of trabeculectomy with adjunctive mitomycin C in uveitic glaucoma. Rinsho Ganka (Jpn J Clin Ophthalmol) 2001; 55: 359–363.
Liebmann JM, Ritch R . Complications of glaucoma filtrating surgery. in: Ritch R, Shields MB, Krupin T (eds). The Glaucomas, 2nd edn. Mosby: St Louis, 1996, pp 1703–1735.
Nussenblatt RB, Whitcup SM, Palenstine AG . Examination of the patients with uveitis. in: Nussenblatt RB, Whitcup SM, Palenstine AG (eds). Uveitis Fundamental and Clinical Practice, 2nd edn. Mosby: St Louis, 1996, pp 58–68.
Hu CY, Matsuo H, Tomita G, Suzuki Y, Araie M, Shirato S et al. Clinical characteristics and leakage of functioning blebs after trabeculectomy with mitomycin-C in primary glaucoma patients. Ophthalmology 2003; 110: 345–352.
Fontana H, Nouri-Mahdavi K, Lumba J, Ralli M, Caprioli J . Trabeculectomy with mitomycin C: outcomes and risk factors for failure in phakic open-angle glaucoma. Ophthalmology 2006; 113: 930–936.
Kim YY, Sexton RM, Shin DH, Kim C, Ginde SA, Ren J et al. Outcomes of primary phakic trabeculectomies without versus with 0.5–1-min versus 3–5-min mitomycin C. Am J Ophthalmol 1998; 126: 755–762.
Shigeeda T, Tomidokoro A, Chen YN, Shirato S, Araie M . Long-term follow-up of initial trabeculectomy with mitomycin C for primary open-angle glaucoma in Japanese patients. J Glaucoma 2006; 15: 195–199.
Akyol N, Demir T, Kukner A, Colakoglu N . Effects of systemic octreotide, local mytomycine-C and local corticosteroids on wound-healing reaction after glaucoma surgery. Int Ophthalmol 2001; 24: 235–241.
Starita RJ, Fellman RL, Spaeth GL, Poryzees EM, Greenidge KC, Traverso CE . Short- and long-term effects of postoperative corticosteroids on trabeculectomy. Ophthalmology 1985; 92: 938–946.
Toris CB, Pederson JE . Aqueous humor dynamics in experimental iridocyclitis. Invest Ophthalmol Vis Sci 1987; 28: 477–481.
Miyata H, Ando Y, Suzuki S, Kamizono J . Surgical result of glaucoma secondary to uveitis. Ganka Shujutsu (Jpn J Ophthalmic Surg) 1991; 4: 711–715.
Skuta GL, Parrish II RK . Wound healing in glaucoma filtering surgery. Surv Ophthalmol 1987; 32: 149–170.
Broadway DC, Bates AK, Lightman SL, Grierson I, Hitchings RA . The importance of cellular changes in the conjunctiva of patients with uveitic glaucoma undergoing trabeculectomy. Eye 1993; 7: 495–501.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaburaki, T., Koshino, T., Kawashima, H. et al. Initial trabeculectomy with mitomycin C in eyes with uveitic glaucoma with inactive uveitis. Eye 23, 1509–1517 (2009). https://doi.org/10.1038/eye.2009.117
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.117
Keywords
This article is cited by
-
Preserflo microshunt implant for the treatment of refractory uveitic glaucoma: 36-month outcomes
Eye (2023)
-
Long-term outcomes of initial trabeculectomy in glaucoma associated with granulomatous and non-granulomatous uveitis
International Ophthalmology (2021)
-
Evaluation of the outcome of long-tube shunt implant surgery in uveitic glaucoma patients by analyzing the background of uveitis
International Ophthalmology (2021)
-
The influence of mitomycin C concentration on the outcome of trabeculectomy in uveitic glaucoma
International Ophthalmology (2018)
-
Deep sclerectomy for uveitic glaucoma: long-term outcomes
Eye (2017)